Abstract
OBJECTIVE
To propose a diagnostic and therapeutic approach to feeding problems in early childhood.
QUALITY OF EVIDENCE
Articles were retrieved through a MEDLINE search from January 1990 to December 2005 using the MeSH terms eating disorders, infant, and child. Recommended practice is based mainly on levels II and III evidence.
MAIN MESSAGE
Feeding problems are classified under structural abnormalities, neurodevelopmental disabilities, and behavioural disorders, with overlap between categories. A medical approach also needs an evaluation of diet and an assessment of the interaction between parent and child. Treating medical or surgical conditions, increasing caloric intake, and counseling about general nutrition can alleviate mild to moderate problems. More complicated cases should be referred to multidisciplinary teams. Behavioural therapy aims to foster appropriate behaviour and discourage maladaptive behaviour.
CONCLUSION
Feeding problems in early childhood often have multifactorial causes and a substantial behavioural component. Family physicians have a key role in detecting problems, offering advice, managing mildly to moderately severe cases, and referring more complicated cases to multidisciplinary teams.
Abstract
OBJECTIF
Proposer une façon de diagnostiquer et traiter les problèmes alimentaires des jeunes enfants.
QUALITÉ DES PREUVES
On a fait un relevé d’articles dans MEDLINE entre janvier 1990 et décembre 2005 à l’aide des termes MeSH eating disorders, infant et child. Les pratiques recommandées reposent sur des preuves de niveaux II et III.
PRINCIPAL MESSAGE
Les problèmes alimentaires peuvent relever d’anomalies structurelles, de désordres neurodéveloppementaux et de troubles du comportement, ces catégories se chevauchant. L’approche médicale doit aussi évaluer le régime ainsi que l’interaction parent-enfant. Se peut être efficace de traiter les conditions médicales ou chirurgicales, d’augmenter l’apport calorique et de donner des conseils généraux sur la nutrition dans les cas légers à modérés. Les cas plus compliqués devraient être adressés à des équipes multidisciplinaires. La thérapie comportementale vise à favoriser un comportement approprié et à décourager un comportement inadapté.
CONCLUSION
Les problèmes alimentaires de la petite enfance ont souvent des causes multiples ainsi qu’une importante composante comportementale. Le médecin de famille joue un rôle clé pour détecter ces problèmes, donner des conseils, traiter les cas légers à modérés et diriger les cas plus compliqués à des équipes multidisciplinaires.
EDITOR’S KEY POINTS.
Some 25% to 40% of infants and toddlers are reported by their caregivers to have feeding problems, mainly colic, vomiting, slow feeding, and refusal to eat. This article reviews the classification and clinical features of such problems, proposes an approach to diagnosis, and describes some practical therapeutic strategies.
Five key elements should be considered in evaluating feeding disorders. How does the problem manifest? Is the child suffering from disease? Have the child’s weight and development been affected? What is the atmosphere during meals? Is the family under stress?
When infants are growing and developing normally, physicians should reassure parents and explain that no investigations are indicated at that point.
Family physicians are in a key position to detect problems early on, to make a differential diagnosis, to give practical advice to parents, and to initiate therapy.
POINTS DE REPÈRE DU RÉDACTEUR.
Au dire de ceux qui s’en occupent, environ 25% à 40% des bébés et jeunes enfants présentent des problèmes alimentaires, principalement sous la forme de coliques, vomissements, lenteur des repas et refus de manger. Cet article fait le point sur la classification et les caractéristiques cliniques de ces problèmes, propose une approche au diagnostic et décrit certaines stratégies thérapeutiques pratiques.
Cinq éléments clés devraient être pris en compte lorsqu’on évalue les problèmes alimentaires. Comment le problème se manifeste-t-il? L’enfant souffre-t-il d’une maladie? Son poids et son développement sont-ils affectés? Quel est l’atmosphère durant les repas? La famille est-elle sous stress?
Si l’enfant croît et se développe normalement, on doit rassurer les parents et expliquer qu’aucune investigation n’est requise pour le moment.
