Abstract
PURPOSE One in 4 Swedish women experiences a hip fracture, an event that has high concomitant morbidity and mortality. We developed and validated a clinical predictor of fracture and mortality risk, the Fracture and Mortality (FRAMO) Index.
METHODS This was a population-based prospective cohort study with a baseline questionnaire and 2-year outcomes of hip fracture, fragility fracture, and death. The questionnaire was sent to 1,498 women aged 70 years or older in 3 rural populations, asking them about their age, weight, height, mobility, previous fractures, smoking, medication use, and housing. Some women were also asked about previous vertebral radiographs. We defined 2 risk models before outcome data collection and subsequently renamed 1 model (age =80 years, weight <60 kg, previous fragility fracture, and the need to use arms to rise from the sitting position) the FRAMO Index. We used logistic regression analysis to study the association between the FRAMO Index and outcomes in all participants.
RESULTS The participation rate was 83% in this elderly female population (N = 1,248). The 63% of women with 0 to 1 risk factor had a 2-year hip fracture risk of 0.8% and mortality risk of 3.2%. In contrast, women with 2 to 4 risk factors had a 2-year hip fracture risk of 5.4% (odds ratio = 7.5; 95% confidence interval, 3.0–18.4) and mortality risk of 23.7% (odds ratio = 9.5; 95% confidence interval, 6.0–14.9). These differences remained significant after adjustment for age as a continuous variable. Mortality increased with the number of risk factors. The proportion of women reporting previous vertebral fractures was higher among the group specifically questioned about vertebral radiographs (P <.001).
CONCLUSIONS The FRAMO Index identified the majority of women who experienced hip fractures during a 2-year follow-up, who might have been candidates for intensified preventive measures. The FRAMO Index, based on 4 binary risk factors, would be practical for routine use in primary care.
Keywords: Hip fractures; fractures, bone; mortality; women; aged; risk factors; risk assessment; primary health care; Sweden
INTRODUCTION
Hip fracture is an increasing problem worldwide.1 One in 4 Swedish women (23%) experiences a hip fracture during her lifetime, an event that is associated with 20% mortality within 1 year. 2,3 There are several methods for fracture prevention, although they are underused in routine health care.
Combinations of low bone mineral density (BMD) with certain clinical risk factors are associated with an increased risk of hip fracture,4–8 but low BMD alone is less predictive of fracture.4,9,10 Many individuals who have an elevated risk of hip fracture might be identified by clinical risk factors alone.4,5,11 Previously described risk factor models for hip fracture are fairly complicated, requiring several weighted variables. Six clinical risk factors (2 weighted) and BMD assessment predicted fractures in the Study of Osteoporotic Fractures (SOF), and this risk factor combination was validated in another elderly community-based female population, the European Patent Information and Document Service (EPIDOS) fracture study.5 That study found that the combination had a sensitivity of 78.6% and specificity of 61.7% for predicting hip fracture within 5 years. The Melton Osteoporotic Fracture (MOF) study investigated 6 weighted clinical risk factors in an elderly female population in primary care and found that this combination had a sensitivity of 84% and specificity of 68% for hip fracture within 3 years.11
In this study, we selected 5 established clinical risk factors for hip fracture that we expected would be easy to ascertain and prevalent among elderly women.4,5,9,12–14 By combining only 4 of these factors and creating risk indices, we aimed to facilitate risk factor assessment during routine consultations. The goal of our study was to develop and validate a practical tool for hip fracture risk assessment and assess its ability to predict fractures and total mortality.
METHODS
Study Population
Our study population was drawn from 1,498 women aged 70 years or older living in 3 rural primary health care districts in southern Sweden. They were recruited from the National Swedish Population Register in November 2001. We selected the entire female population in the Vislanda district (501 women) and a similar number of age-matched women from each of 2 other districts, Tingsryd and Emmaboda. The Regional Ethics Committee at the University of Lund approved the study (LU 406-00).
Questionnaire Data and Follow-up
We sent the women a 22-item questionnaire focused on risk factors for fracture, combined with brief advice on fracture prevention. A relative or caregiver was allowed to assist women in answering the questions, most of which were multiple choice. Nonresponders were reminded twice by mail within 2 months.
We tested 2 risk models (described further below). The questions used for risk model 1 were age, weight, need to use arms to rise from the sitting position, and previous fragility fracture after age 40 (Table 1 ▶). These risk factors and questions about falls during the last year, maternal history of hip fracture, current height, and health perception were similar to the questions in the study by Cummings et al.4 Questions about previous fracture, smoking, and use of cortisone medication were used in the Scandinavian Scandos study.14 In a previous study among 73 women in the Vislanda district, the question about previous fragility fracture had a 3-year reliability of 94% (17 of 18 responses agreeing).15 If the location of a reported fragility fracture was uncertain, we determined the location by using the primary care system’s radiology data bank, which recorded fractures since 1994 or 1999 in these 3 districts. We did not search medical records for earlier radiology results.
Table 1.
Questions Used to Assess the 4 Risk Factors in Risk Model 1
| Question | Points |
| 1. What is your present age? | |
| ≥80 y | 1 |
| 70–79 y | 0 |
| 2. What is your current weight? | |
| <60 kg | 1 |
| ≥60 kg | 0 |
| 3. Can you rise 5 times from a chair without using your arms? (Try if you want.) | |
| No, I must use my arms to rise | 1 |
| Yes | 0 |
| 4. Have you broken any bones after the age of 40 y? | |
| If so, which bone? | |
| Have your vertebrae been x-rayed?* | |
| Fracture of wrist/lower arm, upper arm, hip, or vertebrae, or vertebral compression seen on radiograph | 1 |
| No fracture, or fracture in some other location | 0 |
* Specific question about vertebral radiographs posed only to women in the Vislanda population.
