Abstract
OBJECTIVE
To describe Ottawa family physicians’ perceptions of their preparedness to respond to outbreaks of infectious diseases or other public health emergencies and to assess their capacity and willingness to assist in the event of such emergencies.
DESIGN
Cross-sectional self-administered survey conducted between February 11 and March 10, 2004.
SETTING
The City of Ottawa, Ont, and the Department of Family Medicine at the University of Ottawa.
PARTICIPANTS
Ottawa family physicians; respondents can be considered a self-selected sample.
MAIN OUTCOME MEASURES
Self-reported office preparedness and physicians’ capacity and willingness to respond to public health emergencies.
RESULTS
Response rate was 41%. Of 676 physicians contacted, 274 responded, and of those, 246 completed surveys. About 26% of respondents felt prepared for an outbreak of influenza not well covered by vaccine. About 18% felt prepared for serious respiratory epidemics, such as severe acute respiratory syndrome; about 50% felt unprepared. Most respondents (80%) thought they were not ready to respond to an earthquake. About 77% of physicians were willing to be contacted on an urgent basis in case of a public health emergency. Of these, 94% would assist in immunization clinics, 84% in antibiotic clinics, 58% in assessment centres, 52% in treatment centres, 41% with declaration of death, 26% with home care, and 23% with telephone counseling.
CONCLUSION
Family physicians appear to be unprepared for, but willing to address, serious public health emergencies. It is essential to set up effective partnerships between primary care and public health services to support family physicians’ capacity to respond to emergencies. This type of study, along with the creation of a register of available services and of a virtual network for sharing information, is an initial step in assessing primary care response.
Abstract
OBJECTIF
Rapporter ce que les médecins de famille d’Ottawa croient posséder comme préparation pour répondre à des éclosions de maladies infectieuses ou à d’autres urgences de santé publique, et évaluer leur capacité d’aider advenant de telles urgences et leur empressement à le faire.
TYPE D’ÉTUDE
Enquête transversale auto-administrée effectuée entre le 11 février et le 10 mars 2004.
CONTEXTE
La ville d’Ottawa, Ontario, et le département de médecine familiale de l’Université d’Ottawa.
PARTICIPANTS
Des médecins de famille d’Ottawa; on peut considérer que l’échantillon est formé par les répondants volontaires.
PRINCIPAUX PARAMÈTRES MESURÉS
Comment les médecins évaluent la préparation de leur cabinet ainsi que leur capacité et empressement à répondre en cas d’urgences de santé publique.
RÉSULTATS
Le taux de réponse était de 41%. Sur 676 médecins contactés, 274 ont répondu et de ceux-ci, 246 ont complété les questionnaires. Environ 26% des répondants croyaient être préparés pour une éclosion de grippe en absence de couverture vaccinale adéquate. Environ 18% se disaient prêts à affronter une grave épidémie respiratoire comme le syndrome respiratoire aigu sévère; quelque 50% disaient ne pas l’être. La plupart des répondants (80%) ne croyaient pas pouvoir affronter un tremblement de terre. Environ 77% acceptaient d’être contactés sans délai en cas d’urgence de santé publique. Parmi ceux-ci, 94% participeraient aux cliniques de vaccination, 84% aux cliniques d’antibiothérapie, 58% aux centres d’évaluation, 52% aux centres de traitement, 41% aux certificats de décès, 26% aux soins à domicile et 23% au counseling téléphonique.
CONCLUSION
Même s’ils semblent mal préparés, les médecins de famille sont disposés à intervenir en cas d’urgence majeure de santé publique. Il est essentiel d’établir une collaboration adéquate entre les soins de première ligne et les services de santé publique afin d’aider le médecin de famille à répondre aux urgences. Ce type d’étude, associé à la création d’un registre des services disponibles et d’un réseau virtuel de partage de l’information, constitue un premier pas vers l’évaluation de la réponse des soins primaires.
EDITOR’S KEY POINTS.
This survey describes Ottawa, Ont, family physicians’ self-reported preparedness for, and willingness to respond to, public health emergencies, such as the severe acute respiratory syndrome epidemic.
Response rate was 41%. Among respondents, only about 25% felt at all prepared for an emergency, and almost 50% felt unprepared.
About 75% of respondents, however, indicated a willingness to help during emergencies doing such things as working in immunization, assessment, and treatment centres.
Family physicians appear willing to provide help with “surge capacity” for public health emergencies but want close support and communication with public health staff through e-mail, fax, and hot-line.
