Abstract
Study Design.
Reposition sense of lumbar curvature was assessed as a function of trunk flexion, trunk asymmetry, and target lumbar curvature using a repeated-measures design and an active-active proprioception paradigm.
Objective.
The objectives of the research were to measure the ability of the subjects to sense and control the lumbar curvature in different lifting postures and to see if error in the lumbar curvature would increase in high-risk postures.
Summary of Background Data.
The risk of low back disorders (LBDs) is related to trunk posture, with greater risk reported in flexed and asymmetric trunk positions. Spinal posture, including trunk position and lumbar lordosis, influences spinal stability. Hence, the ability to accurately sense and control spinal curvature may be an important factor in the control of LBD risk.
Methods.
Eleven subjects were trained to assume specified lumbar curvatures using visual feedback. The ability of the subjects to reproduce this curvature without feedback was then assessed. This procedure was repeated for different trunk postures, including flexion and asymmetry, and with different target lumbar curvatures.
Results.
These measurements demonstrated reposition error was increased in flexed trunk positions but was unchanged with trunk asymmetry. This increase in reposition error with flexion was diminished when the target posture and lumbar curvature were highly flexed and kyphotic.
Conclusions.
This research suggests that it may be difficult to control spinal curvature in flexed positions, leading to an increased risk of injury. For jobs in which flexed working postures are unavoidable, therefore, it is important to minimize potentially unstable events such as slipping or shifting loads to avoid injury.
Keywords: proprioception, lumbar, posture, lordosis
Asymmetric and flexed postures during manual materials handling are associated with increased risk of low back pain (LBP).12,15 The reason these postures are high risk, however, is not understood completely. It is known that compressive loads on the lumbar spine can be high in these positions. However, Punnett et al15 showed that many injuries occur at compressive loads that may be considered safe by the National Institute of Occupational Safety and Health (NIOSH) guidelines. This has led several researchers to consider stability as a potential factor in the risk of low back injury.5,6 The ability to accurately sense and control spinal curvature is particularly important in the feedback control of spinal stability. Therefore, spinal posture sense may be an important factor contributing to the risk of low back disorders (LBDs) during lifting activities.
Poor reposition sense has been shown to be related to risk of musculoskeletal injury in several joints, including the ankle and knee.4,9,10 Low back disorders have also been associated with changes in trunk reposition sense.7,11,19 Spinal reposition sense is influenced by many factors such as motion, trunk position, and loading.1,18 It remains unclear how position sense may be altered in flexion and twisting tasks traditionally associated with LBD risk.
Industrial lifting task design often constrains trunk position as a result of lifting origin, destination, and subject anthropometry. However, for a given trunk position, a range of lumbar curvatures can be maintained through the coordination of the pelvis (sacral spine) and lumbar segments (Figure 1). Lumbar curvature, e.g., kyphotic curvatures (stoop lifting) versus lordotic curvatures (squat lifting), influences compression and stability and is believed to influence LBD risk.2,3,20 The coordination of lumbar curvature with trunk flexion is often targeted for training by physical therapists treating LBDs.16 To control spinal posture, it is first necessary to be able to sense spinal curvature. Hence, spinal position sense may play a role in the biomechanics, injury, and rehabilitation of LBP.
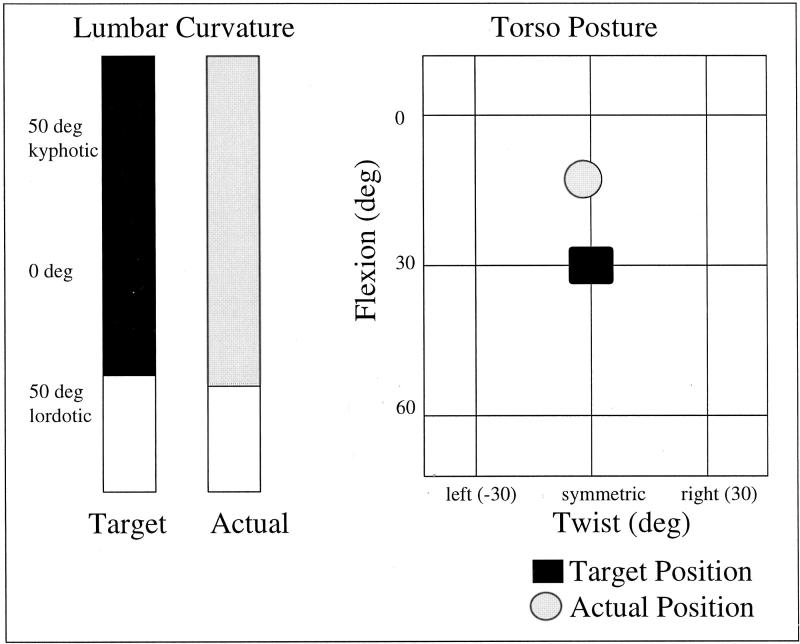
Figure 1.
