Abstract
OBJECTIVE
To explore whether general practitioners who request spinal x-ray investigations are less likely to refer, prescribe medication, or order additional tests when they intend only to reassure patients rather than to exclude or confirm disease.
DESIGN
Cross-sectional survey. Physicians recorded reasons for requesting x-ray examinations and differential diagnoses on the request form. When they received a radiologist’s report on a spinal x-ray test, GPs also received a questionnaire on their subsequent management.
SETTING
Maastricht region of the Netherlands.
PARTICIPANTS
All 90 GPs in the Maastricht region who referred patients for spinal x-ray examinations during 19 consecutive weeks.
MAIN OUTCOME MEASURES
Reason for requesting spinal x-ray investigations, results, and subsequent management.
RESULTS
We received completed questionnaires on 386 patient contacts. Physicians were significantly less likely to refer, prescribe medication, or order additional tests when they intended only to reassure patients rather than to exclude or confirm disease (odds ratio 0.3, 95% confidence interval 0.1 to 0.6). This effect was independent of the results of the x-ray examinations.
CONCLUSION
Physicians seem to be aware that they have requested spinal x-ray examinations only to reassure patients, and they account for this in their management. These findings support debate on the negative consequences of requesting tests for other than purely medical reasons. Concerns about unjustified actions based on the results of x-ray examinations that were requested primarily to reassure patients should probably have only a minor role in the debate about unnecessary testing.
Abstract
OBJECTIF
Vérifier si les omnipraticiens qui prescrivent des radiographies du rachis ont moins de chance de demander des consultations, prescrire des médicaments ou demander des examens additionnels lorsqu’ils cherchent seulement à rassurer les patients plutôt qu’à exclure ou confirmer une maladie.
TYPE D’ÉTUDE
Enquête transversale. Les médecins devaient inscrire sur la prescription les raisons de la demande de radiographie du rachis et de diagnostic différentiel. À la réception du rapport du radiologiste, ils recevaient un questionnaire sur les gestes thérapeutiques à venir.
CONTEXTE
La région de Maastricht en Hollande.
PARTICIPANTS
Les 90 omnipraticiens de la région de Maastricht qui ont adressé des patients pour un examen radiologique du rachis durant 19 semaines consécutives.
PRINCIPAUX PARAMÈTRES ÉTUDIÉS
Motifs des demandes d’examen radiologique du rachis, résultats et traitement subséquent.
RÉSULTATS
Des questionnaires complétés ont été reçus pour 386 cas. Les médecins étaient significativement moins susceptibles de demander une consultation, prescrire un médicament ou demander des examens additionnels lorsqu’ils cherchaient seulement à rassurer les patients plutôt qu’à exclure ou confirmer une maladie (rapport de cote: 0,3; intervalle de confiance à 95%: 0,1 à 0,6). Cet effet était indépendant du résultats de la radiographie.
CONCLUSION
Il semble que les médecins sont conscients d’avoir prescrit des examens radiologiques du rachis uniquement pour rassurer les patients et ils en tiennent compte dans leur façon de faire. Ces résultats alimentent le débat sur les conséquences négatives des demandes de tests pour des raisons autres que purement médicales. Les préoccupations concernant les actions non justifiées entreprises à partir de résultats d’examens radiologiques demandés principalement pour rassurer le patient ne devraient jouer qu’un rôle mineur dans le débat sur les examens inutiles.
EDITOR’S KEY POINTS.
Despite evidence-based guidelines describing the limited usefulness of spinal x-ray films for diagnosis or therapy (up to 50% of requests for lumbar spine radiography could be unnecessary), general practitioners continue to request them.
The consequences of GPs’ requesting investigations only to reassure patients could be severe if subsequent unexpected abnormal results lead to unjustified additional investigations to search for causes of the initial abnormalities.
This study tests the hypothesis that, when GPs request spinal x-ray examinations, they are less likely to pursue active management if they intend only to reassure patients than if they intend to exclude or confirm disease. Results confirmed the hypothesis and showed that GPs take their reasons for requesting x-ray tests into account when deciding on management.