We asked the Vislanda population additional specific questions about previous vertebral fractures (Table 1 ▶) and about their interest in follow-up. Follow-up consisted of a heel BMD measurement by the dual x-ray and laser technique (DXL Calscan bone densitometer, Demetech, Täby, Sweden),16 beginning at the end of 2003, and home visits by nurses during 2003 and 2004. If women reported a vertebral fracture diagnosed by radiograph, we classified the fracture as a previous fragility fracture.
Risk Models and Ascertainment of Fractures and Mortality
We tested 2 models for risk assessment. Risk model 1 included 4 predefined factors: age 80 years or older, weight less than 60 kg, previous fragility fracture, and need to use arms to rise from the sitting position. Risk model 2 included the same risk factors, except that need to use arms to rise was replaced by falls during the last 12 months. For both models, we compared women with at least 2 of 4 risk factors with women with 0 or 1 risk factor. We tested each model as a predictor of future hip fracture, fragility fracture, and total mortality during a 2-year period, both in the whole population and in subpopulations.
We defined new fragility fractures as fractures occurring in the hip, wrist, proximal humerus, pubic bone, ischial bone, and vertebrae during 2002–2003. Vertebral fractures were classified as new if the radiograph report confirmed vertebral compression in women who had local pain. We thoroughly identified all incident fractures using diagnosis registers from the departments of orthopedics and geriatrics and using radiograph reports. We used ICD-10 (International Classification of Diseases, 10th Revision) diagnostic codes, specifically codes S72.00-72.21, S52.50-51, S42.20–21, S32.50, S32.80, S22.00, and S32.00, for the Vislanda and Tingsryd populations. Outpatient care registers were incomplete for the Emmaboda population; therefore, we documented only hip fractures (ICD-10 codes S72.00–72.21) for this population. We ascertained mortality in the study population by using data from the National Swedish Population Register.
Statistical Analysis
We calculated odds ratios (ORs) and hazard ratios (HRs) with logistic and Cox regression analysis for variables with cell values greater than 4. In the predefined risk models, women with missing data were recoded as having a low fracture risk to avoid overestimating the risks, while still evaluating the remaining risk factors for all participants. We used the Fisher exact test or the χ2 test to compare binary variables between 2 independent groups; variables with cell values of less than 5 were analyzed with the Fisher test only. We used the t test or Wilcoxon test for continuous symmetric or skewed variables. Kaplan-Meier curves were compared by the Breslow test. The areas under the receiver operating characteristic (ROC) curves were calculated for the risk models as binary or as predicted probabilities, as one measure of risk model discrimination. We regarded 2-sided P values of less than .05 to be significant and used exact tests whenever possible. We used the statistical programs SPSS 13.0 (Statistical Package for the Social Sciences; SPSS Inc, Chicago, Ill) and Epi Info 6.0 (Centers for Disease Control and Prevention, Atlanta, Ga).
RESULTS
Response Rate and Baseline Characteristics
The response rate to the questionnaire was 83%. The 250 nonrespondents (17%) were 3.4 years older than the respondents (P <.001).
The response rates for individual questions and the baseline characteristics of respondents are given in Table 2 ▶. The 1,248 women included in analyses ranged in age from 70 to 100 years (mean, 78.8 years). Ten percent lived in residential care.
Table 2.
Response Rates and Distributions for 19 Possible Risk Factors in the Questionnaire Completed by Women Aged =70 Years in 2001 (N = 1,248)
| Characteristic | Response Rate No. (%) | Study Population No. or Mean Value* | %† |
| Continuous risk factors | |||
| Age, y | 1,248 (100.0) | 78.8 ± 6.5 | – |
| Weight, kg | 1,214 (97.2) | 67.3 ± 11.8 | – |
| Height, cm | 1,213 (97.1) | 161 ± 6.1 | – |
| Dairy calcium intake, mg/d | 1,208 (96.7) | 628 ± 292 | – |
| Predefined risk factors | |||
| Age, y | |||
| 70–74 | 1,248 (100.0) | 377 | 30.2 |
| 75–79 | 1,248 (100.0) | 382 | 30.6 |
| 80–84 | 1,248 (100.0) | 236 | 18.9 |
| 85–89 | 1,248 (100.0) | 156 | 12.5 |
| 90–100 | 1,248 (100.0) | 97 | 7.8 |
| Weight <60 kg | 1,214 (97.2) | 302 | 24.9 |
| Fragility fracture after age 40 y‡,§ | 1,205 (96.6) | 398 | 33.0 |
| Uses arms when rising 5 times from chair | 1,210 (97.0) | 362 | 29.9 |
| Fell during last 12 mo | 1,192 (95.4) | 397 | 33.3 |
| Other possible risk factors | |||
| Any type of fracture after age 40 y§ | 1,210 (97.0) | 486 | 40.2 |
| Use of cortisone medication for >3 mo | 1,158 (92.7) | 149 | 12.9 |
| Has never given birth | 1,238 (99.1) | 164 | 13.2 |
| Lives in residential care (vs community) | 1,231 (98.6) | 123 | 10.0 |
| Height >167 cm | 1,213 (97.1) | 183 | 15.1 |
| Dairy calcium intake <500 mg/d | 1,208 (96.7) | 377 | 31.2 |
| Impaired vision, self-reported (vs good vision) | 1,226 (98.2) | 356 | 29.0 |
| History of maternal hip fracture | 1,108 (88.7) | 123 | 11.1 |
| Subjective health poor (vs excellent or fair) | 1,224 (98.0) | 120 | 9.8 |
| Current smoking | 1,231 (98.6) | 53 | 4.3 |
| Daily coffee intake ≥ 2 cups (vs 0-1 cup) | 1,233 (98.7) | 1,040 | 84.3 |
| Menopausal age <45 y | 1,072 (85.8) | 128 | 11.9 |
| No daily medication|| | 1,229 (98.4) | 152 | 12.4 |
| Any parent of non-Nordic origin (vs Nordic)|| | 1,226 (98.2) | 23 | 1.9 |
* Mean value is given as arithmetic mean ± SD.
