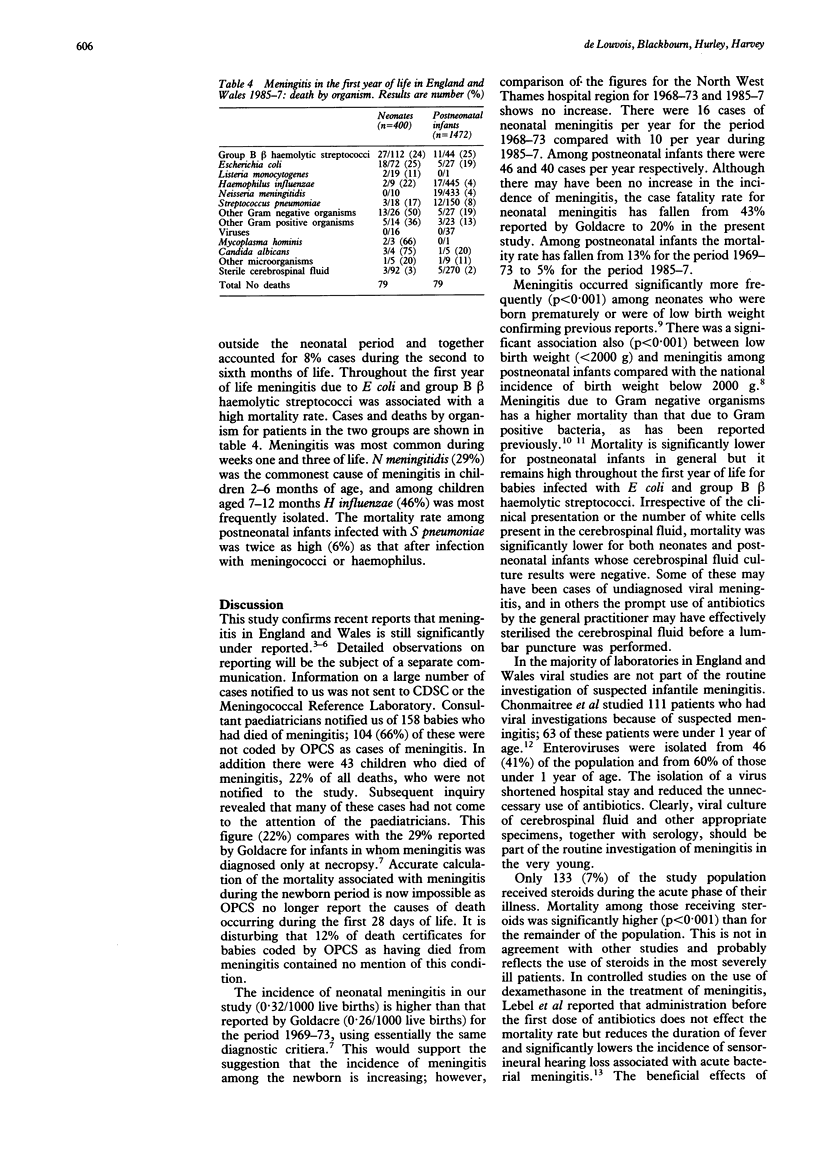
Abstract
A two year prospective study identified 1922 cases of meningitis in children under 1 year of age. A further 201 cases were identified from other sources. The annual incidence of meningitis during the first year of life was 1.6/1000; during the first 28 days of life it was 0.32/1000, and among postneonatal infants it was 1.22/1000. The male:female ratio was 1.4:1. The overall case fatality rate was 19.8% for neonates and 5.4% for postneonatal infants. Two thirds of deaths identified in the study, 50% of all deaths, were not attributed to meningitis by the Office of Population Censuses and Surveys. Group B beta haemolytic streptococci (28%), Escherichia coli (18%), and Listeria monocytogenes (5%) were most frequently isolated from neonates and Neisseria meningitidis (31%), Haemophilus influenzae (30%), and Streptococcus pneumoniae (10%) from postneonatal infants. At 2-6 months of age N meningitidis meningitis was most common, and at 7-12 months H influenzae predominated. Meningitis caused by group B beta haemolytic streptococci occurred up to 6 months of age and had a consistent mortality of 25%. Neonatal meningitis due to Gram negative enteric rods had a mortality of 32%. Low birth weight was a significant predisposing factor for both neonates and postneonatal infants. In both groups mortality was significantly higher among children admitted in coma. There was no seasonal variation in incidence in either group. Neonates were treated with either group. Neonates were treated with either chloramphenicol (50%) or gentamicin (48%) usually in combination with a penicillin; 40% received a third generation cephalosporin. Of the 1472 postneonatal infants treated 84% received chloramphenicol with a penicillin and 10% received a third generation cephalosporin. Relapse occurred in 49 patients and three died. Eighteen babies coned as a result of raised intracranial pressure, including four neonates, and four died. Mortality among the 133 (7%) children who received steroids was significantly higher than in the rest of the study group.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cartwright K. A., Stuart J. M., Noah N. D. An outbreak of meningococcal disease in Gloucestershire. Lancet. 1986 Sep 6;2(8506):558–561. doi: 10.1016/s0140-6736(86)90124-8. [DOI] [PubMed] [Google Scholar]
- Chonmaitree T., Menegus M. A., Powell K. R. The clinical relevance of 'CSF viral culture'. A two-year experience with aseptic meningitis in Rochester, NY. JAMA. 1982 Apr 2;247(13):1843–1847. [PubMed] [Google Scholar]