The authors concluded that concerns about unjustified active management should probably have only a minor role in the debate about requesting unnecessary tests.
POINTS DE REPÈRE DU RÉDACTEUR.
Malgré certaines directives fondées sur des preuves indiquant que les radiographies du rachis ont une utilité limitée pour le diagnostic ou le traitement (jusqu’à 50% des demandes de radiographie pour la colonne lombaire seraient non nécessaires), les omnipraticiens continuent d’en prescrire.
Le fait que les médecins prescrivent des examens uniquement pour rassurer les patients pourrait avoir des conséquences graves si un résultat anormal inattendu entraînait des examens additionnels non justifiés pour trouver les causes des anomalies initiales.
Cette étude voulait vérifier l’hypothèse selon laquelle lorsqu’un médecin prescrit un examen radiologique du rachis, il est moins susceptible de poursuivre un traitement actif s’il vise seulement à rassurer le patient plutôt qu’à exclure ou confirmer une maladie. Les résultats ont confirmé l’hypothèse et montré que les médecins tiennent compte de leurs raisons de demander des examens radiologiques lorsqu’il décident des actions à prendre.
Les auteurs concluent que les préoccupations au sujet des traitements actifs non justifiés ne joueront probablement qu’un rôle mineur dans le débat sur la prescription d’examens non nécessaires.
Imaging of the cervical, thoracic, or lumbar spine is frequently ordered in general practice.1 Despite evidence-based guidelines on the usefulness of spinal x-ray films for diagnosis or therapy, GPs continue to request them contrary to recommendations.1-4 Up to 50% of requests for lumbar spine radiography could be unnecessary according to clinical guidelines.5-7 Several studies showed that GPs have many reasons for these requests; reassuring patients is apparently particularly important grounds for such requests.8,9
It is important to know the effect of requesting spinal x-ray films on GPs’ management. If they request the tests, their management might be guided mainly by the results. This is important because experts on medical decision making warn that, in interpreting test results, it is essential to look not only at the results themselves but also at GPs’ estimate of disease probability.10 If disease probability is not included in interpreting results, the importance of abnormal findings could be overestimated.11 There have been case reports of GPs’ requesting laboratory investigations to reassure patients and receiving unexpected abnormal results that led to unjustified additional tests to search for the causes of the abnormalities.12,13 When requesting spinal x-ray films in daily practice, the very fact that GPs intend only to reassure might increase their reluctance to prescribe medication or refer patients, regardless of the results. Such reluctance might be caused by lack of interest in the results or by a perceived incongruence between clinical symptoms and x-ray findings.14
Although the intention to reassure patients might be expected to affect GPs’ management, there is hardly any evidence supporting such an expectation. This study tested the hypothesis that, when they request spinal x-ray films, GPs are less likely to pursue active management (referral to specialists, prescribing medication, physical therapy, or additional investigations) when they intend only to reassure patients rather than to exclude or confirm disease.
METHODS
Study design
We conducted a cross-sectional survey of all 90 GPs in the region around the Dutch town of Maastricht. The GP population in this region does not differ substantially from the overall population of GPs in the Netherlands.15 In this region, GPs order tests without referring patients to outpatient clinics and without having to consult specialists. All requests are handled by the Diagnostic Centre at the Maastricht University Hospital. X-ray films are seen and interpreted by hospital radiologists, and reports are sent to the GPs who requested the examinations.
Data collection
To ensure that data collection would be feasible and not put undue strain on GPs, we chose one specific, infrequently ordered test: x-ray examination of the lumbar, thoracic, or cervical parts of the spine. All requests for such tests ordered during 19 consecutive weeks were selected. Physicians were already in the habit of recording the reason for their requests and the differential diagnoses on the request forms. When results were returned to GPs, a 1-page inquiry was attached. It contained the question, “What was your management after you received the result of the x-ray test?” Physicians were asked to tick off any management maneuvers they had used and to add comments. The questionnaire had been pilot-tested in 2 practices. Telephone calls were used to remind GPs to complete and return the forms. Maastricht University’s Medical Ethics Review Committee approved the study.