† Estimated percentage for participants with valid data for that measure.
‡ Previous fragility fracture in hip, lower arm, upper arm, or vertebrae after age 40 years.
§ Only the Vislanda population was asked the additional question about vertebral radiographs.
|| This subgroup expected to have lower fracture risk.
Response rates for the 5 predefined risk factors included in the risk models averaged 97% (range, 95%–100%). Only 3 risk factor questions had a response rate of less than 95%.
One third (33%) of the study population reported having falls during the last 12 months, and 40% reported experiencing fractures after the age of 40. Each of the 5 predefined risk factors was found in 25% to 39% of the participants.
Risk Factors for Hip Fracture
Thirty-one women experienced at least 1 hip fracture during the study period, a cumulative annual incidence of 1.2%. This incidence did not differ between the Vislanda and the remaining districts studied (P = .38).
Compared with women who did not experience hip fractures, women who did were 4.2 years older (82.9 vs 78.7 years), weighed 6.8 kg less (60.7 vs 67.5 kg), and had a higher mean number of previous fragility fractures (0.84 vs 0.54 fractures) (P <.01 for each comparison).
In univariate Cox regression analysis, 4 of the 5 predefined risk factors were associated with an increased risk of hip fracture (Table 3 ▶). Of the remaining 14 risk factors, 4 were associated with an increased hip fracture risk (any type of fracture, use of cortisone medication, nulliparity, and living in residential care). After adjustment for age as a continuous variable, the factors still significantly associated with the risk of hip fracture were a low body weight (HR = 2.4; 95% confidence interval [CI], 1.2–5.0), previous fragility fracture (HR = 2.2; 95% CI, 1.1–4.4), and any type of fracture (HR = 2.1; 95% CI, 1.0–4.4).
Table 3.
Two-Year Hip Fracture Risk According to Clinical Risk Factors Among Women Aged 70-100 Years in 2001 (N = 1,248)
| Characteristic | Hip Fracture (n = 31)No. (%)* | No Hip Fracture (n = 1,217)No. (%)* | P Exact† | Univariate‡ HR (95% CI) | Multivariate‡ 4 Risk Factors HR (95% CI) | Multivariate‡,§ 11 Risk Factors HR (95% CI) |
| Predefined risk factors | ||||||
| Age 80–100 y | 19 (61) | 470 (39) | .01|| | 2.7 (1.3–5.6)|| | 2.2 (0.99–4.7) | 2.0 (0.9–4.7) |
| Weight <60 kg | 15 (48) | 287 (24) | .005|| | 3.1 (1.5–6.2)|| | 2.4 (1.2–5.0)|| | 2.6 (1.2–5.8)|| |
| Fragility fracture after age 40 y¶,# | 17 (55) | 381 (32) | .01|| | 2.5 (1.3–5.2)|| | 2.3 (1.1–4.7)|| | 2.6 (1.2–5.6)|| |
| Uses arms when rising 5 times from chair | 14 (47) | 348 (30) | .07 | 2.3 (1.1–4.7)|| | 1.7 (0.8–3.6) | 1.5 (0.6–3.7) |
| Fell during last 12 mo | 12 (41) | 385 (33) | .42 | 1.5 (0.7–3.1) | — | 1.0 (0.4–2.3) |
| Other possible risk factors | ||||||
| Any type of fracture after age 40 y# | 19 (61) | 468 (40) | .02|| | 2.4 (1.7–5.0)|| | — | — |
| Use of cortisone medication for >3 mo | 7 (26) | 142 (13) | .07 | 2.4 (1.0–5.6)|| | — | 2.6 (1.1–6.3)|| |
| Has never given birth | 8 (26) | 156 (13) | .054 | 2.4 (1.1–5.4)|| | — | 2.4 (1.0–5.6) |
| Lives in residential care (vs community) | 7 (23) | 116 (10) | .03|| | 3.3 (1.4–7.8)|| | — | 1.8 (0.6–5.0) |
| Height >167 cm | 5 (17) | 178 (15) | .80 | 1.1 (0.4–2.9) | — | 1.2 (0.4–3.5) |
| Dairy calcium intake <500 mg/d | 9 (31) | 368 (31) | 1.00 | 1.0 (0.5–2.2) | — | 1.0 (0.4–2.2) |
| Impaired vision, self-reported (vs good vision) | 8 (26) | 348 (29) | .84 | 0.9 (0.4–2.0) | — | 0.5 (0.2–1.3) |
| History of maternal hip fracture | 4 (15) | 119 (11) | .52 | — | — | — |
| Subjective health poor (vs excellent or fair) | 1 (3) | 119 (10) | .36 | — | — | — |
| Current smoking | 0 (0) | 53 (4) | .64 | — | — | — |
| Daily coffee intake ≥2 cups (vs 0–1 cup) | 28 (93) | 1,010 (84) | .21 | — | — | — |
| Menopausal age <45 y | 4 (18) | 124 (12) | .32 | — | — | — |
| No daily medication** | 2 (6) | 150 (12) | .42 | — | — | — |
| Any parent of non-Nordic origin (vs Nordic)** | 2 (7) | 21 (2) | .10 | — | — | — |
HR = hazard ratio; CI = confidence interval.