Le médecin de famille est bien placé pour détecter précocement ces problèmes, faire le diagnostic différentiel, donner des conseils pratiques aux parents et initier le traitement.
Feeding is an important part of the everyday life of infants and young children, and much parent-child interaction occurs at feeding times. About 25% to 40% of infants and toddlers are reported by their caregivers to have feeding problems, mainly colic, vomiting, slow feeding, and refusal to eat.1
Although some of these difficulties are transient, some problems, such as refusal to eat, are found in 3% to 10% of children and tend to persist.2-6 Parents soon become concerned and turn to their family physicians for advice. This article reviews the classification and clinical features of early childhood feeding problems, proposes a diagnostic approach, and describes some practical therapeutic strategies.
Quality of evidence
MEDLINE was searched for all articles published in English or French between January 1990 and December 2005 using the MeSH terms eating disorders, infant, and child. The references of articles retrieved were searched for further articles not found in the MEDLINE search. There were few randomized controlled trials, and those that were identified had few patients enrolled. Recommended practice is based mainly on levels II and III evidence.
Classification of feeding disorders
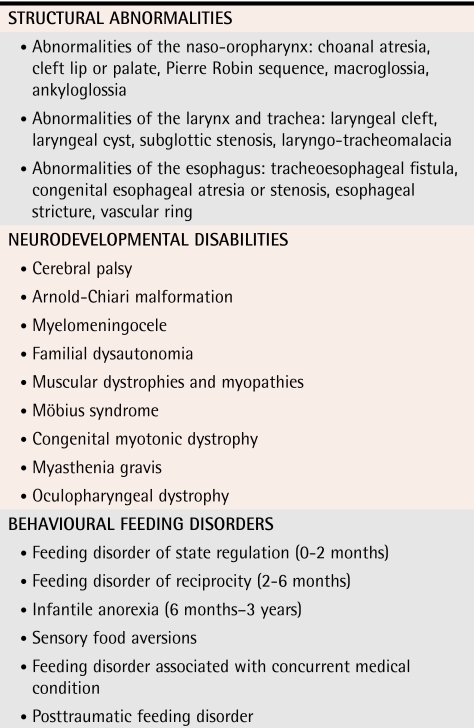
Feeding disorders can be classified under 3 categories (Table 1), although there is often overlap among categories. Structural abnormalities affect 3 areas: the naso-oropharynx, the larynx and trachea, and the esophagus. Neurodevelopmental disabilities disrupt the process of “learning to eat” and can result in oral hypersensitivity and oral-motor dysfunction. The third category is behavioural feeding disorders, as defined by Diagnostic and Statistical Manual of Mental Disorders, 4th edition, text revision (DSM-IV-TR)7 criteria, which have been refined by Chatoor.8 Describing these disorders, however, is beyond the scope of this review. It should be emphasized that, at present, these disorders have been described mainly from a single site and that their face validity is overly dependent on case reports (level II evidence).
Table 1.
Classification of feeding disorders
Evaluating feeding problems
Five key elements should be considered in evaluating feeding disorders.
How is the problem manifested?
Is the child suffering from any disease?
Have the child’s weight and development been affected?
What is the emotional climate like during the child’s meals?
Are there any great stress factors in the family?
History
Medical history should include antenatal and perinatal history; family history of atopy or feeding problems; previous illnesses and hospitalizations; and manipulation around the oropharynx, such as tube feeding. The chronology of feeding problems, diet since birth, changes of formulas, introduction of solids, current diet, textures, route and time of administration, and feeding position should be recorded. Food aversions, quantities eaten, length of meals and associated routines, strategies already used, and environment and behaviour around mealtimes need to be documented.