Variables
Physicians’ decision to pursue active management was the dependent variable. Active management was defined as starting or changing medication, repeat testing, offering physical therapy, or consulting a specialist. Physical therapy included physiotherapy, exercise therapy, and manual therapy. The reason for the request for spinal x-ray films was the independent variable. It was classified into 5 categories: to exclude disease, to confirm disease, for follow-up, to reassure a patient, and requested by a health professional other than GP. The category “to reassure a patient” included physicians’ requests and x-ray films ordered at patients’ request.
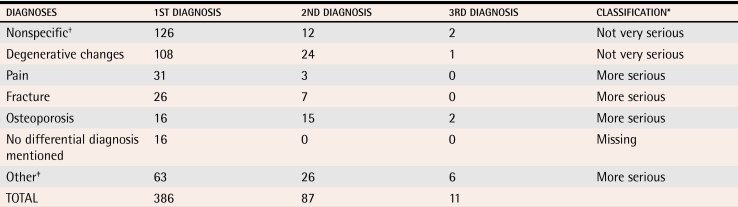
We regarded the results of x-ray examinations as a confounder and corrected for their influence on management in the analysis. Results were classified into 3 categories by 3 of the authors using radiologists’ reports: normal (no abnormalities mentioned), minor degenerative changes (minor degenerative changes and minor scoliosis or kyphosis), and abnormal (eg, appreciable degenerative changes, fractures, or osteoporosis) (Table 1). We also regarded the differential diagnosis as a confounder. It was coded into 2 categories: less serious and more serious. Coding was done by 2 of the authors. Patients’ age and sex were also considered as potential confounders in the analysis.
Table 1.
Differential diagnoses mentioned on request forms
*If at least 1 of the 3 differential diagnoses was a more serious diagnosis, the differential diagnosis variable was coded as more serious.
†The GP mentioned no differential diagnoses but asked for abnormalities (eg, pathology, bone abnormalities, or musculoskeletal disease).
‡All other diagnoses (eg, spondylolisthesis or radicular syndrome).
Analysis
Analysis was done using SPSS 11.0 for Windows. Descriptive cross-tabulations were used to analyze the influence of the reason for the request and the test result on decisions about management. Chi-square tests were performed to calculate significant differences. Variables were checked for multicolinearity. Multiple logistic regression analysis, using the enter method, was used to compare the categories “to confirm disease” and “to reassure a patient” from the variable “reason for request” with the category “to exclude disease.” The categories “for follow-up” and “request by a health professional other than GP” were omitted from the analysis (25 cases). Cases with missing data were included in the analysis. The product of the variables “reason for request” and “result” was included in the initial model to test for effect modification. It turned out not to be significant and was omitted from the final analysis.
RESULTS
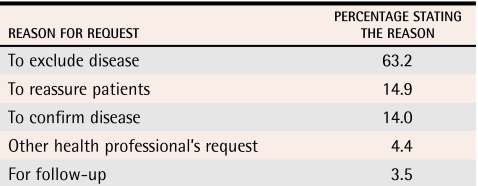
All 90 GPs associated with the Diagnostic Centre requested x-ray tests during the study period. Among the 98% of questionnaires (n = 386) returned, 58% involved female patients, 22% involved patients older than 65 years, and 33% involved patients younger than 40 years. The most frequently missing item among the responses was the reason for requesting x-ray investigation (Table 2). In descending order, 63% of x-ray tests were requested to exclude disease, 15% to reassure a patient, and 14% to confirm disease. More than 70% of the differential diagnoses mentioned on the request forms concerned disorders that were not serious. As to the results, 137 (36%) were normal, 185 (48%) showed minor degenerative changes, and 64 (17%) were abnormal.
Table 2. Reasons for requesting spinal x-ray films.
n = 315, 71 responses missing.
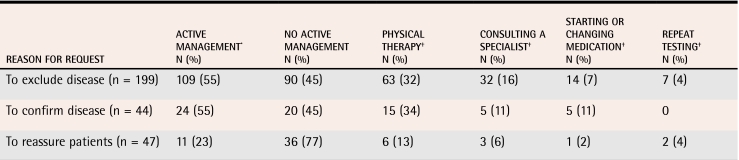
Table 3 shows the relation between reasons for requests and management by GPs. X-ray investigations requested only to reassure patients led to active management of 11 patients (23%). This was fewer than the corresponding number of patients actively managed when x-ray tests were requested to exclude (109, 55%) or to confirm (24, 55%) disease (P <.001).