* Estimated percentage of participants with valid data for that measure.
† Exact P value according to the Fisher exact test, 2-sided.
‡ Cox regression analysis (for time alive before hip fracture) for participants with valid data and only for variables with cell values greater than 4.
§ The variable “any type of fracture” was excluded from multivariate analysis because it competed with and was highly correlated with “previous fragility fracture.”
|| P <.05
¶ Previous fragility fracture in the hip, lower arm, upper arm, or vertebrae after age 40 years.
# Reported vertebral fractures included from responses to the question about radiographs posed only to the Vislanda population.
** This subgroup had a lower fracture risk in previous studies.
After multiple Cox regression analysis of the 4 predefined risk factors that were significant predictors in univariate analysis, low body weight and previous fragility fracture remained significant predictors (Table 3 ▶). Use of cortisone medication was also a significant predictor when the multiple analysis was based on 11 risk factors.
The predefined risk factors for hip fracture also predicted all-cause mortality in this cohort (Table 4 ▶). Four women (13%) died within 1 year after their hip fracture. During 2003, the corresponding 1-year mortality for women who did not experience an incident hip fracture was 6% (OR = 2.5; 95% CI, 0.7–7.7).
Table 4.
Hip Fracture, Fragility Fracture, or Death Within 2 Years, Predicted by 2 to 4 vs 0 to 1 Risk Factors, According to Risk Model
| Total Population (N = 1,248) | |||||||||
| Risk Model | Total N | Events n | No Events n | NPV/PPV (%) | Specificity/Sensitivity (%) | Odds Ratio (95% CI) | P Exact | Vislanda (n = 435)P Exact | Tingsryd & Emmaboda (n = 418& 395)P Exact |
| Risk model 1 (FRAMO Index): Age, weight, previous fragility fracture,*† and using arms to rise | |||||||||
| Hip fractures | |||||||||
| 0–1 risk factor | 789 | 6 | 783 | 99.2/5.4 | 64/81 | 1.0 | <.001‡ | <.001‡ | .002§ |
| 2–4 risk factors | 459 | 25 | 434 | 7.5 (3.0–18.4)‡ | |||||
| Fragility fractures||,¶ | |||||||||
| 0–1 risk factor | 547 | 9 | 538 | 98.4/10.0 | 66/78 | 1.0 | <.001‡ | <.001‡ | .001§ |
| 2–4 risk factors | 306 | 31 | 275 | 6.7 (3.2–14.3)‡ | |||||
| Mortality | |||||||||
| 0–1 risk factor | 789 | 25 | 764 | 96.8/24.0 | 67/81 | 1.0 | <.001‡ | <.001‡ | <.001‡ |
| 2–4 risk factors | 459 | 109 | 350 | 9.5 (6.0–14.9)‡ | |||||
| Risk model 2: Age, weight, previous fragility fracture,*† and fall | |||||||||
| Hip fractures | |||||||||
| 0–1 risk factor | 775 | 9 | 766 | 98.8/4.7 | 63/71 | 1.0 | <.001‡ | .001§ | .052 |
| 2–4 risk factors | 473 | 22 | 451 | 4.1 (1.9–9.1)‡ | |||||
| Fragility fractures||,¶ | |||||||||
| 0–1 risk factor | 537 | 12 | 525 | 97.8/8.9 | 65/70 | 1.0 | <.001‡ | <.001‡ | .04# |
| 2–4 risk factors | 316 | 28 | 288 | 4.2 (2.1–8.5)‡ | |||||
| Mortality | |||||||||
| 0–1 risk factor | 775 | 35 | 740 | 95.5/21.0 | 66/74 | <.001‡ | <.001‡ | <.001‡ | |
| 2–4 risk factors | 473 | 99 | 374 | 5.6 (3.7–8.4)‡ | |||||
NPV = negative predictive value; PPV = positive predictive value; CI = confidence interval; FRAMO = Fracture and Mortality.
Note: Hypothesis tested by the Fisher exact test. Risk model 1 (FRAMO Index): age =80 years, weight <60 kg, previous fragility fracture, and using arms when rising at least 5 times from sitting position.*† Risk model 2: age =80 years, weight <60 kg, previous fragility fracture, and falls during the past 12 months. Women with missing data were recoded as having a low fracture risk; therefore, data for all 1,248 women were included in the Fisher exact 2-sided test and the binary logistic regression analysis.
* Previous fragility fractures: fractures in the hip, lower arm, upper arm, or vertebrae after age 40 years.
† Included reported vertebral fractures from responses to the radiograph question in the Vislanda population.
‡ P <.001.
§ P <.01.
|| Fragility fractures: fractures of the hip, distal radius, proximal humerus, pubic bone, ischial bone, or vertebrae during 2002–2003. ¶ Data for all types of fragility fractures were obtained only for the Vislanda and Tingsryd populations (n = 853).
# P <.05.
Assessment of Fracture and Mortality Risk
The total annual mortality rate was 5.4% in this study population, and 134 women died during 2002–2003.