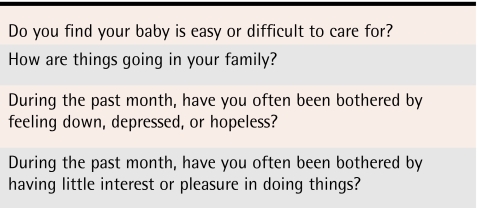
Anatomic abnormalities should be suspected when children have problems swallowing. A history of recurrent pneumonia should alert physicians to chronic aspiration because about 70% to 94% of episodes of aspiration are “silent.”9 Stridor in relation to feeding could be due to glottic or subglottic abnormalities. Suck-swallow-breathing coordination can be affected by choanal atresia. Vomiting, diarrhea, or constipation; colic; and abdominal pain should alert physicians to the possibility of gastroesophageal reflux (GER) or allergy to cow’s milk, because some symptoms are similar for both diseases.10 Finally, physicians should explore social stress, family dynamics, and emotional problems. Examples of questions that might elicit information on maternal depression11 are shown in Table 2.
Table 2.
Questions that elicit information about maternal depression
Physical examination
Physical examination should start with anthropometric measurements, including head circumference. A growth curve should have been documented since birth. Craniofacial abnormalities, signs of systemic disease, and atopy should be sought. A complete neurologic examination is mandatory, as is an evaluation of psychomotor development.
Investigations
No laboratory investigations are indicated for infants with normal results of physical examinations, normal growth curves, and normal results of developmental assessments. For children with colic and occasional vomiting, an immunoglobulin E–mediated cow’s milk allergy can be suspected. Confirmation of this diagnosis with skin testing and radioallergosorbent testing is not readily available, however, and these tests are not completely reliable either12 (level I evidence). Gastroesophageal reflux should be considered. Although upper gastrointestinal contrast studies are neither sensitive nor specific for GER, they allow observation of the coordination as a bolus is moved through the oropharynx and esophagus and for detection of anatomic abnormalities, such as malrotation.13 Esophageal pH monitoring is not readily available and should be reserved for patients who do not respond to empiric treatment with acid suppressants13 (level II evidence).
Feeding problems that appear to stunt growth need thorough investigation. First-line laboratory investigations should include a complete blood count and assessment of sedimentation rate, serum albumin and protein, serum iron, iron-binding capacity, and serum ferritin to detect specific nutrient deficits and to assess hepatic and renal function, as well as a sweat test to screen for systemic diseases. Antitransglutaminase antibodies for celiac disease are becoming more widely available. If diagnosis of GER is unclear, esophagogastroduodenoscopy and biopsy can determine the presence and severity of esophagitis, strictures, and webs13 (level II evidence).
A detailed dietary history must be taken with the help of a nutritionist, if possible. Quality and quantity of food ingested must be assessed to document deficits in calories, vitamins, and trace elements and food aversions. Physicians should inquire about excessive consumption of milk or fruit juices.
Parent-child interactions during feeding should be assessed. Positive interactions, such as eye contact, reciprocal vocalizations, praise, and touch, and negative interactions, such as forced feeding, coaxing, threatening, and children’s disruptive behaviour (turning the head away from food, throwing food) should be noted. An assessment should also document behaviour occurring before food is presented, such as prompting and positive reinforcement for accepting food and use of neutral or ineffective consequences for other behaviour.14
Management of feeding disorders
When infants are growing and developing normally, physicians should reassure parents and explain that no investigations are indicated at this point. In cases of colic and occasional vomiting, dietary intervention is worth a trial. Excluding allergenic foods, such as dairy products, eggs, nuts, fish, soy, and wheat, from the breastfeeding mother’s diet or giving bottle-fed infants hypoallergenic formulas might reduce symptoms of colic, mainly in infants with a positive family history of atopy15 (level I evidence). If physicians suspect cow’s milk allergy, mainly in atopic families, excluding allergenic foods can be empirically suggested to breastfeeding mothers and hypoallergenic formulas can be suggested for infants not breastfed12 (level III evidence).
