Summary
Introduction
The prevalence of hypertension ranges between 10 to 20% in Nigeria. Studies elsewhere have revealed left ventricular diastolic dysfunction to be highly prevalent in hypertension.
Objective
To evaluate the prevalence of diastolic dysfunction in adult hypertensive Nigerians.
Patients and Methods
One hundred and five (105) hypertensive patients, with ages ranging from 18 to 85 years, were enrolled between November 1998 and January 2000. These were divided into 3 groups of 35 each, according to levels of diastolic blood pressure as mild, moderate and severe hypertension. The weight, height, body surface area, body mass index, heart rate and systolic as well as diastolic blood pressures were checked. They were all investigated with M-mode, two-dimensional and pulsed Doppler echocardiographic techniques.
Results
Diastolic dysfunction was found in 82.86% (87) of the 105 hypertensive patients (P<0.0001). Twenty six (74.29%) of the 35 mildly hypertensive; 28 (80%) of the moderately hypertensive, and 33 (94.29%) of the severely hypertensive patients had diastolic dysfunction. This is as compared to only 12(34.29%) of the 35 normotensive patients who had diastolic dysfunction.
Conclusion
The findings from the study show that diastolic dysfunction is highly prevalent in unselected adult Nigerian patients with primary hypertension. This result is in keeping with, and even outstrips, the findings in other related works.
It is recommended from this study, that as much as practicable, hypertensive patients be evaluated with Doppler echocardiogram in order to detect the early effects of hypertension on the heart, especially as represented by diastolic dysfunction, with a view to affecting the management outcome.
Keywords: Prevalence, diastolic dysfunction, hypertensive Nigerians
Introduction
The prevalence of hypertension in adults all over the world, using the cut off of 160/95mmHg as at 1984 was estimated at 10 to 16%1. By now, with the adoption of 140/90mmHg, the prevalence is obviously much higher! As at 1972, Akinkugbe had put the prevalence in the adult African population as 10 to 15%2. Ahren and Mutembei had established this as 9.2% in Tanzania by 19843, while Cooper and Rotimi had an estimated standard prevalence of 14% for West Africa4.
Many studies have been done in various areas of Nigeria involving specific subsections of the population on the prevalence hypertension. In 1965 Ikeme documented the prevalence of hypertension in the cardiovascular clinic of the University College Hospital, Ibadan, as 28%5. Osilesi et al6, in a review, had an estimated prevalence of 15%, while Abengowe, in a survey in the adult population of Northern Nigeria in 1987 had a prevalence of 10%7. Similar work at the University of Nigeria Teaching Hospital, Enugu, by Onwubere and Ike, yielded a 15.2% prevalence8.
A survey by the expert committee on non communicable diseases in Nigeria revealed the prevalence of hypertension in adult Nigerians aged 15 years and above, to be 11.2%, (4.33 million) using 160/95mmHg as the cut off, with rates in the rural and urban communities of 9.8% and 14.6% respectively9. Adjusting these, with the cut-off point of 140/90mmHg, these results would lead to a current prevalence rate of 17 to 20% (7.8million)10.
Left ventricular diastolic dysfunction is the first discernible manifestation of heart disease in hypertensive patients11,12. Pulsed Doppler transmitral echocardiography can detect left ventricular (diastolic) filling abnormalities in patients with hypertension even before any clinical or electrocardiographic abnormalities are present13,14.
The diastolic phase of the cardiac cycle is divided into the isovolumic relaxation period and three filling phases. These filling phases include the rapid filling (diastasis) and atrial filling. The highest velocity during the early rapid filling period is what is recorded in Pulsed-wave transmitral Doppler tracing as the E wave velocity, while the highest velocity during the atrial contraction (late filling) period is traced as the A wave velocity. The A:E ratio, which is the index for diastolic dysfunction, is calculated/derived from the ratio of the peak atrial filling velocity to the peak early ventricular filling velocity. In normal situations the A:E ratio is less than 1. In diastolic dysfunction the A:E ratio is equal to or greater than 115,16. The prevalence of left ventricular diastolic dysfunction in hypertension has been well documented. This ranges from 46 to 68% in various works in Caucasians17–20.
Subjects and Methods
The study group was drawn from consecutive hypertensive patients attending the medical out patients (MOP) and Cardiac clinics of the University of Nigeria Teaching Hospital (UNTH), Enugu. All adult patients, of both sexes, newly diagnosed to have primary hypertension and those who have not been on antihypertensive treatment for at least two weeks prior to recruitment and who gave informed consent were included in the study.