Torso angle (twist, lateral bend, and flexion) is the tilt of the torso from horizontal as defined by the position of the three markers (A). Lumbar curvature is the difference in angle in twist, lateral bending, and flexion of the marker at T10 relative to the marker at S1 (B).
Although studies have investigated the reposition sense of trunk angle, there has been no direct research on the reposition sense of the lumbar spine. A few studies have examined the variability in lumbar curvature with the reposition of trunk angle. This research is useful but limited in describing control of the lumbar curvature, because although lumbar curvature is measured, subjects were not attempting to control the lumbar curvature but rather were controlling solely the trunk flexion. Gill and Callaghan7 concluded that the variability of self-selected lumbar curvature was greater in LBP subjects than in healthy normal persons during standing and kneeling. Swinkels and Dolan18 observed that lumbar curvature was more variable in flexed postures but was not influenced by preparatory motion. None of these studies have examined reproduction of lumbar curvature when lumbar curvature is the target. Only by having lumbar curvature as the target can self-selection or preference be removed from the measurement of this lumbar position sense. For example, if one is asked to stand upright, this posture may be achieved by a slouched back (i.e., a less lordotic lumbar spine) or by standing at attention (i.e.,a more lordotic lumbar spine). If the target is purely torso position, a variety of lumbar curvatures are possible, and a subject may choose among them based on personal preference. This personal preference would factor into the variability of lumbar curvature and may change with many external factors. However, if a subject is instructed to “stand up straight” with visual reinforcement (target curvature displayed on a computer screen) of lumbar curvature, the subject is no longer self-selecting lumbar curvature but is instead focusing on reposition of a lumbar curvature. This gives a more direct measure of the reposition sense of the lumbar spine, as preference and self-selection are removed from the measurement. None of the research on reposition sense of the trunk so far has examined this type of reposition sense assessment.
The goal of this study was to quantify the reposition sense of lumbar curvature as a component in the feedback control of spinal mechanics. The authors hypothesized that the reposition sense of the lumbar curvature will be less accurate (increased error) in high-risk trunk positions, such as flexion and asymmetric bending. This error may be a function of the target curvature.
Methods
This study included seven male and four female subjects (aged 24-34 [27 ± 4] years), with no significant history of LBP (defined here as a history of chronic LBP lasting > 1 month or incidence of LBP during the past year based on self-report). This study was approved by the Human Investigations Committee of the University of Virginia. The experiment consisted of 1) an assessment of the normal (self-selected) lumbar curvature at each of three trunk flexion angles (0°,30°, and 60°) and at three twist angles (30° right, 0° and 30° left) and 2) reposition tests at these postures. All combinations of these flexion and torso twist angles were assessed, with the exception of 60° of flexion and 30° of twist. This combination was found to be difficult for some subjects to achieve.