POINTS DE REPÈRE DU RÉDACTEUR.
Cette enquête rapporte le degré de préparation et d’empressement que croient avoir les médecins de famille d’Ottawa, Ontario, pour répondre à des urgences de santé publique comme une épidémie du syndrome respiratoire aigu sévère.
Le taux de réponse était de 41%. Environ 25% seulement des répondants estimaient posséder une certaine préparation pour une urgence et près de 50% croyaient n’en avoir aucune.
Toutefois, environ 75% des répondants se disaient disposés à aider en cas d’urgence, par exemple en travaillant dans des centres de vaccination, d’évaluation et de traitement.
Les médecins de famille paraissent donc prêts à fournir de l’aide dans un élan d’enthousiasme mais ils veulent un support étroit et une communication adéquate avec le personnel de santé publique par courrier électronique, télécopieur et ligne téléphonique prioritaire.
Public health emergencies, such as the recent severe acute respiratory syndrome (SARS) epidemic in Ontario or a threatened pandemic of influenza, underscore the need for surge capacity in responding to respiratory health threats and other health crises. The public health system in isolation, however, cannot be expected to respond effectively to such serious challenges that severely compromise resources.
Response to public health emergencies would be enhanced if existing primary care infrastructure were deployed to temporarily expand the public health work force. As generalists, primary care practitioners are flexible in their ability to respond to various population health needs in partnership with public health professionals.1 With support from public health and infectious disease experts, local community-based clinicians could be mobilized rapidly to deliver appropriate care and resources. Under epidemic conditions, it could be helpful also to have a decentralized health response. For instance, in the event that a mass immunization campaign is required, offering clinics in hundreds of different primary care offices would reduce the amount of contact people have with one another.
Internationally, a long history of policy indicates the importance of partnerships between primary care and public health services.2 Such policy has not been applied systematically to emergency preparedness, however. Very little research has been done in this area.3 Some have called for greater efforts, mainly after September 11,3-6 focusing on preparedness for bioterrorism but they have generally continued to neglect the public health–primary care overlap, with a few exceptions.3,7 One study done in Israel looked at patient preferences for care and physicians’ sense of responsibility in the case of bioterrorism, such as anthrax attacks.8 It found that one third of patients interviewed would go to emergency wards and two thirds would seek care from their family physicians or health authorities. Most physicians (89%) thought it was their responsibility to treat anthrax-infected patients. The study concluded that family physicians have a major role in bioterrorist emergencies.
The potential for enhancing public health surge capacity through participation of primary care practitioners has been virtually unexplored. Efforts in this direction have tended to look primarily at improving capacity at facility or public health system levels.9-11 How prepared primary care offices are to respond to health emergencies has not been ascertained, and we do not know what type of assistance they could provide or what additional equipment or personnel they might need to respond to various disasters. An effective response to serious health threats would be facilitated by a virtual network of primary care providers and public health authorities. No formal model is in place, however, to enable rapid mobilization of primary care providers nor is there a system to maintain readiness. There is a clear need for creating and maintaining a rapid communication infrastructure12 that includes contact data and information on the availability and capacity of primary care providers to assist in a range of emergency situations. As a step in that direction, this study seeks to explore Ottawa, Ont, family physicians’ perceptions of how well their offices are prepared to respond to infectious disease outbreaks or emergencies and of their capacity and willingness to assist in the event of public health emergencies.
METHOD
We conducted a cross-sectional survey of all family physicians in Ottawa. Self-administered questionnaires were sent out between February 11 and March 10, 2004. The complete list of all family doctors in Ottawa was developed in several stages. First, a previously compiled list from May 2002 based partly on the College of Physicians and Surgeons of Ontario’s database was updated by calling each practice listed, which resulted in identification of 609 family physicians. Then, through the Internet search engine MD Select (http://www.mdselect.com), 218 additional physicians were identified. This list was checked against the Academy of Medicine’s list of physicians to verify that all doctors listed were indeed family doctors. Ninety additional family physicians among the 218 were identified, for a total of 696. We contacted 676 of them. Physicians were included if they were classified in the source under family medicine or emergency family medicine or if their educational degrees were CCFP, CCFP(EM), MD, or GP/psychotherapy. Nonrespondents were followed up 3 times (by fax and a final telephone call) 2, 3, and 4 weeks after the initial communication. Because the survey was intended to reach all family physicians in Ottawa, sampling procedures were not used. Given the response rate, subjects could be considered a self-selected sample.