Table 3. Reasons for requesting x-ray films and management decisions.
P <.001, 2 degrees of freedom.
*Active management includes physical therapy, consulting specialists, starting or changing medication, and repeat testing. Because GPs could choose more than 1 item per patient, the sum of these items might exceed the number of patients actively managed.
†Not tested for significance.
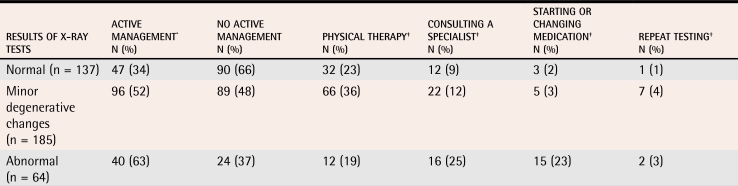
Results were regarded as a confounder in this study, but they also influenced management (Table 4). Active management was more likely to be pursued (P <.001) when results showed minor degenerative changes (52%) or were abnormal (63%) than when they were normal (34%). Results showing minor degenerative changes were more likely to lead to referrals for physical therapy than abnormal or normal results were.
Table 4. Test results and management decisions.
P <.001, 2 degrees of freedom.
*Active management includes physical therapy, consulting specialists, starting or changing medication, and repeat testing. Because GPs could choose more than 1 item per patient, the sum of these items might exceed the number of patients actively managed.
†Not tested for significance.
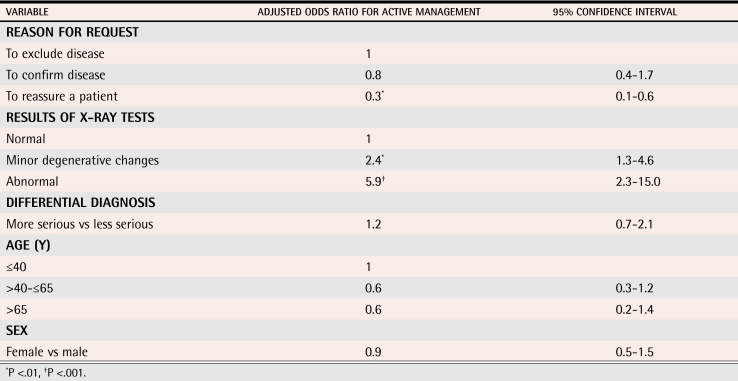
Table 5 shows the results of multiple logistic regression analysis. The GPs were significantly less likely to pursue active management (odds ratio [OR] 0.3, 95% confidence interval [CI] 0.1 to 0.6) when they had intended to reassure a patient than when they had intended to exclude disease. Requests intended to confirm disease had the same influence as those intended to exclude disease. This effect on management was independent of x-ray results. Results were the only confounder that also had an independent influence on management. When results showed minor degenerative changes, active management was 2.4 times more likely (95% CI 1.3 to 4.6) than when results were normal. Active management was 5.9 times more likely (95% CI 2.3-15.0) when results were abnormal.
Table 5. Multiple logistic regression analysis.
N = 281; 80 cases were missing, and 25 cases were excluded.
DISCUSSION
Summary of main findings
Results of this study confirmed our hypothesis: when spinal x-ray investigations were requested with the intention of reassuring patients, the adjusted OR (ie, irrespective of the result) for pursuing active management was 0.3 compared with when tests were ordered to exclude disease. Apparently then, GPs’ decisions to pursue active management are influenced by the reasons for requests.
Strengths and limitations of the study
As far as we know, this is the first study to determine the influence on GPs’ routine management of ordering spinal x-ray investigations with the intention of reassuring patients. The strength of this study is that it provides insight into the way in which requests that are probably not in accordance with evidence-based guidelines influence management. It appears that, even when results are abnormal, GPs are less likely to pursue active management when the intent was to reassure patients. We think, therefore, that the results of this study are valuable for those seeking to improve the requesting of spinal x-ray tests.