Six hundred and ninety two (692) volunteers were recruited, over a period of fifteen months, from November 1998 to January 2000. One hundred and five (105) patients met the inclusion criteria which included:
Absence of clinical, electrocardiographic or echocardiographic evidence of secondary hypertension, valvular, congenital and ischaemic heart diseases, as well as diabetes mellitus, heart failure and renal diseases
Normal haematological and biochemical indices.
Primary hypertension was diagnosed in subjects showing diastolic blood pressure values ≥ 95mmHg using the WHO classification21,22 and the Nigerian Non-Communicable Diseases Expert Survey cut off point9, which were prevailing at the time the study. Blood pressure was evaluated on at least three separate visits, in lying position, and the average of the three readings was used for the study.
The patients were divided into 3 groups of 35 each according to levels of diastolic blood pressure.
Group I: diastolic blood pressure 96–104 mmHg
Group II: diastolic blood pressure 105–114 mmHg
Group III: diastolic blood pressure 115 mmHg and above
Thirty five healthy normotensive subjects, matched for age and sex, were also enrolled. These served as controls. They were chosen from medical students, hospital staff and other subjects undergoing clinical check up and found to be healthy.
Each subject underwent M-mode, two dimensional and Doppler echocardiography, with a Siemens Sonoline CD echocardiographic machine, equipped with a 3.5HZ transducer, a video recorder and print our processor. Left parasternal and the apical four chamber views were used as indicated.
Statistical Analysis: Data were expressed as mean and standard deviation. Comparisons between groups were performed using the analysis of variance (ANOVA). P values less than 0.05 were regarded as significant.
Ethical Approval: Clearance was obtained from the University of Nigeria Teaching Hospital ethical committee.
Results
During the fifteen month study period, a total of 692 patients were screened. One hundred and five of these met the inclusion criteria. Thirty-five controls mainly from the hospital workers and students, were also studied. The study population included 69 males and 71 females, their ages ranged from 18 to 85 years.
The clinical characteristics of the patient groups and normotensive controls are summarized in Table 1. No significant difference in age, body surface area, body mass index and heart rate was found among the subjects. As a result of the selection criteria, the systolic and diastolic blood pressures differed very significantly across the groups (P<0.0001).
Table 1.
Clinical characteristics of study population
| Parameter | Normotensive Subjects (N) |
Hypertensive Patients | ANOVA | ||||
| Mild(I) | Moderate(II) | Severe(III) | P value | F | R2 | ||
| Number | 35 | 35 | 35 | 35 | |||
| Sex (M/F) | 17/18 | 17/18 | 17/18 | 17/18 | |||
| Age (Years) | 43.46 (14.96) | 51.37 (14.96) | 54.23 (12.46) | 52.17 (10.37) | 0.5618 | 0.6969 | 0.0695 |
| BSA (m2) | 1.81 (0.18) | 1.79 (0.18) | 1.74 (0.19) | 1.75 (0.19) | 0.3073 | 1.214 | 0.0261 |
| BMI (Kg/m2) | 26.7 (5.07) | 27.43 (5.56) | 26.24 (4.14) | 26.14 (5.23) | 0.6959 | 0.4812 | 0.0105 |
| HR (beats/min) | 78.06 (11.12) | 81.46 (11.46) | 78.34 (10.84) | 86.34 (13.40) | 0.4109 | 0.9658 | 0.0209 |
| SBP (mmHg) | 123 (21) | 159 (21) | 172 (15) | 194 (23) | < 0.0001 | 50.75 | 0.5282 |
| DBP (mmHg) | 74 (7) | 99 (2) | 109 (2) | 124 (8) | < 0.0001 | 508.0 | 0.9181 |
Table 2 reveals that the A:E ratio (diastolic dysfunction index) was significantly different across all the subject groups (p<0.005; ANOVA). There was also a significant difference between the mean values of diastolic dysfunction index of A:E ratio in all the subject groups. These ranged from 0.94 in normotensive to 1.23 (mild), 1.27 (moderate) and 1.33 (severe), respectively.
Table 2.