- Davies L. A. Assessing the value of different sources of information on meningococcal disease. Community Med. 1989 Aug;11(3):239–246. doi: 10.1093/oxfordjournals.pubmed.a042474. [DOI] [PubMed] [Google Scholar]
- Girgis N. I., Farid Z., Mikhail I. A., Farrag I., Sultan Y., Kilpatrick M. E. Dexamethasone treatment for bacterial meningitis in children and adults. Pediatr Infect Dis J. 1989 Dec;8(12):848–851. doi: 10.1097/00006454-198912000-00004. [DOI] [PubMed] [Google Scholar]
- Goldacre M. J. Acute bacterial meningitis in childhood. Incidence and mortality in a defined population. Lancet. 1976 Jan 3;1(7949):28–31. doi: 10.1016/s0140-6736(76)92921-4. [DOI] [PubMed] [Google Scholar]
- Lebel M. H., Freij B. J., Syrogiannopoulos G. A., Chrane D. F., Hoyt M. J., Stewart S. M., Kennard B. D., Olsen K. D., McCracken G. H., Jr Dexamethasone therapy for bacterial meningitis. Results of two double-blind, placebo-controlled trials. N Engl J Med. 1988 Oct 13;319(15):964–971. doi: 10.1056/NEJM198810133191502. [DOI] [PubMed] [Google Scholar]
- Mason-Brothers A., Ritvo E. R., Pingree C., Petersen P. B., Jenson W. R., McMahon W. M., Freeman B. J., Jorde L. B., Spencer M. J., Mo A. The UCLA-University of Utah epidemiologic survey of autism: prenatal, perinatal, and postnatal factors. Pediatrics. 1990 Oct;86(4):514–519. [PubMed] [Google Scholar]
- Mulder C. J., Zanen H. C. A study of 280 cases of neonatal meningitis in The Netherlands. J Infect. 1984 Sep;9(2):177–184. doi: 10.1016/s0163-4453(84)91351-3. [DOI] [PubMed] [Google Scholar]
- Mulhall A., de Louvois J., Hurley R. Efficacy of chloramphenicol in the treatment of neonatal and infantile meningitis: a study of 70 cases. Lancet. 1983 Feb 5;1(8319):284–287. doi: 10.1016/s0140-6736(83)91697-5. [DOI] [PubMed] [Google Scholar]
- Ritvo E. R., Jorde L. B., Mason-Brothers A., Freeman B. J., Pingree C., Jones M. B., McMahon W. M., Petersen P. B., Jenson W. R., Mo A. The UCLA-University of Utah epidemiologic survey of autism: recurrence risk estimates and genetic counseling. Am J Psychiatry. 1989 Aug;146(8):1032–1036. doi: 10.1176/ajp.146.8.1032. [DOI] [PubMed] [Google Scholar]
- Shohet I., Davidson S., Shahar E., Lison M., Barzilay Z., Rubinstein E. Bacterial meningitis. A follow-up study of 115 children. Isr J Med Sci. 1982 Jul;18(7):779–784. [PubMed] [Google Scholar]
- Smalley S. L., Asarnow R. F., Spence M. A. Autism and genetics. A decade of research. Arch Gen Psychiatry. 1988 Oct;45(10):953–961. doi: 10.1001/archpsyc.1988.01800340081013. [DOI] [PubMed] [Google Scholar]