The associations between the 5 main risk factors according to the 2 predefined risk models and outcomes are shown in Table 4 ▶. Both models significantly predicted hip fracture, fragility fracture, and mortality for the whole population, but risk model 1 had higher ORs (Table 4 ▶). In further analyses, we applied risk model 1, renamed the Fracture and Mortality (FRAMO) Index, to all 1,248 participants.
The FRAMO Index was strongly associated with hip fracture, fragility fracture, and mortality risk within 2 years, with ORs of 7.5, 6.7, and 9.5, respectively (Table 4 ▶ and Figure 1 ▶). All lower limits of the 95% CIs were 3.0 or higher for these 3 ORs.
Figure 1.
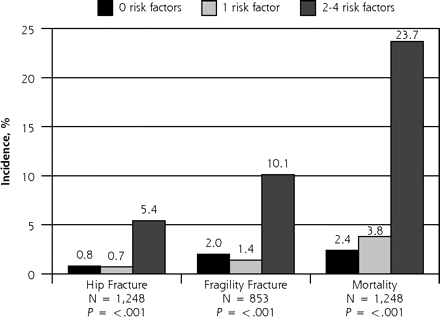
Two-year cumulative incidence of hip fracture, fragility fracture, and total mortality, divided into tertiles of women with 0, 1, or 2 to 4 risk factors.
Note: Risk assessment with 0, 1, or 2 to 4 risk factors among age =80 years, weight <60 kg, previous fragility fracture, and using arms to rise. The proportions of women with 0, 1, and 2 to 4 risk factors were 30%, 34%, and 37%, respectively.
Even when adjusted for age as a continuous variable in multivariate logistic regression analysis, the FRAMO Index had an OR of 6.8 (95% CI, 2.4–19.5) for hip fracture and an OR of 4.3 (95% CI, 2.5–7.4) for mortality. The crude FRAMO Index predicted 2-year hip fracture risk with 81% sensitivity and 64% specificity. Its sensitivity and specificity for predicting mortality were 81% and 67%, respectively. For the low-risk group (0 to 1 risk factor), which comprised 63% of the whole study population, the absolute risks of any hip fracture and of death were only 0.8% and 3.2%, respectively (Figure 1 ▶). The corresponding risks for the high-risk group (2 to 4 risk factors) were 5.4% and 23.7%. Mortality increased significantly with the number of risk factors (Figure 2 ▶). The risk of hip fracture during the 2-year study period for the 2 risk groups is shown in Figure 3 ▶.
Figure 2.
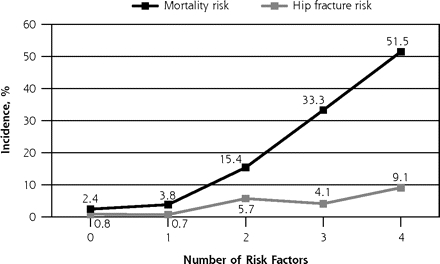
Two-year cumulative incidence of hip fracture and total mortality according to number of risk factors.
Note: Hip fracture and total mortality for women with 0, 1, 2, 3, or 4 risk factors among age =80 years, weight <60 kg, previous fragility fracture, and using arms to rise. The proportions of women in these groups were 30%, 34%, 22%, 12%, and 3%, respectively.
Figure 3.
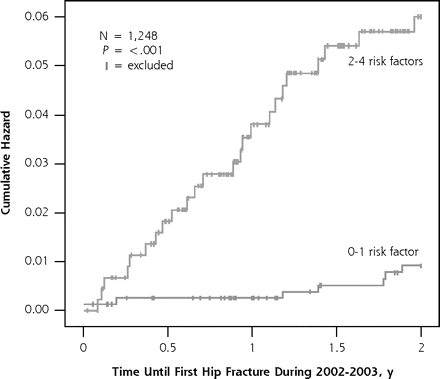
FRAMO Index 2-year cumulative hazard for hip fracture.
FRAMO = Fracture and Mortality.
Note: In these Kaplan-Meier curves, women were excluded after death or first hip fracture.
We defined in advance the high-risk threshold values for age and weight in the FRAMO Index and its application to create 2 risk groups (0–1 vs 2–4 risk factors). These levels proved appropriate, yielding an area under the ROC curve of 0.72 (95% CI, 0.64–0.81) for hip fracture and 0.75 (95% CI, 0.71–0.79) for mortality when all 1,248 women were analyzed. When the 4 risk factors were weighted (using continuous age and the risk factors’ logistic regression coefficients), the area under the curve for hip fracture increased only slightly and nonsignificantly, to 0.75 (P = .66). We chose the unweighted index because it is so easily calculated.
Reported Vertebral Fracture
The questionnaire given to all women included multiple-choice questions concerning different types of fractures occurring after the age of 40. An additional question about previous vertebral radiographs was sent only to the Vislanda population. Fully 10.0% of women from this district reported vertebral fractures, compared with 4.3% of the women from the other 2 districts (Tingsryd and Emmaboda) combined (P <.001). When the FRAMO Index was applied to the Vislanda population only, its sensitivity for hip fracture was 92%. The index yielded an area under the ROC curve of 0.78 for hip fracture in this population, compared with 0.68 in the remaining women, a non-significant difference (P = .20).