Doppler measurements of study population
| Parameters | Normotensive Subjects (N) |
Hypertensive Patients | ANOVA | ||||
| I | II | III | P value | F | R2 | ||
| (E) (cm/s) | 61.77 (18.82) | 53.51 (16.88) | 52.34 (16.69) | 52.29 (14.14) | 0.4938 | 0.8038 | 0.0174 |
| (A) (cm/s) | 53.51 (16.78) | 61.71 (16.15) | 61.80 (14.09) | 66.97 (14.83) | 0.0048 | 4.507 | 0.0904 |
| A/E ratio | 0.94 (0.49) | 1.23 (0.41) | 1.27 (0.45) | 1.33 (0.33) | 0.0008 | 5.894 | 0.1151 |
Data presented represent mean for each group
Numbers in brackets =± Standard Deviation of the mean
A/E = Diastolic dysfunction index
E = Early ventricular (diastolic) filling
A= (Late) atrial contraction diastolic filling
Table 3 shows that 99 (70.7%) of the total study population had diastolic dysfunction. Diastolic dysfunction indices of A:E ratio ≥ 1 across the groups was statistically significant as shown in the table (chi square analysis: P value < 0.0001). Also as shown from the table, 12 (34.29%) of the 35 normotensive control group had diastolic dysfunction, as contrasted to 87 (82.86%) of the 105 hypertentsive subjects. The prevalence of the diastolic dysfunction progressively rose from mild (74.29%; 26 of 35), moderate (80%; 28 of 35 subjects), to 94.29% (33 of 35 subjects) in the severe hypertensive groups, respectively.
Table 3.
Chi-square analysis of diastolic dysfunction across the groups (using 2 x Y contingency table)
| Group | A/E ratio ≥ 1 |
A/E ratio < 1 |
Total |
| Normal | 12 | 23 | 35 |
| Mild | 26 | 9 | 35 |
| Moderate | 28 | 7 | 35 |
| Severe | 33 | 2 | 35 |
| Total | 99 | 41 | 140 |
X2 (Odds Ratio) =33.49
Df =3
P Value = 0.00000025
Statistically significant? Yes (P < 0.0001)
A/E = Diastolic dysfunction index
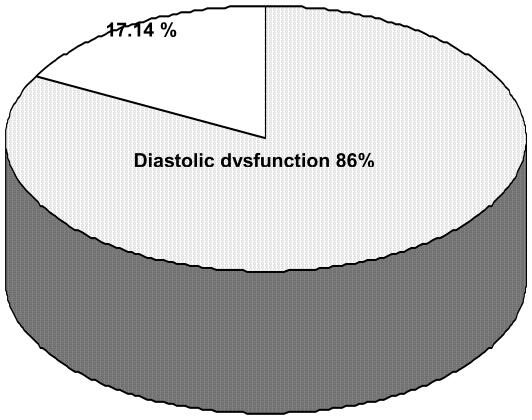
Figure 1 displays the proportion of diastolic dysfunction (A:E ratio ≥ 1) in all the hypertensive population. Eighty seven out of the 105 hypertensive patients studied (82.86%) had diastolic dysfunction.
Figure 1.
Total diastolic dysfunction (in hypertensive groups)
Discussion
The overall prevalence of diastolic dysfunction in the hypertensive groups in this study was 82.86%. This is as matched with the normotensive control, with 34.29%. This result is in keeping with, and even higher than findings in other studies17–19 in Europe (46%–48%).
The works of Kingue et al in Cameroon123, and Balogun and Co-workers in Nigeria24 earlier referred to, documented 67.4% and 58% prevalence, respectively.
However, Philips et al25 rather discovered abnormal left ventricular filling rates only in patients with systolic blood pressure (SBP) higher than 130mmHg, but not in those patients with SBP lower than 130mmHg. Contrariwise, Gardin et al26 in a study in a group of 21 mild hypertensive patients, found normal values of peak E velocity, peak A velocity and normal A:E ratio, with no diastolic dysfunction in the hypertensive group. This result has, however, been attributed to the fact that Gardin and his associates had relatively low blood pressures in the hypertensive group they studied (clinic blood pressure: 147.9/95.8mmHg; average 24 hours blood pressure: 137.1/83.2 mmHg).
It would be noted that the prevalence rate for the patients in Group I in our study (74.29%) approximated to those found in London by Mayet et al (68%)20 and Kingue et al in Cameroon (67.4%)23. This was with a mean diastolic blood pressure of 99 mmHg for these Group 1 patients. The greater proportion of the total 82.86% prevalence rate found in the study was contributed to by Group II (prevalence rate 94.29%; diastolic blood pressure 109mmHg) and Group III (prevalence rate 94.29%; mean diastolic blood pressure, 124mmHg) patients. This may suggest that the black population represented by the study have significantly more severe forms of hypertension than in the comparable study population especially in the Caucasians, as documented in literature.
The possibility that these patients may stay longer without treatment before presenting at the hospital, due to socioeconomic factors, as compared to their counterparts in other parts of the world with higher standard of living, may also offer a possible explanation27. Balogun et al24 had noted that cost in obtaining needed investigations in various cardiac diseases reduces access of those in the low socioeconomic class, who are quite many in Nigeria.