Reposition tests were achieved using an active-active paradigm. These tests consisted of groups of four training and two assessment runs for each postural condition. At each condition, subjects were asked to twist and flex to the prescribed trunk posture using real-time visual feedback from a computer monitor and to assume a prescribed lumbar curvature. The independent measures of trunk flexion, lumbar lordosis, and trunk twist were simultaneously displayed on a computer monitor for the subject to observe. Trunk posture was represented by a graph of twist on the x-axis and flexion on the y-axis (Figure 2). Lumbar curvature was represented by bar plots (Figure 2). Once the subject stated they had reached what they believed to be the correct position, data were collected for 5 seconds. During training exertions, both lumbar curvature and trunk posture were shown on the monitor for feedback. During assessment exertions, subjects were asked to recreate their previous lumbar curvature and trunk posture, while visual feedback illustrating lumbar curvature was removed, leaving only the visual display of trunk posture. An additional training exertion, with feedback display of both lumbar curvature and trunk posture, was performed between the two assessment exertions. The order of the runs during each position sense test was as follows:
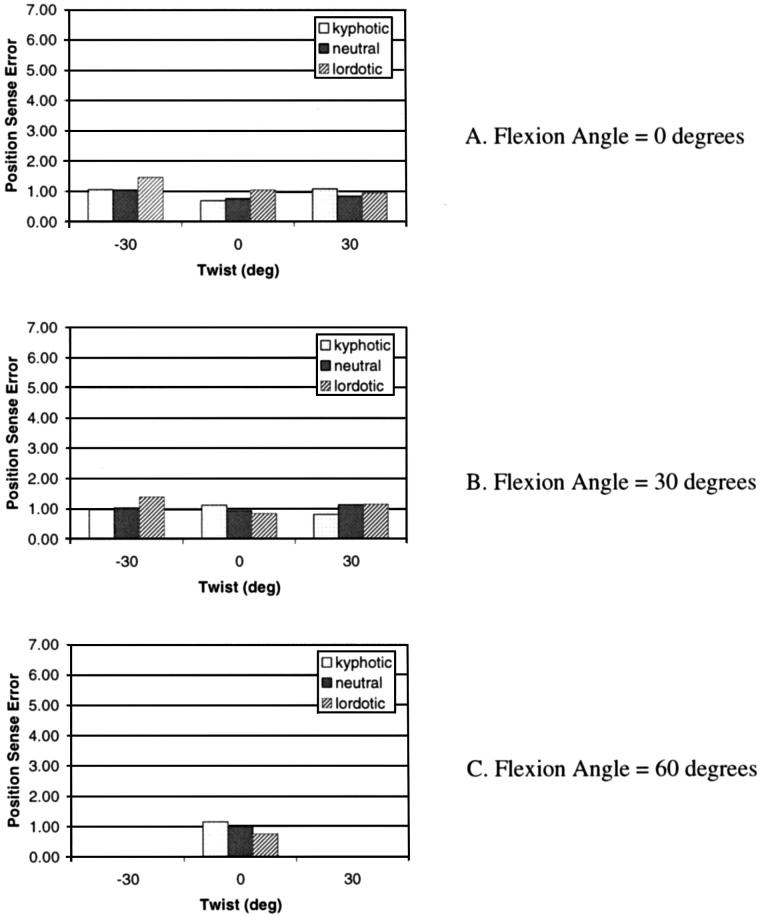
Figure 2.
Visual feedback was accomplished by displaying trunk posture (graph on right) and lumbar curvature (bars on left) in a display similar to that illustrated here. Trunk posture was represented on an x-y graph, with the x-axis as twist and the y-axis as flexion. Subjects matched a circle (representing their position) to a square (representing the target). For lumbar curvature, subjects matched the right bar plot (representing their lumbar curvature) with the left bar plot (representing the target). The lumbar curvature display was turned off for reposition sense testing.
Training (feedback = trunk position + lumbar curvature)
Training (feedback = trunk position + lumbar curvature)
Training (feedback = trunk position + lumbar curvature)
Assessment (feedback = trunk position only)
Training (feedback = trunk position + lumbar curvature)
Assessment (feedback = trunk position only)
Between each of these runs, subjects were asked to return to upright standing and to flex approximately 30° to prevent them from holding the curvature. The period between each run was approximately 10 seconds. When the next run commenced, subjects were given as much time as they needed to find the target again. Once subjects stated they had obtained the torso position and lumbar curvature, kinematic data were collected for 5 seconds.
Electromagnetic sensors (Ascension Technologies, Burlington, VT) were used to monitor torso flexion, lateral bending, and twist and to assess lumbar curvature based on surface curvature. These sensors have a reported resolution of 0.1° and 0.5 mm and a static accuracy of 0.5° and 1.8 mm. Sensors were placed over the spinous processes of the T10 thoracic vertebra and the S1 sacral vertebra. These locations were chosen to be consistent with previous work examining lumbar motion.8 A third sensor was placed over the manubrium. These sensors were attached to the skin using double-sided tape. These sensors can assess both position and orientation (twist, lateral, flexion). Torso orientation was calculated by examining the plane created by the three sensors (Figure 1A). Flexion, lateral bending, and twist were defined by a series of Euler angles with the rotation sequence of twist, lateral bending, and flexion (the matrix product for this sequence [R] is Rflex Rlat Rtwist). This sequence was used to have the two angles, twist and flexion, describe a realistic asymmetric lifting posture. Lumbar curvature was determined from the difference in flexion angle of the thoracic and sacral sensors (Figure 1B).
