Abstract
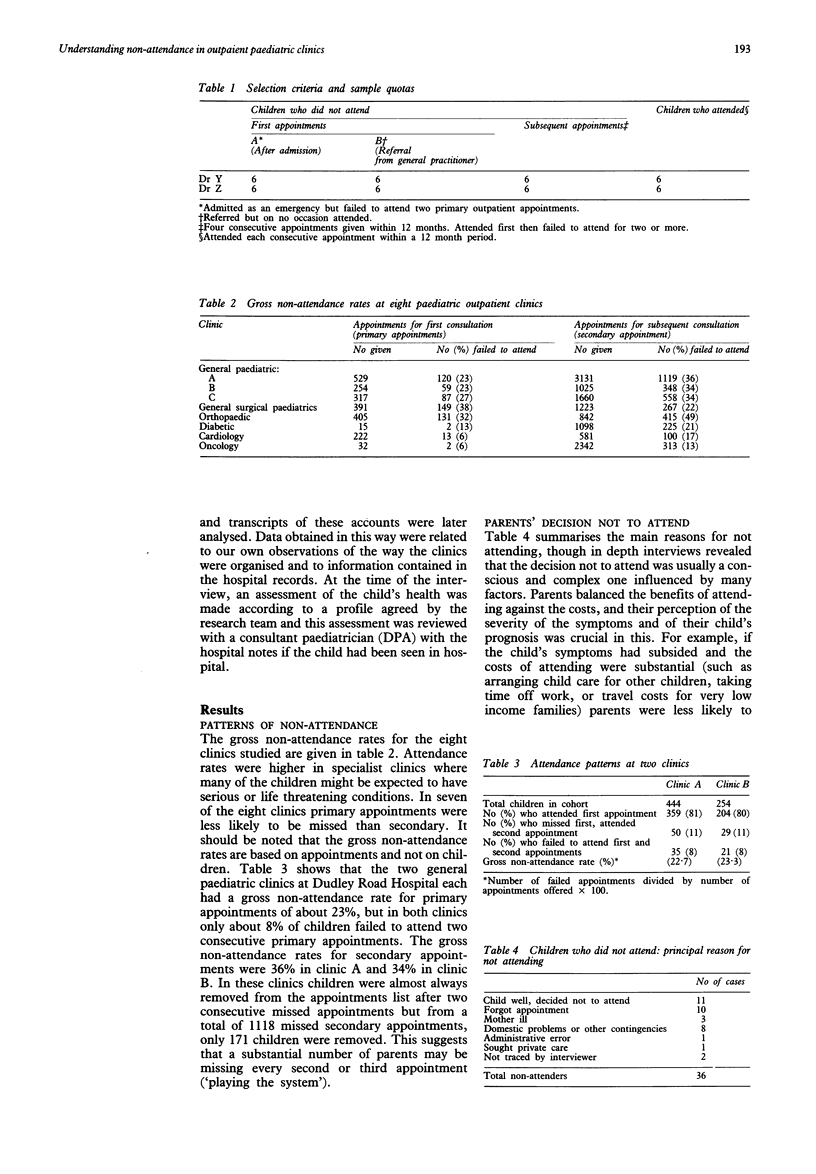
Outpatient clinic appointments are often not kept. There has been little study of the reasons for this, but failure to attend may affect future health. Our study was based on the children's outpatient department of a large inner city district general hospital. The parents of 34 children who had failed to keep appointments and of 12 who did attend were interviewed in depth and the appointment systems of the hospital and of a nearby regional referral centre for children were reviewed. At the district general hospital 23% of first appointments and 35% of subsequent appointments were not kept. We found that parents usually made a conscious decision about attending, balancing the perceived advantages and disadvantages of doing so. Their assessment of the severity of the child's illness was crucial in this. Twenty one of the 34 children who had not attended were assessed at the time of interview as still needing to attend. Of these, 16 subsequently kept an appointment and 11 underwent further investigation or treatment. We conclude that children who are not brought for outpatient appointments may be at risk of avoidable ill health and that ways of either ensuring attendance at outpatient clinics or providing alternative means of health supervision are needed.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Andeson F. P., Rowe D. S., Dean V. C., Arbisser A. An approach to the problem of noncompliance in a pediatric outpatient clinic. Am J Dis Child. 1971 Aug;122(2):142–143. [PubMed] [Google Scholar]
- Cockburn J., Gibberd R. W., Reid A. L., Sanson-Fisher R. W. Determinants of non-compliance with short term antibiotic regimens. Br Med J (Clin Res Ed) 1987 Oct 3;295(6602):814–818. doi: 10.1136/bmj.295.6602.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper N. A., Lynch M. A. Lost to follow up: a study of nonattendance at a general paediatric outpatient clinic. Arch Dis Child. 1979 Oct;54(10):765–769. doi: 10.1136/adc.54.10.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace J. F., Armstrong D. Reasons for referral to hospital: extent of agreement between the perceptions of patients, general practitioners and consultants. Fam Pract. 1986 Sep;3(3):143–147. doi: 10.1093/fampra/3.3.143. [DOI] [PubMed] [Google Scholar]
- Marinker M., Wilkin D., Metcalfe D. H. Referral to hospital: can we do better? BMJ. 1988 Aug 13;297(6646):461–464. doi: 10.1136/bmj.297.6646.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGlade K. J., Bradley T., Murphy G. J., Lundy G. P. Referrals to hospital by general practitioners: a study of compliance and communication. BMJ. 1988 Nov 12;297(6658):1246–1248. doi: 10.1136/bmj.297.6658.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon T., Clark C. M., Bailie G. R. Who provides patients with drug information? Br Med J (Clin Res Ed) 1987 Feb 7;294(6568):355–356. doi: 10.1136/bmj.294.6568.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pill R., French J., Harding K., Stott N. Invitation to attend a health check in a general practice setting: comparison of attenders and non-attenders. J R Coll Gen Pract. 1988 Feb;38(307):53–56. [PMC free article] [PubMed] [Google Scholar]