If vomiting and irritability persist despite use of hypoallergenic formulas, a trial of acid suppression is worth initiating under the assumption of a possible overlap between cow’s milk allergy and GER. Histamine-2 receptors can be used, followed by proton pump inhibitors (levels II and III evidence). Cisapride, a drug restricted because of the risk of arrythmias, should not be used before confirmation of GER by esophageal pH monitoring13 (level I evidence).
If a child’s growth appears to be stunted, caloric intake should be increased. Human milk can be fortified with formula powder, carbohydrate, or fat. Infant formula can be concentrated up to 3.4 to 4.2 kJ/mL, by either lessening dilution or adding glucose polymers or vegetable oil. Solid foods can be fortified with butter, vegetable oil, cream, sauces, glucose polymers, and powdered milk (level III evidence).
Children with normal neurologic function generally do well after surgical correction of anatomic abnormalities. Neurologically disabled children, however, need nasogastric or gastrostomy feedings when they are unable to ingest adequate calories safely and when the time required to provide adequate nutrition by mouth consumes parents’ and children’s lives, leaving little time for nurturing activities9 (level III evidence).
Coexisting medical problems should be addressed. Good medical management does not always alleviate feeding problems adequately. For instance, young children with cystic fibrosis often have a pattern of eating slowly, having difficulty chewing, preferring liquids, refusing to eat solids, and having an aversion to new food.5 Retrospective and case-control studies have shown that, despite medical and surgical therapy, infants with GER have lower intake of energy-generating food, have fewer adaptive skills and less readiness for solids, are more likely to refuse food, and are more demanding and difficult at feeding time6,16 (level II evidence). Under these conditions, behavioural interventions should be considered.
Behavioural interventions
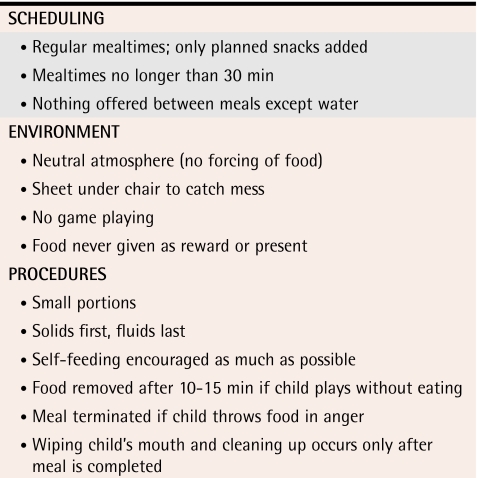
Parents should first know the basic food rules that apply to all young children17 (Table 3). Parents should control what, when, and where children are being fed. Children should control how much they eat in order to learn internal regulation of eating in accordance with physiologic signals of hunger and fullness.
Table 3.
Food rules applicable to children beyond infancy
In the feeding disorder termed “state regulation,” mothers should be helped to modulate the amount of stimulation during feeding (level III evidence). Infants should be fed promptly before prolonged crying (not more than 30 minutes) and should not be unnecessarily aroused, burped, or wiped. Mothers’ anxiety, fatigue, or depression should be addressed.18
In the feeding disorder termed “reciprocity,” the focus should be on training parents in sensitivity and responsiveness to infants’ feeding cues18 (level III evidence). Complicated cases need a multidisciplinary approach where family physicians can play a key role in coordinating services.
In cases of infantile anorexia, the mother-child dyad becomes involved in conflicting interactions, with a struggle for control and food being the battleground. Therapy consists of helping parents understand their children’s special temperaments, set limits, and structure mealtimes to facilitate the internal regulation of eating and to counteract the external regulation produced by emotional interactions within the caregiving environment.19 Food rules are strongly encouraged, and “time out” should be used in response to children’s inappropriate behaviour (level II evidence).
Prevention of sensory food aversions starts with introducing various foods at 4 to 6 months of age. New foods should be introduced singly and not during illnesses, such as colds and diarrhea, and parents should persevere and present the new food day after day until children get used to it. Toddlers more easily accept a new food if they see their parents eating it. Withholding favourite food to get toddlers to eat “healthy” food seems to have a negative effect.20 Treatment of food aversions is based on increasing appropriate behaviour through positive reinforcement and decreasing maladaptive behaviour by extinction (removing what reinforces a response) and time out14 (level II evidence).