Normal (self-selected) curvature and the variability in normal curvature at each flexion and twist angle were assessed at the beginning of each experiment. Subjects were asked to assume the prescribed torso twist and flexion posture without instruction regarding lumbar curvature. Once subjects were comfortable in the position, lumbar curvature was recorded for 5 seconds. The order of the trunk postures was random, with subjects returning to upright between each condition. Each condition was repeated three times. The standard deviation in normal curvature recorded from these calibration trials was analyzed to compare with the literature. Normal curvatures for each subject, measured at the beginning of the experiment, were used to assign the target lumbar curvature in position sense conditions. Three target lumbar curvatures were used. These included 1) the normal curvature, 2) 5° more kyphotic than the normal curvature, and 3) 5° more lordotic than the normal curvature. These targets were selected because, in pilot studies, they were found to be the largest range that all subjects could accomplish comfortably.
For each training and reposition assessment, lumbar curvature error (the dependent variable) was calculated as the difference between the target lumbar curvature and the actual curvature in degrees. The absolute value of this error was used for analysis. Independent variables included 1) torso flexion angle (0°,30°,60°), 2) torso twist angle (-30°,0°,30°), and 3) target lumbar curvature (kyphotic, lordotic, or normal). Two separate and distinct analyses of variance were performed. First, data for all torso twist angles, all target lumbar curvature angles, and flexion angles of 0° and 30° were used to assess the effect of asymmetry and the interaction between asymmetry and flexion. Second, data for the symmetric cases (twist angle of 0°) were used to assess the changes in position sense as a function of torso flexion.
Results
Three dependent variables were assessed in this experiment: 1) error in lumbar curvature reposition during training runs with available visual feedback of lumbar posture, 2) error in lumbar curvature reposition during assessment trials without visual feedback describing lumbar posture, and 3) variability in lumbar curvature during initial self-selected lumbar curvature measurements. The first two represent the novel element of this experiment, and the third was used to compare the results of this experiment with those in previous literature.
Reposition accuracy was significantly reduced when visual feedback was removed. The absolute value of error in lumbar curvature during the training runs was small (1.01° ± 0.73°). This illustrates that the subjects were able to effectively use the visual feedback to control lumbar curvature. The absolute value of error increased significantly in the reposition assessment trials (when visual feedback was no longer available) to a mean error of 3.02° ± 2.85°. No significant difference in error was found within the three training runs or within the two position sense assessment runs. The absolute value of the error indicates the magnitude of error. However, it is also interesting to examine the possible bias toward under- or overestimation. In the reposition sense tests, no systematic under- or over estimation was observed, with the average actual error (not absolute) at 0.17° ± 0.68°.
In the training runs, when visual feedback of lumbar curvature was available, absolute error in lumbar curvature did not change with flexion or asymmetry (Figure 3). During the reposition assessments, when visual feedback of lumbar curvature was removed, absolute error in lumbar curvature increased significantly with flexion (1.49° ± 0.93° at 0° flexion, 4.16° ± 2.64° at 30° flexion, and 4.81° ± 2.64° at 60°flexion; P < 0.01; F = 6.66) during sagittally symmetric tasks (Figure 4, Table 1). Post hoc analyses revealed differences between the error during upright postures and both 30° and 60° of flexion. Although the lumbar reposition error increased from trunk flexion of 30° to 60°, the difference failed to achieve significance in post hoc analyses. Asymmetric positions did not demonstrate a significant effect in reposition error (P = 0.15; F = 2.06) (Table 1).
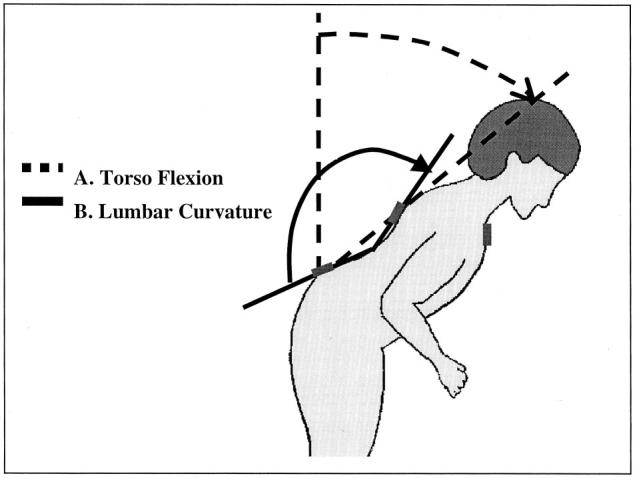
Figure 3.