DISCUSSION
Main Findings
We validated a very simple clinical risk model in a representative cohort of 1,248 women aged 70 years or older in 3 Swedish primary care populations. Eighty-three percent of this elderly population, which included women in residential care, responded to the questionnaire. The FRAMO Index consists of only 4 simply worded questions with yes/no answers, yet it predicts hip fractures as well as more complex risk scoring systems. We found that a majority of women (63%) had 0 or 1 risk factor, which was associated with very low absolute risks of hip fracture and total mortality within 2 years (0.8% and 3.2%, respectively). In contrast, the predicted hip fracture risk was more than 7-fold greater for the 37% of women with at least 2 risk factors. Their risk for all types of fragility fractures was also increased. The mortality risk was more than 9-fold greater for women with the higher FRAMO Index score, and mortality increased steadily with the number of risk factors. After the FRAMO Index was adjusted for age, the risk estimates were still significant. Finally, we found that including a specific question about vertebral radiographs improved the reporting of previous vertebral fractures, which is an important predictor of future fractures13 and improves the sensitivity of the index.
Limitations
Although this study was small and few fractures occurred, the lower limits of the 95% CIs for the ORs were at least 3.0 for the FRAMO Index. Because the number of incident fractures was small, only 3 individual risk factors remained significant predictors in univariate analysis after adjustment for age. Although the response rate was high, the 17% of women who were nonrespondents were somewhat older than respondents. This pattern probably decreased the actual risk estimates somewhat, because hip fractures become more common with age.
The observation period in this study was only 2 years. Because the FRAMO Index is simple and binary, with only yes/ no responses possible, this index is easy to repeat during regular consultation in primary care, even without use of the written questionnaire. Age as a binary variable may become less predictive during a longer observation period.
The number of fragility fractures that occurred during the study period was slightly underestimated. Hip, arm, and pelvic fractures are usually detected by radiographs, but not all women experiencing vertebral fractures are evaluated and given radiographic diagnoses.
This study was limited to white, rural, Swedish female populations, nearly all of whom (98%) had parents of Nordic origin. Urban women, who have a higher fracture risk, more often have a history of fracture and are less physically active.17,18 Because these factors might be reflected in the index items of previous fragility fracture and using arms to rise, the index may also be suitable for fracture prediction in urban populations.
Further Studies
This study needs to be replicated in larger, non-Scandinavian, urban populations and possibly among both sexes (with modified variables for men), to obtain more precise fracture risk estimates. Also, the observation period should be extended. BMD measurement may improve the risk model, and the role of BMD in choosing strategies for fracture prevention can be more clearly defined. More information is needed to define different preventive treatments for different levels of risk.
Comparison With Other Studies
The age-adjusted ORs we observed for low weight and any type of previous fracture were similar to those in earlier studies.5,10 Despite the use of only 4 clinical risk factors applied in a strict binary fashion in our FRAMO Index, its sensitivity and specificity for 2-year hip fracture incidence were on par with those of previous studies with more complicated risk scoring.5,8,11
Similar risk factors have been used in other studies, in which scores for predicting the risk of hip fracture within 3, 4, or 5 years were created.4,5,11 In those studies, however, the variables of age or body weight were weighted, and a history of any type of fracture after age of 50 was used instead.
The SOF5 and the EPIDOS fracture study5 used a 7-item index. It included BMD as a significant independent predictor of the 5-year incidence of hip fracture. Inclusion of BMD increased the positive predictive value of that risk index slightly from 5.6% to 5.8%. The index was validated for use in community-based volunteers,5 in contrast to our index, which was evaluated among women selected from total population registers for primary care areas.
In the MOF study,11 the risk model used to predict hip fracture within 3 years was more complex than our FRAMO Index, and the participation rate (70%) was lower than that in our study (83%).
Implications
Our very simple FRAMO Index was useful in identifying older women at high risk for hip fracture, fragility fracture, and mortality. The high response rate to the questionnaire may indicate a high level of interest in fracture prevention among this elderly female population. Population-based fracture risk assessment, including women in residential care, may be feasible using this method. This simple risk index might easily be applied during an ordinary consultation in primary care, even without the use of the written questionnaire.
Of the independent predictors of hip fracture, such as impaired mobility, older age, previous fracture, or low BMD,4–6 all but age are possibly modifiable risk factors. We have included age as a risk indicator in the FRAMO Index because fracture prevention may be most effective in older women.9 For example, bisphosphonates have been used for fracture prevention among post-menopausal women with previous vertebral fracture and osteoporosis.19,20 The absolute risk reduction for fracture increases with age (from age 55 years up to age 75–85 years) with bisphosphonate therapy,9,21 which is more cost-effective at age 77 years than at age 65 years.22
Data on the predictive value of the combination of BMD with the FRAMO Index are not yet available. A high FRAMO Index, like other clinical scores that include age, low weight, and previous fragility fracture, may identify women with osteoporosis; therefore, these 3 items have been used to select women for BMD testing.12,23,24 BMD assessment may delimit an even smaller group, at very high risk, who can derive more benefit from drugs to treat osteoporosis.4,5,21
Even more accurately, the FRAMO Index identifies a majority of women aged 70 years or older with minimal fracture or mortality risk who therefore have less of a need for fracture prevention interventions. For these women, BMD assessment may be unnecessary; according to the findings of the study by Cummings et al,4 women with few clinical risk factors are less likely to experience hip fracture, even if they are in the group with the lowest one third of BMD values.4
For postmenopausal women at all risk levels, clinicians should encourage basic lifestyle modifications to prevent fractures, such as regular physical activity, smoking cessation, and good nutrition, including adequate intakes of calcium and vitamin D.25–28 When the FRAMO Index shows that a patient is at high risk for fracture, several interventions may be valuable. Physical training may improve the ability to rise from sitting,29 and smoking cessation, walking outdoors, and daily physical activity are recommended.25,26,30,31 Training improves muscle strength and mobility, which may reduce the number of falls.29,32,33 Also, a safer home environment and discontinuation of unnecessary psychotropic medication could reduce the tendency to fall.34–36 Hip protectors may prevent hip fracture among elderly individuals in institutional care.37 Clinicians should also consider pharmaco-logic treatment with calcium and vitamin D338–43 and bisphosphonates.13,19,21,28,44,45
Because hip or spinal fracture itself increases the risk of mortality,46 preventing fractures may prolong life. Women with several risk factors who sustain hip fractures probably also require longer rehabilitation and have even shorter survival. This pattern might in turn warrant more active fracture prevention in this group.