Feeding problems associated with concurrent medical conditions might result from an interaction between intrinsic oral motor dysfunction, oral hypersensitivity, odynophagia, and learned aversive behaviour. Parents should be taught management skills, such as setting clear time limits for meals, ignoring non-eating behaviour, and using contingencies (active praising, positive reinforcement) to motivate children to meet the food-intake goals that have been set21 (level I evidence).
Infants with posttraumatic feeding disorder are generally receiving enteral tube feeding that interferes with their experience of hunger and development of oropharyngeal coordination. Treatment is aimed at eliminating tube feeding and overcoming the resistance to oral feeding, either through the behavioural technique of extinction, which was shown to be successful in 1 controlled study22 (level I evidence), or by gradual desensitization (level II evidence).8
Conclusion
Infants’ and toddlers’ feeding problems often have multifactorial causes and a substantial behavioural component. During well-child visits, family physicians are in a key position to detect problems early on; to make differential diagnoses; to give practical advice to parents on food rules and increase of caloric intake, if needed; and to initiate therapeutic approaches to colic, cow’s milk allergy, and GER. More complicated cases are generally managed by multidisciplinary teams; primary care physicians can have a key role in coordinating services.
Levels of evidence.
Level I: At least one properly conducted randomized controlled trial, systematic review, or meta-analysis
Level II: Other comparison trials, non-randomized, cohort, case-control, or epidemiologic studies, and preferably more than one study
Level III: Expert opinion or consensus statements
Biography
Dr Bernard-Bonnin is an Associate Professor of Pediatrics at CHU Ste-Justine at the University of Montreal in Quebec. Her main interest is in ambulatory pediatrics, and she is a member of the Nutrition Clinic at the Ste-Justine Outpatient Department.
Footnotes
Competing interests: None declared
References
- 1.Reau NR, Senturia YD, Lebailly SA, Christoffel KK. (the Pediatric Practice Research Group). Infant and toddler feeding patterns and problems: normative data and a new direction. J Dev Behav Pediatr. 1996;17:149–153. [PubMed] [Google Scholar]
- 2.Dahl M. Early feeding problems in an affluent society. III. Follow-up at two years: natural course, health, behaviour and development. Acta Paediatr Scand. 1987;76:872–880. doi: 10.1111/j.1651-2227.1987.tb17257.x. [DOI] [PubMed] [Google Scholar]
- 3.Dahl M, Sundelin C. Feeding problems in an affluent society. Follow-up at four years of age in children with early refusal to eat. Acta Paediatr. 1992;81:575–579. doi: 10.1111/j.1651-2227.1992.tb12303.x. [DOI] [PubMed] [Google Scholar]
- 4.Dahl M, Rydell AM, Sundelin C. Children with early refusal to eat: follow-up during primary school. Acta Paediatr. 1994;83:54–58. doi: 10.1111/j.1651-2227.1994.tb12952.x. [DOI] [PubMed] [Google Scholar]
- 5.Mitchell MJ, Powers SW, Byars KC, Dickstein S, Stark LJ. Family functioning in young children with cystic fibrosis: observations on interactions at mealtime. J Dev Behav Pediatr. 2004;25:335–346. doi: 10.1097/00004703-200410000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Nelson SP, Chen EH, Syniar GM, Christoffel KK. [cited 1998 December 1];One-year follow-up of symptoms of gastroesophageal reflux during infancy. 1998 102:67. doi: 10.1542/peds.102.6.e67. Available from: http://pediatrics.aappublications.org/cgi/content/full/102/6/e67. [DOI] [PubMed]