Error (in degrees) in training run tests was calculated as the absolute difference between the target lumbar curvature (displayed for the subject) and the actual lumbar curvature. This error did not change significantly with flexion or asymmetric (twist). A, The error at a flexion angle of 0°; B, the error at a flexion angle of 30°; and C, the error at a flexion angle of 60°.
Figure 4.
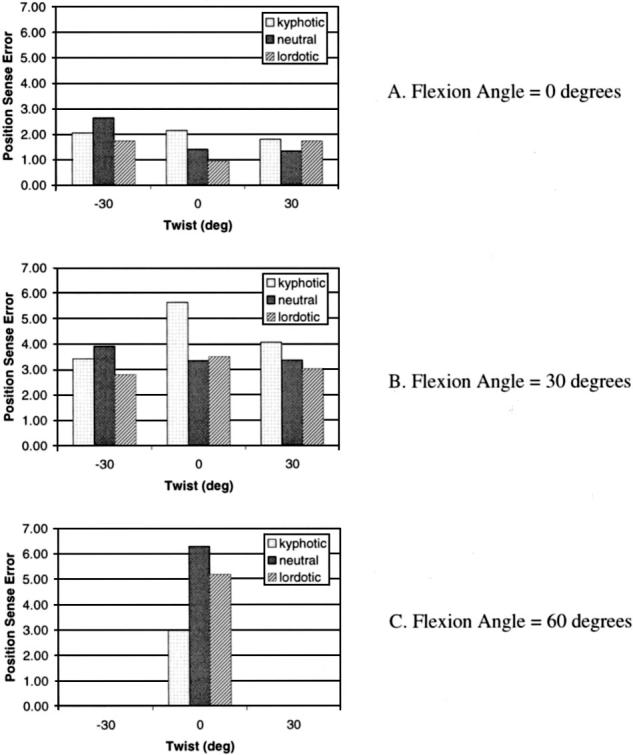
Error (in degrees) in position sense tests was calculated as the absolute difference between the target lumbar curvature (not displayed) and the actual lumbar curvature. A, The error at a flexion angle of 0°; B, the error at a flexion angle of 30°; and C, the error at a flexion angle of 60°. This error increased significantly at flexion angles of 30° (B) and 60° (C). However, the error did not change with asymmetric (twist). In the fully flexed kyphotic posture, error was reduced.
Table 1.
Two Analyses of Variance (ANOVAs) were Performed on the Position Assessment Tests, the Training Runs, and the Standard Deviation of Self-Selected Curvature. The First Analysis Examined the 0° and 30° Flexion Cases, Assessing Asymmetry (Twist), Flexion Angle, and Target Curvature Using a Huynh-Feldt Adjusted ANOVA. The Second Analysis Examined the Symmetric Cases to Assess All Three Flexion Angles.
| F | df | ε | P | ||
|---|---|---|---|---|---|
| ANOVA of Asymmetric Cases (Flexion Angle = 0° or 30°) | |||||
| Position sense | Twist angle | 0.40 | 1.82 | 0.91 | 0.656 |
| Flexion angle* | 20.35 | 1.00 | 1.00 | 0.001 | |
| Target posture | 2.06 | 2.00 | 1.00 | 0.154 | |
| Training | Twist angle | 2.01 | 1.55 | 0.84 | 0.173 |
| Flexion angle | 0.04 | 1.00 | 1.00 | 0.843 | |
| Target posture | 0.93 | 1.68 | 0.84 | 0.400 | |
| Variability | Twist angle | 0.68 | 1.98 | 0.99 | 0.516 |
| Flexion angle | 3.67 | 1.00 | 1.00 | 0.085 | |
| ANOVA of Symmetric Cases (twist 0°) | |||||
| Position sense | Flexion angle* | 6.66 | 1.77 | 0.88 | 0.009 |
| Target posture | 0.35 | 2.00 | 1.00 | 0.709 | |
| Training | Flexion angle | 0.88 | 1.92 | 0.96 | 0.427 |
| Target posture | 0.58 | 1.70 | 0.85 | 0.542 | |
| Variability | Flexion angle | 2.55 | 2.00 | 1.00 | 0.104 |
Indicates significance at P < 0.01.