The limitations of cross-sectional designs are generally known. For our results, these limitations mean that, although we found a relation between the reasons for requesting the tests and subsequent management, we cannot prove a causative relationship.
The response rate was surprisingly high. This might be explained by the existing close cooperation between the GPs and the Diagnostic Centre. Physicians in Maastricht have attended several training sessions on test ordering organized by the Diagnostic Centre and are accustomed to speak openly with colleagues about requesting diagnostic tests.
We recognize that other variables influence complex decision processes like management choice, such as patients’ symptoms, pain, or worries. Because assessing such symptoms would have taken a great deal of time and effort from participating GPs, we chose to focus on the few variables that we regarded as key determinants of management. Future studies could explore the role of other variables that might confound the relation between reasons for requests and management.
Comparison with other studies
Results of x-ray tests were in accordance with those found in other primary care studies. In a randomized controlled trial, results of lumbar spine x-ray tests showed no abnormalities in 31% of patients.16 In another study, 37% of radiologic findings on lumbar x-ray films were normal, and 36% showed minor changes.5 These results are roughly comparable with our results.
A study in a Dutch population reported that x-ray investigations were ordered at patients’ request or for reassurance in 38% of cases.17 Little and colleagues6 found that 28% of all requests were made for psychosocial reasons. We found only 14.9% of requests were made to reassure. We recorded only the primary reason, however, while the other studies recorded secondary reasons also. Reassurance is often a secondary reason, and our figure of almost 15% would probably have been higher if secondary reasons had been taken into account.
Implications for future research and clinical practice
Many requests for spinal x-ray films are intended to reassure patients, and there could be concerns about unjustified active management after results are received. Our study found that GPs take their reason for requesting x-ray films into account when deciding on management. Therefore, concerns about unjustified active management should probably play only a minor role in the debate about requesting unnecessary tests.
Nevertheless, there are still many reasons to encourage GPs to adhere closely to national guidelines on requesting spinal x-ray investigations. For example, patients with low back pain who undergo x-ray tests for reassurance are more likely to consult their GPs in the subsequent months.16
Conclusion
Up to 50% of all requests for lumbar spine radiography could be unnecessary according to clinical guidelines. While reassuring patients is an important motive for requesting spinal x-ray tests, we did not know how such requests influenced further management. This study shows that, when GPs request spinal radiography to reassure patients, active management, such as prescribing medication and referral to specialists or physical therapy, is about 3 times less likely (P <.01) than when they request radiography to confirm or exclude disease. This effect was found regardless of results.
Apparently, GPs take their reasons for requesting radiography into account when deciding on active management. This study increases our insight into the consequences of requesting tests for other than purely medical reasons and thus provides valuable information to those involved in improving physicians’ use of radiographic services.
Levels of evidence.
Level I: At least one properly conducted randomized controlled trial, systematic review, or meta-analysis
Level II: Other comparison trials, non-randomized, cohort, case-control, or epidemiologic studies, and preferably more than one study
Level III: Expert opinion or consensus statements
Biographies
Dr Houben is a junior researcher and a general practitioner in the Centre for Quality of Care Research and the Department of General Practice at Maastricht University in the Netherlands.
Dr van der Weijden is an epidemiologist in the Centre for Quality of Care Research and the Department of General Practice at Maastricht University.
Ms Sijbrandij is a statistical analyst and epidemiologist in the Centre for Data and Information Management at Maastricht University.
Dr Grol is a Professor of General Practice and Coordinator of the Centre for Quality of Care Research.
Dr Winkens is a general practitioner in the Centre for Quality of Care Research and the Integrated Care Unit at the University Hospital in Maastricht.