- 7.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Text revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 8.Chatoor I. Feeding and eating disorders of infancy and early childhood. In: Weiner JM, Dulcan MK, editors. Textbook of child and adolescent psychiatry. Arlington, Va: American Psychiatric Publishing Inc; 2004. pp. 639–652. [Google Scholar]
- 9.Arvedson JC. Management of pediatric dysphagia. Otolaryngol Clin North Am. 1998;31:453–475. doi: 10.1016/s0030-6665(05)70064-5. [DOI] [PubMed] [Google Scholar]
- 10.Salvatore S, Vandenplas Y. Gastroesophageal reflux and cow milk allergy: is there a link? Pediatrics. 2002;110:972–984. doi: 10.1542/peds.110.5.972. [DOI] [PubMed] [Google Scholar]
- 11.Green M. Diagnosis, management, and implications of maternal depression for children and pediatricians. Curr Opin Pediatr. 1994;6:525–529. doi: 10.1097/00008480-199410000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Bahna SL. Cow’s milk allergy versus cow milk intolerance. Ann Allergy Asthma Immunol. 2002;89(6 Suppl 1):56–60. doi: 10.1016/s1081-1206(10)62124-2. [DOI] [PubMed] [Google Scholar]
- 13.Rudolf CD, Mazur LJ, Liptak GS, Baker RD, Boyle JT, Colletti RB, et al. North American Society for Pediatric Gastroenterology and Nutrition. Pediatric Gastroesophageal Reflux Clinical Practice Guidelines. J Pediatr Gastroenterol Nutr. 2001;32(Suppl 2):1–31. doi: 10.1097/00005176-200100002-00001. [DOI] [PubMed] [Google Scholar]
- 14.Babbitt RA, Hoch TA, Coe DA, Cataldo MF, Kelly KJ, Stackhouse C, et al. Behavioral assessment and treatment of pediatric feeding disorders. J Dev Behav Pediatr. 1994;15:278–291. [PubMed] [Google Scholar]
- 15.Garrison MM, Christakis DA. A systematic review of treatments for infant colic. Pediatrics. 2000;106:184–190. [PubMed] [Google Scholar]
- 16.Mathisen B, Worrall L, Masel J, Wall C, Shepherd RW. Feeding problems in infants with gastro-oesophageal reflux disease: a controlled study. J Paediatr Child Health. 1999;35:163–169. doi: 10.1046/j.1440-1754.1999.t01-1-00334.x. [DOI] [PubMed] [Google Scholar]
- 17.Chatoor I, Dickson L, Schaefer S, Egan J. A developmental classification of feeding disorders associated with failure to thrive: diagnosis and treatment. In: Drotar D, editor. New directions in failure to thrive: research and clinical practice. New York, NY: Plenum Press; 1985. pp. 235–258. [Google Scholar]
- 18.Satter EM. The feeding relationship: problems and interventions. J Pediatr. 1990;117:181–189. doi: 10.1016/s0022-3476(05)80017-4. [DOI] [PubMed] [Google Scholar]
- 19.Chatoor I, Hirsch R, Persinger M. Facilitating internal regulation of eating: a treatment model of infantile anorexia. Inf Young Children. 1997;9(4):12–22. [Google Scholar]
- 20.Birch LL. Development of food preferences. Ann Rev Nutr. 1999;19:41–62. doi: 10.1146/annurev.nutr.19.1.41. [DOI] [PubMed] [Google Scholar]
- 21.Powers SW, Jones JS, Ferguson KS, Piazza-Waggoner CP, Daines C, Acton JD. Randomized clinical trial of behavioral and nutrition treatment to improve energy intake and growth in toddlers and preschoolers with cystic fibrosis. Pediatrics. 2005;116:1442–1450. doi: 10.1542/peds.2004-2823. [DOI] [PubMed] [Google Scholar]
- 22.Benoit D, Wang EE, Zlotkin S. Discontinuation of enterostomy tube feeding by behavioural treatment in early childhood: a randomized controlled trial. J Pediatr. 2000;137:498–503. doi: 10.1067/mpd.2000.108397. [DOI] [PubMed] [Google Scholar]