Lordotic versus kyphotic postures influenced reposition error as a function of torso posture (flexion and twist). In upright and 30° flexed positions, errors in the normal, more lordotic, and more kyphotic target curvatures were not significantly different. However, within the 60° trunk flexion posture, the more kyphotic curvature was found to have a significantly lower error than the other two target postures.
Variability in lumbar curvature was also recorded during the neutral trials, wherein subjects achieved the prescribed trunk postures three separate times to establish normal curvature values. Increased variability of normal lumbar curvature with flexion failed to achieve statistical significance (3.14° ± 1.95° at 0° flexion, 5.98° ± 3.83° at 30°flexion, and 4.35° ± 4.23° at 60°flexion at 0° twist; P = 0.10; F = 2.55) for symmetric postures. The standard deviation of the normal lumbar curvature was not found to vary as a function of asymmetry.
Discussion
Position sense is intrinsic to the coordination of the torso musculature and the stability of the spine. In this study, the ability to reproduce lumbar curvature accurately has been shown to decrease in flexed positions. It was not, however, found to increase or decrease significantly with task asymmetry. It has long been shown that manual materials handling tasks involving flexed positions and asymmetric tasks pose a greater risk of low back pain. This research suggests that in flexion tasks, poor control of the lumbar curvature may be a component of this increased risk. However, poor control, evidenced by decreased position sense, does not explain the increased risk in asymmetric tasks.
Position sense can be thought of as the first part of a feedback mechanism that provides motor control and stabilization to the lumbar spine. The motor control of a sudden perturbation to the lumbar spine can be modeled with a feedback loop. The feedback is subject to a detection threshold, a time delay, and a response gain. Increased reposition error can be represented as an increased detection threshold. This would result in a decreased stability of the system.
Position sense in this experiment was measured as the absolute difference between the target and actual lumbar curvature. In addition, the actual difference (target curvature minus actual curvature) was also assessed. The absolute difference measures how accurate the system is overall, whereas the actual difference gets at whether there is a bias (underestimation vs. overestimation). In this experiment, there was a trend toward the actual error being an underestimation of the target lordosis (i.e., slightly more kyphotic) with increased flexion, but this trend was not significant. Neither was the average actual error significantly different than zero. This suggest that overall there was no bias toward underestimation or overestimation.
Both lumbar curvature and the torso posture were determined using the Euler angle sequence of twistlateral bending-flexion. This sequence is one in which a subject could achieve the combination of a twist and flexion by first twisting and then flexing in the twisted direction. This would be represented differently if the angles were in another sequence. The sequence chosen here was used because it represents the flexed, asymmetric lifting task in terms of only two angles, twist and flexion. Different rotation sequences may yield different results in the asymmetric torso postures. In addition, the lumbar curvature was defined using markers at the T10 and S1 spinal levels. This was done to be consistent with previous studies.8 However, it would also be possible to use alternate levels, such as T12 and S1. Some preliminary testing of the T12 position by the authors has shown that markers T10 and T12 rotate in a similar fashion. Although the value of the absolute error may be slightly different with alternate marker placement, the pattern of the results (increased error with flexion) would most likely remain the same.
The primary result of this study was an increase in reposition error with flexion. The flexed tasks differ from the upright tasks and the asymmetric upright tasks in the loading of the torso musculature and the orientation of the torso. This experiment did not seek to differentiate these two possible factors in reposition error. However, either or both may play a role in the loss of position sense. In sagittally flexed postures, lumbosacral moment created by the weight of the upper body increases relative to upright standing. Because the moment and torso flexion increase together, it is impossible in this experiment to tell whether the increases in reposition error with flexion are caused by altered geometry or by increased moment loads and muscle activity. Future research is needed to differentiate the potential effects of loading from the effects of geometric (torso flexion) changes.
The lack of a change in reposition sense with asymmetry was a surprising finding. There are two potential factors that may go into this. First, it was observed that the neutral curvature did not change much with asymmetry, whereas it changed dramatically with flexion. It is possible that reposition sense is a function of the spine shape. If this were the case, one would expect reposition sense to change with flexion but not asymmetry. However, if this were the case, one may also expect to see a difference in reposition sense with target curvature. Secondarily, in asymmetric tasks, the lumbosacral moment would not be expected to change a great deal relative to equally flexed symmetric tasks. In contrast, lumbosacral moment would increase dramatically with flexion. If reposition sense were a function of loading, then it is possible it would not change much with asymmetry but would change significantly with flexion.