The survey questionnaire was developed by the investigators in consultation with a survey expert and was pretested by conducting 2 focus groups of 6 to 8 family physicians. Feedback was sought regarding its clarity, completeness, length, format, and question sequencing and was used to produce the final instrument. Likert-scale items were used to measure physicians’ preparedness and willingness to assist during public health emergencies. Composite measures for these constructs were not created. Instead, we reported the percentage of physicians indicating their level of agreement with questionnaire items or the type of responses. Preparedness was defined as the activities, programs, and systems in place before disasters or emergencies occur that can be used to support and enhance response in order to limit the effect. The Ottawa Hospital Research Ethics Board approved the study.
RESULTS
Of the 676 physicians surveyed, 41% (274) responded. Among those, 246 completed the survey, and 28 declined to do so.
Perceptions of office preparedness
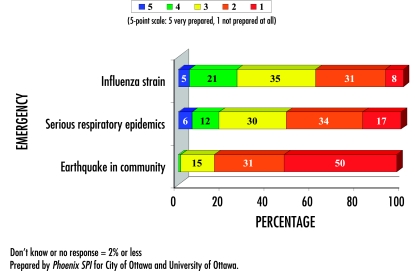
Figure 1 depicts family physicians’ ratings of how prepared their offices were to respond to public health emergencies, including outbreaks of influenza strains for which vaccines are or are not available, serious respiratory epidemics, and local earthquakes. Responses indicated that 26% of family physicians believed their offices were prepared to respond to outbreaks of influenza. Almost 40% believed they were not prepared for them, and 34% were not sure. With respect to serious respiratory epidemics, such as SARS, fewer than 1 in 5 (18%) thought their offices were prepared, and about 50% believed their offices were not prepared. Regarding earthquakes in the community, 81% of physicians believed that their offices were not equipped to respond.
Figure 1.
Level of preparedness to respond to public health emergencies
Interest in response measures
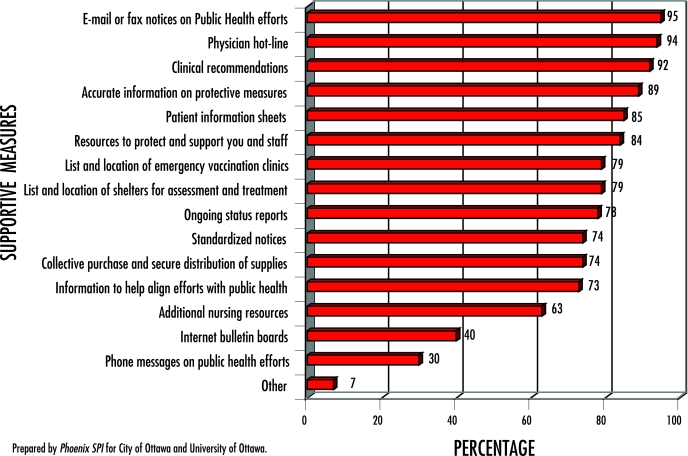
Figure 2 shows family physicians’ interest in various measures intended to support their ability to respond to public health emergencies. Between 73% and 95% of physicians expressed an interest in 12 of the 16 measures. Most family physicians were interested in e-mail or fax notices on public health efforts (95%) and a hot-line for physicians (94%). There was also strong interest in clinical recommendations (92%) and accurate information on protective measures (89%). Interest in Internet bulletin boards or discussion groups (40%) or telephone messages on public health efforts (30%) was lower.
Figure 2. Interest in measures to support family physicians’ ability to respond to public health emergencies.
Multiple responses were accepted.
Participation in surge capacity
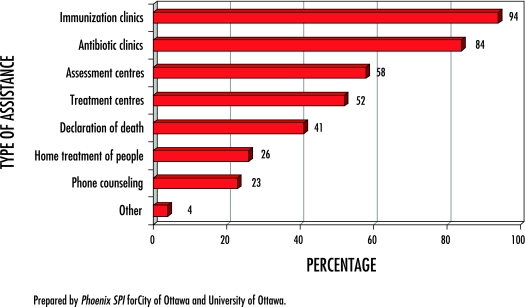
More than 75% of physicians surveyed indicated their willingness to be contacted on an urgent basis in the event of public health emergencies by Ottawa’s Public Health Department and to help according to their capacity. One in 5 (21%) indicated that they were not willing to be contacted.