The FRAMO Index, validated in this study, might be a practical fracture and survival assessment tool for clinicians to use during routine consultations.
Acknowledgments
Statistician Anna Lindgren provided substantial assistance with the statistical calculations.
Conflicts of interest: none reported
Funding support: This study received financial and material support from the R&D Center, Kronoberg County Council, Växjö.
REFERENCES
- 1.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7(5):407–413. [DOI] [PubMed] [Google Scholar]
- 2.Kanis JA, Johnell O, Oden A, et al. Risk of hip fracture derived from relative risks: an analysis applied to the population of Sweden. Osteoporos Int. 2000;11(2):120–127. [DOI] [PubMed] [Google Scholar]
- 3.Sernbo I, Johnell O. Consequences of a hip fracture: a prospective study over 1 year. Osteoporos Int. 1993;3(3):148–153. [DOI] [PubMed] [Google Scholar]
- 4.Cummings SR, Nevitt MC, Browner WS, et al. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med. 1995;332(12):767–773. [DOI] [PubMed] [Google Scholar]
- 5.Black DM, Steinbuch M, Palermo L, et al. An assessment tool for predicting fracture risk in postmenopausal women. Osteoporos Int. 2001;12(7):519–528. [DOI] [PubMed] [Google Scholar]
- 6.Dargent-Molina P, Favier F, Grandjean H, et al. Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet. 1996;348(9021):145–149. [DOI] [PubMed] [Google Scholar]
- 7.Taylor BC, Schreiner PJ, Stone KL, et al. Long-term prediction of incident hip fracture risk in elderly white women: Study of Osteoporotic Fractures. J Am Geriatr Soc. 2004;52(9):1479–1486. [DOI] [PubMed] [Google Scholar]
- 8.De Laet CE, Van Hout BA, Burger H, et al. Hip fracture prediction in elderly men and women: validation in the Rotterdam study. J Bone Miner Res. 1998;13(10):1587–1593. [DOI] [PubMed] [Google Scholar]
- 9.De Laet CE, van Hout BA, Burger H, Hofman A, Pols HA. Bone density and risk of hip fracture in men and women: cross sectional analysis. BMJ. 1997;315(7102):221–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kanis JA, Johnell O, De Laet C, et al. A meta-analysis of previous fracture and subsequent fracture risk. Bone. 2004;35(2):375–382. [DOI] [PubMed] [Google Scholar]
- 11.McGrother CW, Donaldson MM, Clayton D, Abrams KR, Clarke M. Evaluation of a hip fracture risk score for assessing elderly women: the Melton Osteoporotic Fracture (MOF) study. Osteoporos Int. 2002;13(1):89–96. [DOI] [PubMed] [Google Scholar]
- 12.Dargent-Molina P, Poitiers F, Breart G. In elderly women weight is the best predictor of a very low bone mineral density: evidence from the EPIDOS study. Osteoporos Int. 2000;11(10):881–888. [DOI] [PubMed] [Google Scholar]
- 13.Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15(4):721–739. [DOI] [PubMed] [Google Scholar]
- 14.Gunnes M, Mellstrom D, Johnell O. How well can a previous fracture indicate a new fracture? A questionnaire study of 29,802 post-menopausal women. Acta Orthop Scand. 1998;69(5):508–512. [DOI] [PubMed] [Google Scholar]
- 15.Albertsson D, Mellström D, Eggertsen R. Risk group for hip fracture in elderly women identified by primary care questionnaire—clinical implications. Ups J Med Sci. 2006;111(2):179–187. [DOI] [PubMed] [Google Scholar]
- 16.Kullenberg R. Reference database for dual X-ray and laser Calscan bone densitometer. J Clin Densitom. 2003;6(4):367–372. [DOI] [PubMed] [Google Scholar]
- 17.Jonsson B, Gardsell P, Johnell O, Redlund-Johnell I, Sernbo I. Differences in fracture pattern between an urban and a rural population: a comparative population-based study in southern Sweden. Osteoporos Int. 1992;2(6):269–273. [DOI] [PubMed] [Google Scholar]
- 18.Jonsson B, Gardsell P, Johnell O, Sernbo I, Gullberg B. Life-style and different fracture prevalence: a cross-sectional comparative population-based study. Calcif Tissue Int. 1993;52(6):425–433. [DOI] [PubMed] [Google Scholar]
- 19.Ensrud KE, Black DM, Palermo L, et al. Treatment with alendronate prevents fractures in women at highest risk: results from the Fracture Intervention Trial. Arch Intern Med. 1997;157(22):2617–2624. [PubMed] [Google Scholar]
- 20.Cummings SR, Black DM, Thompson DE, et al. Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention Trial. JAMA. 1998;280(24):2077–2082. [DOI] [PubMed] [Google Scholar]
- 21.Hochberg MC, Thompson DE, Black DM, et al. Effect of alendronate on the age-specific incidence of symptomatic osteoporotic fractures. J Bone Miner Res. 2005;20(6):971–976. [DOI] [PubMed] [Google Scholar]
- 22.Johnell O, Jonsson B, Jonsson L, Black D. Cost effectiveness of alendronate (Fosamax) for the treatment of osteoporosis and prevention of fractures. Pharmacoeconomics. 2003;21(5):305–314. [DOI] [PubMed] [Google Scholar]