A few previous studies have examined variability in the lumbar curvature with flexion. This variability is a measure of the self-selected lumbar curvature and is at best an indirect measure of the lumbar reposition sense. In this experiment, both the lumbar reposition sense and the variability in self-selected lumbar curvature were measured. Although reposition error increased significantly in this experiment, the increase in lumbar curvature variability was not significantly influenced by trunk posture. This finding suggests that lumbar curvature variability is not as strong a measure of position sense. The ability to more directly measure the localized control of the lumbar spine by removing the element of self-selection greatly enhances our ability to measure and understand lumbar coordination.
This research also examined the association between target position (more kyphotic or lordotic) and error. In highly flexed positions (60° of torso flexion), more kyphotic target postures were found to have significantly less reposition error than were more lordotic target postures. In these highly flexed positions, the ligamentous structures of the low back begin to provide support to the spine. Solomonow et al17 demonstrated that stretch of these ligamentous structures creates a reflex response providing proprioceptive feedback mechanism. This would suggest that a more kyphotic posture may be easier to maintain in highly flexed positions because the ligamentous structures provide mechanical support and assist in maintaining spinal stability. However, prolonged flexion may disturb this. McGill and Kippers14 demonstrated that these structures can undergo a viscoelastic stretch in prolonged flexed positions, and Solomonow et al17 demonstrated that prolonged stretch of spinal ligaments can result in decreased reflexive activity. Further research is warranted to investigate the effect of viscoelastic stretch on reposition sense of the lumbar curvature. In addition, the total stability of this posture may be subject to changes in other elements of the feedback response control loop that should also be investigated, including reduced muscle stiffness. Finally, although the position sense is improved, the strain on the passive tissues may put the individual at risk of injuring those tissues.
Recent trends in physical therapy for LBP have been to improve control of posture through “spinal stabilization exercises.”13,16 The current results suggest that this control of curvature is a function of torso flexion and target spinal shape and may play a role in spinal stabilization. Future research should examine how such exercises may improve this position sense.
In conclusion, if increased reposition error leads to an increased risk of stability-related injuries, results suggest that manual materials handling in flexed postures would be the most risky, in agreement with epidemiologic evidence. Ideally, work tasks would be designed to minimize flexion in order to minimize the risk of low back injuries. However, in some jobs, flexion tasks are unavoidable. For workers engaged in flexion tasks, this research suggests that sudden or unexpected loading events may be particularly risky. It may be more important, therefore, to assure that workers are particularly secure in footing and are not handling unsteady objects when they are forced to work in flexed postures. Additional research is required to understand how the loading in such flexion tasks may influence position sense and ultimately the stability of the low back and the risk of injury.
Key Points.
•Lumbar reposition sense, measured with lumbar curvature as the feedback, is a novel measure of the ability of an individual to sense and control low back posture.
•Reposition error increases with flexion but remains unchanged with asymmetry.
•Increased error with flexion may result in decreased stability and may help to explain the increased incidence of LBDs with flexed tasks.
Acknowledgment
This research was supported in part by a grant R01 AR46111-02 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) of the National Institutes of Health and by fellowship support from DePuy-Acromed.
Footnotes
This work was supported in part by DePuy-Acromed and by grant R01 AR46111-02 from National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) of the National Institutes of Health.
Conflict of interest: Corporate/industry and federal funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this report.