Footnotes
Competing interests: None declared
References
- 1.Oakeshott P, Kerry SM, Williams JE. Randomized controlled trial of the effect of the Royal College of Radiologists’ guidelines on general practitioners’ referrals for radiographic examination. Br J Gen Pract. 1994;44:197–200. [PMC free article] [PubMed] [Google Scholar]
- 2.Royal College of Radiologists Working Party. Influence of Royal College of Radiologists’ guidelines on referral from general practice. BMJ. 1993;306:110–111. doi: 10.1136/bmj.306.6870.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Vos Meiring P, Wells IP. The effect of radiology guidelines for general practitioners in Plymouth. Clin Radiol. 1990;42:327–329. doi: 10.1016/s0009-9260(05)82146-4. [DOI] [PubMed] [Google Scholar]
- 4.Grimshaw JM, Russell IT. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet. 1993;342:1317–1322. doi: 10.1016/0140-6736(93)92244-n. [DOI] [PubMed] [Google Scholar]
- 5.Halpin SF, Yeoman L, Dundas DD. Radiographic examination of the lumbar spine in a community hospital: an audit of current practice. BMJ. 1991;303:813–815. doi: 10.1136/bmj.303.6806.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Little P, Cantrell T, Roberts L, Chapman J, Langridge J, Pickering R. Why do GPs perform investigations? The medical and social agendas in arranging back X-rays. Fam Pract. 1998;15:264–265. doi: 10.1093/fampra/15.3.264. [DOI] [PubMed] [Google Scholar]
- 7.Van Boven K, Dijksterhuis P, Lamberts H. Defensive testing in Dutch family practice. Is the grass greener on the other side of the ocean? J Fam Pract. 1997;44:468–472. [PubMed] [Google Scholar]
- 8.Espeland A, Baerheim A, Albrektsen G, Korsbrekke K, Larsen JL. Patients’ views on importance and usefulness of plain radiography for low back pain. Spine. 2001;26:1356–1363. doi: 10.1097/00007632-200106150-00020. [DOI] [PubMed] [Google Scholar]
- 9.Van der Weijden T, Van Bokhoven MA, Dinant GJ, Van Hasselt CM, Grol RP. Understanding laboratory testing in diagnostic uncertainty: a qualitative study in general practice. Br J Gen Pract. 2002;52:974–980. [PMC free article] [PubMed] [Google Scholar]
- 10.Hoffrage U, Gigerenzer G. Using natural frequencies to improve diagnostic inferences. Acad Med. 1998;73:538–540. doi: 10.1097/00001888-199805000-00024. [DOI] [PubMed] [Google Scholar]
- 11.Heller RF, Sandars JE, Patterson L, McElduff P. GPs’ and physicians’ interpretation of risks, benefits and diagnostic test results. Fam Pract. 2004;21:155–159. doi: 10.1093/fampra/cmh209. [DOI] [PubMed] [Google Scholar]
- 12.Vafiadis P. The dilemma of the unexpected result. Aust Fam Physician. 1996;25:971–975. [PubMed] [Google Scholar]
- 13.Brigden ML, Heathcote JC. Problems in interpreting laboratory tests. What do unexpected results mean? Postgrad Med. 2000;107:145. doi: 10.3810/pgm.2000.06.1127. 145-6,151-2,155-8,161-2. [DOI] [PubMed] [Google Scholar]
- 14.Symmons DP, Van Hemert AM, Vandenbroucke JP, Valkenburg HA. A longitudinal study of back pain and radiological changes in the lumbar spines of middle aged women. II. Radiographic findings. Ann Rheum Dis. 1991;50:162–166. doi: 10.1136/ard.50.3.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bugter-Maessen AM, Winkens RA, Grol RP, Knottnerus JA, Kester AD, Beusmans GH, et al. Factors predicting differences among general practitioners in test ordering behaviour and in the response to feedback on test requests. Fam Pract. 1996;13:254–258. doi: 10.1093/fampra/13.3.254. [DOI] [PubMed] [Google Scholar]
- 16.Kendrick D, Fielding K, Bentley E, Kerslake R, Miller P, Pringle M. Radiography of the lumbar spine in primary care patients with low back pain: randomized controlled trial. BMJ. 2001;322:400–405. doi: 10.1136/bmj.322.7283.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dijksterhuis PH, Van Boven C. De schatbare waarde van aanvullend onderzoek in de huisartspraktijk. Lelystad, NL: Meditekst; 1993. [Google Scholar]