Physicians willing to help (n = 189) were asked to identify the type of assistance they would be willing to offer (Figure 3). Most said they would assist in immunization clinics (94%) and antibiotic clinics (84%). More than half indicated a willingness to provide assistance in assessment centres (58%) and treatment centres (52%).
Figure 3. Areas in which physicians would be willing to assist during public health emergencies.
N=189; asked of those willing to help; multiple responses were accepted.
Office resources available
Physicians were asked to report how many examination rooms they had and the capacity of their waiting rooms. Slightly more than half (54%) indicated that they had 6 or more examination rooms, 21% had 3 to 5 rooms, and 23% had 1 or 2 rooms. In terms of waiting rooms, about half the physicians indicated that their waiting rooms could accommodate 16 or more patients.
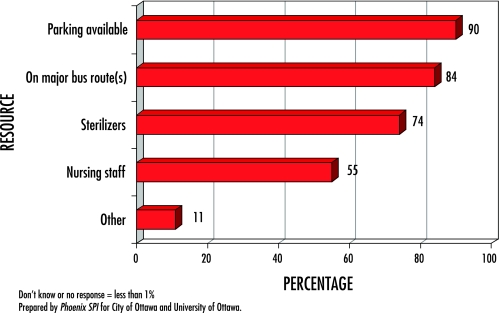
When asked to identify other office resources or attributes at their disposal that could be available in the event of a public health emergency (Figure 4), 90% of physicians indicated that parking was available at their offices, 84% noted that their offices were on major bus routes, and 74% said their practices had sterilizers. About 55% reported having nursing staff as a resource. The other 7% of resources identified included counselors, hospital access, on-site pharmacies or physiotherapy, storage and meeting facilities, supplies, and specialists.
Figure 4.
Office resources available for public health emergencies
Website interest
Just over half the physicians surveyed (58%) expressed an interest in a website for Ottawa public health issues. Those interested in such a website were asked to rate their interest in the various features it might have. Most endorsed having access to reports on emerging illnesses or trends (76%) and a directory of local resources (68%). About 60% expressed an interest in links to top Canadian and American websites related to public health issues (60%), a question-and-answer section (59%), and disaster-preparedness plans (57%) among other things.
DISCUSSION
These results indicate that Ottawa family physicians perceive their offices as currently unprepared to address serious public health crises. This is consistent with the perceptions of American family physicians of their capacity to respond to bioterrorist attacks.3 At the same time, surveyed physicians reported a widespread willingness to help increase surge capacity in the event of serious public health emergencies and to share their available resources. Physicians also were interested in support for their capacity to respond and in maintaining a website regarding public health issues for the city.
Physicians’ perceptions of their preparedness to face public health emergencies confirm that, despite calls for building partnerships between primary care and public health services,2 such joint efforts have not yet prepared Ottawa for emergencies. This gap needs to be addressed, especially in light of an increased focus on risk of bioterrorism3,7 and on risk of an avian influenza pandemic.
This survey is only the first step in coordinating emergency planning between family physicians and local public health authorities. Targeted continuing education programs can foster this collaboration, and there are plans for follow-up communication with the physicians who indicated an interest in working with public health services. Harnessing the capacity of community-based primary care practices would enhance public health response to emergencies by temporarily expanding the work force and providing important resources.
The creation of a virtual network that includes Ottawa family physicians is a vital initial step in ensuring their participation in surge capacity for an effective response. A climate of primary care reform, the renewed threat of public health epidemics, and further research in this area could increase recognition of the importance of increasing surge capacity to minimize the health effects of emergencies on the general population. Further studies of whether family physicians in other Canadian cities have similar perceptions regarding their preparedness for public health emergencies are needed.
Limitations
The main limitation of the study is the 41% response rate. Respondents can be considered as a self-selected sample of interested physicians or “keeners.” Assuming that this group would be more likely to participate in preparedness activities owing to their interest in them, it is feasible to infer that the real gap in preparedness is greater than respondents perceive. Given the survey’s response rate, the representativeness of the results is limited. Also, because they are based on responses from only 1 urban centre in Canada, we cannot be sure of the generalizability of our results. Surveys with representative samples are worth repeating in other places.
Conclusion
Overall, family physicians appear to be unprepared for, but willing to address, serious public health emergencies. It is essential to set up effective partnerships between primary care and public health services to support family physicians’ response capacity. This type of study, along with the creation of a register of available services and of a virtual network for sharing information, is an initial step in assessing primary care response.