References
- 1.Ashton-Miller JA, McGlashen KM, Schultz AB. Trunk positioning accuracy in children 7-18 years old. J Orthop Res. 1992;10:217–25. doi: 10.1002/jor.1100100209. [DOI] [PubMed] [Google Scholar]
- 2.Burgess-Limerick R, Abernethy B. Toward a quantitative definition of manual lifting postures. Hum Factors. 1997;39:41–8. doi: 10.1518/001872097778940632. [DOI] [PubMed] [Google Scholar]
- 3.Burgess-Limerick R, Abernethy B, Neal RJ, et al. Self-selected manual lifting technique: functional consequences of the interjoint coordination. Hum Factors. 1995;37:395–411. doi: 10.1518/001872095779064537. [DOI] [PubMed] [Google Scholar]
- 4.Carter ND, Jenkinson TR, Wilson D, et al. Joint position sense and rehabilitation in the anterior cruciate ligament deficient knee. Br J Sports Med. 1997;31:209–12. doi: 10.1136/bjsm.31.3.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cholewicki J, Panjabi MM, Khachatryan A. Stabilizing function of trunk flexorextensor muscles around a neutral spine posture. Spine. 1997;22:2207–12. doi: 10.1097/00007632-199710010-00003. [DOI] [PubMed] [Google Scholar]
- 6.Crisco JJ, Panjabi MM. Euler stability of the human ligamentous lumbar spine: part 1. Theory. Clinical Biomechanics. 1992;7:19–26. doi: 10.1016/0268-0033(92)90003-M. [DOI] [PubMed] [Google Scholar]
- 7.Gill KP, Callaghan MJ. The measurement of lumbar proprioception in individuals with and without low back pain. Spine. 1998;23:371–7. doi: 10.1097/00007632-199802010-00017. [DOI] [PubMed] [Google Scholar]
- 8.Granata KP, Sanford AS. Lumbar-pelvic coordination is influence by lifting task parameters. Spine. 2000;25:1413–8. doi: 10.1097/00007632-200006010-00014. [DOI] [PubMed] [Google Scholar]
- 9.Konradsen L, Olesen S, Hansen HM. Ankle sensorimotor control and eversion strength after acute ankle inversion injuries. Am J Sports Med. 1998;26:72–7. doi: 10.1177/03635465980260013001. [DOI] [PubMed] [Google Scholar]
- 10.Konradsen L, Ravn JB, Sorensen AI. Proprioception at the ankle: the effect of anaesthetic blockade of ligament receptors. J Bone Joint Surg Br. 1993;75:433–6. doi: 10.1302/0301-620X.75B3.8496215. [DOI] [PubMed] [Google Scholar]
- 11.Lam SS, Jull G, Treleaven J. Lumbar spine kinesthesia in subjects with low back pain. J Orthop Sports Phys Ther. 1999;29:294–9. doi: 10.2519/jospt.1999.29.5.294. [DOI] [PubMed] [Google Scholar]
- 12.Marras WS, Lavender SA, Leurgans SE, et al. Biomechanical risk factors for occupationally related low back disorders. Ergonomics. 1995;38:377–410. doi: 10.1080/00140139508925111. [DOI] [PubMed] [Google Scholar]
- 13.McGill SM. Low back exercises: evidence for improving exercise regimens. Phys Ther. 1998;78:754–65. doi: 10.1093/ptj/78.7.754. [DOI] [PubMed] [Google Scholar]
- 14.McGill SM, Kippers V. Transfer of loads between lumbar tissues during the flexion-relaxation phenomenon. Spine. 1994;19:2190–6. doi: 10.1097/00007632-199410000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Punnett L, Fine LJ, Keyserling WM, et al. Back disorders and nonneutral trunk postures of automobile assembly workers. Scand J Work Environ Health. 1991;17:337–46. doi: 10.5271/sjweh.1700. [DOI] [PubMed] [Google Scholar]
- 16.Richardson C, Jull G, Hodges P, et al. Therapeutic Exercise for Spinal Segmental Stabilization in Low Back Pain. Churchill Livingstone; Philadelphia: 1999. [Google Scholar]
- 17.Solomonow M, Zhou BH, Baratta RV, et al. Biomechanics of increased exposure to lumbar injury caused by cyclic loading: part 1. Loss of reflexive muscular stabilization. Spine. 1999;24:2426–34. doi: 10.1097/00007632-199912010-00003. [DOI] [PubMed] [Google Scholar]
- 18.Swinkels A, Dolan P. Spinal position sense is independent of the magnitude of movement. Spine. 2000;25:98–104. doi: 10.1097/00007632-200001010-00017. [DOI] [PubMed] [Google Scholar]
- 19.Taimela S, Kankaanpaa M, Luoto S. The effect of lumbar fatigue on the ability to sense a change in lumbar position: a controlled study. Spine. 1999;24:1322–7. doi: 10.1097/00007632-199907010-00009. [DOI] [PubMed] [Google Scholar]
- 20.Trafimow JH, Schipplein OD, Novak GJ, et al. The effects of quadriceps fatigue on the technique of lifting. Spine. 1993;18:364–7. doi: 10.1097/00007632-199303000-00011. [DOI] [PubMed] [Google Scholar]