It is also observed that the study population had a comparatively higher rate than neighbouring Cameroon, with comparable number of patients studied (105 versus 98) and the same geo-racial setting. It could be argued that the higher prevalence of hypertension in the country of study (Nigeria)10 may partly contribute to the significantly increased prevalence rate of diastolic dysfunction among these hypertensive subjects. All these postulates lend themselves to further detailed study in future.
The main limitation of pulsed Doppler echocardiography, especially with regards to the A:E ratio, is that determination of diastolic function by this technique is imprecise. It permits only an indirect measure of diastolic function in relation to left ventricular filling, since it cannot assess all the factors influencing left ventricular diastolic filling directly, particularly the confounding physiological variables. Combined alterations of these influencing factors may actually “pseudonormalize” the transmitral flow pattern, thus complicating the evaluation of diastolic filling, especially with the presence of both prolonged relaxation and restrictive filling abnormalities15,28,29.
Conclusion
This study has shown that there is a high prevalence of left ventricular diastolic dysfunction in adult Nigerians with primary hypertension. This becomes of great importance, especially as until recently, left ventricular diastolic dysfunction was more often assumed than directly demonstrated in the presence of hypertensive conditions.
It is recommended from this study that hypertensive patients, as much as practicable, be evaluated with Doppler echocardiogram in order to detect the early effects of hypertension on the heart, especially as represented by diastolic dysfunction.
Acknowledgement
We wish to thank Dr. B.C. Anisiuba, for part of the echocardiography performance. We are also grateful to Dr. AU Mbah and Mr. Cletus Ude for their assistance with the computer analysis of the data, as well as all the subjects who willingly volunteered for this study. We are grateful to Miss Maureen Nwaeze for her secretarial assistance.
References
- 1.World Health Organization, author. Arterial Hypertension. Tech Rep Ser. 1984;628:9. [Google Scholar]
- 2.Akinkugbe OO. High blood pressure in the African. London: Churchill Livingstone; 1972. pp. 71–74. [Google Scholar]
- 3.Ahren B, Mutembei DS. Blood pressure distribution: A selected Tanzanian population. East Afr Med J. 1984;61(6):444–446. [PubMed] [Google Scholar]
- 4.Cooper R, Rotimi C. Hypertension in blacks. Am J Hypert. 1997;10(7,1):804–812. doi: 10.1016/s0895-7061(97)00211-2. [DOI] [PubMed] [Google Scholar]
- 5.Ikeme AC. Blood pressure and hypertension in Nigeria: the implication for hypertension control. Trop Card. 1987;139(Suppl II):77–81. [Google Scholar]
- 6.Osilesi O, David LT, Mbofung CF, Osiyemi FO, Atinmo T. Dietary mineral effects on the occurrence and control of hypertension - review paper. Nigeria J of Nutr Sci. 1987;8(2):83–96. [Google Scholar]
- 7.Abengowe CU. Serum uric acid values,hypertension and alcohol consumption in men. Trop Card. 1987;13(51):109–111. [Google Scholar]
- 8.Onwubere BJC, Ike SO. Prevalence of hypertention and its complications among medical admissions at the University of Nigeria Teaching Hospital, Enugu. Nigeria J Int Med. 2000;3(1):17–20. [PubMed] [Google Scholar]
- 9.Akinkugbe OO, editor. Non Communicable Diseases In Nigeria, Final Report of a National Survey. Lagos: Fed. Min. of Health and Social Services; 1997. Hypertension; pp. 12–41. [Google Scholar]
- 10.Kadiri S, Walker O, Salako BL, Akinkugbe O. Blood pressure, hypertension and correlates in urbanised workers in Ibadan, Nigeria-a revisit. Journ Hum Hypert. 1999;13:23–27. doi: 10.1038/sj.jhh.1000722. [DOI] [PubMed] [Google Scholar]
- 11.Iriarte MM, Perez OJ, Sagastoigitia JD, Molinero E, Murga N. Congestive heart failure due to hypertensive ventricular diastolic dysfunction. Am J Cardiol. 1995;76(13):43D–47D. doi: 10.1016/s0002-9149(99)80491-3. [DOI] [PubMed] [Google Scholar]
- 12.Fouad FM. Left ventricular diastolic function in hypertensive patients. Cir. 1987;75(Suppl 1):148–155. [PubMed] [Google Scholar]