- 23.Wehren LE, Siris ES. Beyond bone mineral density: can existing clinical risk assessment instruments identify women at increased risk of osteoporosis? J Intern Med. 2004;256(5):375–380. [DOI] [PubMed] [Google Scholar]
- 24.Bauer DC, Browner WS, Cauley JA, et al. Factors associated with appendicular bone mass in older women. The Study of Osteoporotic Fractures Research Group. Ann Intern Med. 1993;118(9):657–665. [DOI] [PubMed] [Google Scholar]
- 25.Paganini-Hill A, Chao A, Ross RK, Henderson BE. Exercise and other factors in the prevention of hip fracture: the Leisure World study. Epidemiology. 1991;2(1):16–25. [DOI] [PubMed] [Google Scholar]
- 26.Feskanich D, Willett W, Colditz G. Walking and leisure-time activity and risk of hip fracture in postmenopausal women. JAMA. 2002;288(18):2300–2306. [DOI] [PubMed] [Google Scholar]
- 27.Ringsberg KA, Gardsell P, Johnell O, Josefsson PO, Obrant KJ. The impact of long-term moderate physical activity on functional performance, bone mineral density and fracture incidence in elderly women. Gerontology. 2001;47(1):15–20. [DOI] [PubMed] [Google Scholar]
- 28.Wilkins CH, Birge SJ. Prevention of osteoporotic fractures in the elderly. Am J Med. 2005;118(11):1190–1195. [DOI] [PubMed] [Google Scholar]
- 29.Fiatarone MA, Marks EC, Ryan ND, et al. High-intensity strength training in nonagenarians. Effects on skeletal muscle. JAMA. 1990;263(22):3029–3034. [PubMed] [Google Scholar]
- 30.Law MR, Hackshaw AK. A meta-analysis of cigarette smoking, bone mineral density and risk of hip fracture: recognition of a major effect. BMJ. 1997;315(7112):841–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kanis JA, Johnell O, Oden A, et al. Smoking and fracture risk: a meta-analysis. Osteoporos Int. 2005;16(2):155–162. [DOI] [PubMed] [Google Scholar]
- 32.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. Falls prevention over 2 years: a randomized controlled trial in women 80 years and older. Age Ageing. 1999;28(6):513–518. [DOI] [PubMed] [Google Scholar]
- 33.Day L, Fildes B, Gordon I, et al. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ. 2002;325(7356):128–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cumming RG, Thomas M, Szonyi G, et al. Home visits by an occupational therapist for assessment and modification of environmental hazards: a randomized trial of falls prevention. J Am Geriatr Soc. 1999;47(12):1397–1402. [DOI] [PubMed] [Google Scholar]
- 35.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. Psychotropic medication withdrawal and a home-based exercise program to prevent falls: a randomized, controlled trial. J Am Geriatr Soc. 1999;47(7):850–853. [DOI] [PubMed] [Google Scholar]
- 36.Gillespie LD, Gillespie WJ, Robertson MC, et al. Interventions for preventing falls in elderly people. Cochrane Database Syst Rev. 2003;(4):CD000340. [DOI] [PubMed]
- 37.Lauritzen JB, Petersen MM, Lund B. Effect of external hip protectors on hip fractures. Lancet. 1993;341(8836):11–13. [DOI] [PubMed] [Google Scholar]
- 38.Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, et al. Effect of vitamin D on falls: a meta-analysis. JAMA. 2004;291(16):1999–2006. [DOI] [PubMed] [Google Scholar]
- 39.Dawson-Hughes B, Harris SS, Krall EA, Dallal GE. Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med. 1997;337(10):670–676. [DOI] [PubMed] [Google Scholar]
- 40.Chapuy MC, Arlot ME, Duboeuf F, et al. Vitamin D3 and calcium to prevent hip fractures in the elderly women. N Engl J Med. 1992;327(23):1637–1642. [DOI] [PubMed] [Google Scholar]
- 41.Trivedi DP, Doll R, Khaw KT. Effect of four monthly oral vitamin D3 (cholecalciferol) supplementation on fractures and mortality in men and women living in the community: randomised double blind controlled trial. BMJ. 2003;326(7387):469–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bischoff-Ferrari HA, Willett WC, Wong JB, et al. Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. JAMA. 2005;293(18):2257–2264. [DOI] [PubMed] [Google Scholar]
- 43.Larsen ER, Mosekilde L, Foldspang A. Vitamin D and calcium supplementation prevents osteoporotic fractures in elderly community dwelling residents: a pragmatic population-based 3-year intervention study. J Bone Miner Res. 2004;19(3):370–378. [DOI] [PubMed] [Google Scholar]
- 44.Kanis JA, Black D, Cooper C, et al. A new approach to the development of assessment guidelines for osteoporosis. Osteoporos Int. 2002;13(7):527–536. [DOI] [PubMed] [Google Scholar]
- 45.Black DM, Thompson DE, Bauer DC, et al. Fracture risk reduction with alendronate in women with osteoporosis: the Fracture Intervention Trial. FIT Research Group. J Clin Endocrinol Metab. 2000;85(11):4118–4124. [DOI] [PubMed] [Google Scholar]
- 46.Johnell O, Kanis JA, Oden A, et al. Mortality after osteoporotic fractures. Osteoporos Int. 2004;15(1):38–42. [DOI] [PubMed] [Google Scholar]