Acknowledgments
We thank Steve Kiar for his expert advice and for conducting the focus groups on developing the survey instrument.
Biographies
Dr Hogg is a Professor and Director of Research in the Department of Family Medicine and Principal Scientist in the Institute of Population Health at the University of Ottawa and is Director of the C.T. Lamont Primary Health Care Research Centre at the Élisabeth Bruyère Research Institute in Ontario.
Dr Huston was Associate Medical Officer of Health and Manager of Surveillance of Emerging Issues in the Education and Research Division of the City of Ottawa’s Public Health Branch at the time of the study.
Dr Martin is an Associate Professor of family medicine at the Northern Ontario School of Medicine and an Adjunct Professor at the Indigenous Peoples’ Health Research Centre, First Nations University of Canada.
Dr Soto is a Research Manager in the Institute of Population Health at the University of Ottawa.
Footnotes
Competing interests: None declared
References
- 1.Department of Health and Ageing, General Practice Strategy Review Group. General practice: changing the future through partnerships [monograph on the Internet]. Canberra, Aust: Commonwealth of Australia; 1998. [cited 2004 July 11]. Available from: http://www.health.gov.au/internet/wcms/publishing.nsf/Content/health-pcd-publications-gpsrg-gpsrgrpt.htm. [Google Scholar]
- 2.Marriott J, Mable AL. Opportunities and potential: a review of international literature on primary health care reform and models [monograph on the Internet]. Ottawa, Ont: Health Human Resource Strategies Division, Health Policy and Communications Branch, Health Canada; 2000. [cited 2004 July 11]. Available from: http://www.hc-sc.gc.ca/phctf-fassp/english/eng-manual.pdf. [Google Scholar]
- 3.Chen F, Hickner J, Fink K, Galliher J, Burstin H. On the front lines: family physicians’ preparedness for bioterrorism. J Fam Pract. 2002;51(9):745–750. [PubMed] [Google Scholar]
- 4.Geiger HJ. Terrorism, biological weapons and bonanzas: assessing the real threat to public health [letter: comment]. Am J Public Health. 2001;91(5):708–709. doi: 10.2105/ajph.91.5.708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Henretig E. Biological and chemical terrorism defense: a view from the “front lines” of public health [letter: comment]. Am J Public Health. 2001;91(5):718–720. doi: 10.2105/ajph.91.5.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lichtveld M, Cioffi J, Henderson J, Sage M, Steele L. People protected—public health preparedness through a competent workforce [editorial]. J Public Health Manag Pract. 2003;9(5):340–343. doi: 10.1097/00124784-200309000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Rippen H, Gursky E, Stoto M. Importance of bioterrorism preparedness for family physicians [editorial]. Am Fam Physician. 2003;67(9):1877–1878. [PubMed] [Google Scholar]
- 8.Kahan E, Fogelman Y, Kitai E, Vinker S. Patient and family physician preferences for care and communication in the eventuality of anthrax terrorism. Fam Pract. 2003;20(4):441–442. doi: 10.1093/fampra/cmg419. [DOI] [PubMed] [Google Scholar]
- 9.Hick J, Hanfling D, Burstein J, DeAtley C, Barbisch D, Bogdan G, et al. Health care facility and community strategies for patient care surge capacity. Ann Emerg Med. 2004;44(3):253–261. doi: 10.1016/j.annemergmed.2004.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Srinivasan A, McDonald L, Jernigan D, Helfand R, Ginsheimer K, Jernigan J, et al. Foundations of the severe acute respiratory syndrome preparedness and response plan for healthcare facilities. Infect Control Hosp Epidemiol. 2004;25(12):1020–1025. doi: 10.1086/502338. [DOI] [PubMed] [Google Scholar]
- 11.Gostin L. Pandemic influenza: public health preparedness for the next global health emergency. J Law Med Ethics. 2004;2(4):565–573. doi: 10.1111/j.1748-720x.2004.tb01962.x. [DOI] [PubMed] [Google Scholar]
- 12.United States Department of Health and Human Services, Best Practices Initiative. Fax communication with primary care providers during public health emergencies. Rhode Island Department of Health 2002. Washington, DC: United States Department of Health and Human Services; 2002. [cited 2004 July 11 [page updated 2005 June 1]]. Available from: http://phs.os.dhhs.gov/ophs/BestPractice/RI.htm. [Google Scholar]