- 13.Gardin JM, Drayer JI, Rohan MK. Doppler evaluation of left ventricular filling in mild and severe hypertension. J Am Coll Card. 1986;7:185–192. [Google Scholar]
- 14.Labovitz AJ, Pearson AC. Evaluation of left ventricular diastolic function: clinical relevance and recent Doppler echocardiographic insights. Am Heart J. 1987;114(4):836–851. doi: 10.1016/0002-8703(87)90795-2. [DOI] [PubMed] [Google Scholar]
- 15.Appleton CP, Hatle LK, Popp RL. Relation of transmitral flow velocity patterns to left ventricular diastolic dysfunction: new insights from a combined haemodynamic and Doppler echocardiographic study. J Am Coll Cardiol. 1988;12:426–440. doi: 10.1016/0735-1097(88)90416-0. [DOI] [PubMed] [Google Scholar]
- 16.Thirsk G. In: Equipment. In cardiac ultrasound. Wilde P, editor. London: Churchill Livingstone; p. 34. [Google Scholar]
- 17.Angiomachalelis N, Hourzamanis AI, Sideri S, Seralsi E, Vamualis C. Improvement of left ventricular diastolic dysfunction in hypertensive patients. 1 month after ACE Inhibition therapy. Heart Vessels. 1996;11(6):303–309. doi: 10.1007/BF01747189. [DOI] [PubMed] [Google Scholar]
- 18.De Mora MM, Aranda P, Aranda FG, Barakat S, Zafra SJ, Rubio AA, et al. Diastolic dysfunction, left ventricular hypertrophy, and microalbuminuria in mild to moderate essentiall arterial hypertension. Rev Esp Cardiol. 1997;(4):233–238. [PubMed] [Google Scholar]
- 19.Verdecchia P, Schillaci G, Guerrieri M, Boldrini F, Gaiteschi C, Benemio G, et al. Prevalence and determinants of left ventricular diastolic filling abnormalities in an unselected hypertensive population. Eur Heart J. 1990;11:679–691. doi: 10.1093/oxfordjournals.eurheartj.a059783. [DOI] [PubMed] [Google Scholar]
- 20.Mayet J, Shahi M, Poulter NR, Sever PS, Foale RA, Thomas AM. Left ventricular diastolic function in hypertension: a 4 year follow-up study. Int J Cardiol. 1995;50:181–188. doi: 10.1016/0167-5273(95)02367-6. [DOI] [PubMed] [Google Scholar]
- 21.Joint National Committee on detection, evaluation and treatment high blood pressure, author. The third report of the joint national committee on detection, evaluation and treatment of high blood pressure (JNC III) Arch Intern Med. 1984;144:1045–1057. [PubMed] [Google Scholar]
- 22.The guideline sub-committee of the who-ish mild hypertension liaison committee, author. 1993 guidelines for the management of mild hypertension. Memorandum from a world health organization - international society of hypertension meeting. J of Hypert. 1993;11:905–918. doi: 10.1097/00004872-199309000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Kigue S. The Proceedings of the fifth congress of the PanAfrican Society of Cardiology. Yaounde: 1993. Echocardiographic aspects of hypertensive heart disease in a group of hypertensives in Yaounde; p. 13. [Google Scholar]
- 24.Balogun MO, Urhogide GE, Ukoh VA, Adebayo RA. A preliminary audit of Two-dimensional and Doppler echocardiographic service in a Nigerian tertiary private hospital. Nig Journ of Med. 1999;8(40):139–141. [Google Scholar]
- 25.Philips RA, Goldman ME, Ardeljan M, Arora R, Eison HB, Yu BY, et al. Determinants of abnormal left ventricular filling in early hypertension. J Am Coll Cardiol. 1989:979–985. doi: 10.1016/0735-1097(89)90476-2. [DOI] [PubMed] [Google Scholar]
- 26.Gardin JM, Drayer JI, Weber M. Doppler echocardiographic assessment of left ventricular systolic and diastolic function in mild hypertension. Hypert. 1987;9(Suppl II):1990–1196. doi: 10.1161/01.hyp.9.2_pt_2.ii90. [DOI] [PubMed] [Google Scholar]
- 27.Medical research council working party, author. MRC trial of treatment of hypertension in older adults: principal results. Br Med J. 1992;304:405–412. doi: 10.1136/bmj.304.6824.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nicolino A, Ferrara N, Longobardi G, Acanfora D, Rengo C, Rengo F. Left ventricular diastolic filling in elderly hypertensive patients. J Am Geriatr Soc. 1993;41:217–222. [PubMed] [Google Scholar]
- 29.Rakowski H, Appleton C, Chan KL, Dumesnil JG, Honos G, Jue J, et al. For Canadian consensus recommendations for the measurement and reporting of diastolic dysfunction by echocardiography. J Am Soc Echocardiog. 1996;9:736–760. doi: 10.1016/s0894-7317(96)90076-0. [DOI] [PubMed] [Google Scholar]