Abstract
Introduction
We conducted a post-hoc analysis on the effect of recombinant factor VIIa (rFVIIa) on coagulopathic patients from two randomized, placebo-controlled, double-blind trials of rFVIIa as an adjunctive therapy for bleeding in patients with severe trauma.
Methods
Blunt and penetrating trauma patients were randomly assigned to rFVIIa (200 + 100 + 100 μg/kg) at 0, 1, and 3 hours after transfusion of 8 units of red blood cells (RBCs) or to placebo. Subjects were monitored for 48 hours post-dosing and followed for 30 days. Coagulopathy was retrospectively defined as transfusion of fresh frozen plasma (FFP) (>1 unit of FFP per 4 units of RBCs), FFP in addition to whole blood, and transfusion of platelets and/or cryoprecipitate.
Results
Sixty rFVIIa-treated and 76 placebo subjects were retrospectively identified as being coagulopathic. No significant differences were noted in baseline characteristics. The rFVIIa-treated coagulopathic subgroup consumed significantly less blood product: RBC transfusion decreased by 2.6 units for the whole study population (P = 0.02) and by 3.5 units among patients surviving more than 48 hours (P < 0.001). Transfusion of FFP (1,400 versus 660 ml, P < 0.01), platelet (300 versus 100 ml, P = 0.01), and massive transfusions (29% versus 6%, P < 0.01) also dropped significantly. rFVIIa reduced multi-organ failure and/or acute respiratory distress syndrome in the coagulopathic patients (3% versus 20%, P = 0.004), whereas thromboembolic events were equally present in both groups (3% versus 4%, P = 1.00).
Conclusion
Coagulopathic trauma patients appear to derive particular benefit from early adjunctive rFVIIa therapy.
Introduction
Trauma is the leading cause of mortality up to the fifth decade of life [1,2] and uncontrolled hemorrhage is responsible for approximately 40% of these fatalities [2-5]. Diffuse coagulopathy is one of the most challenging situations faced by physicians treating these patients and is associated with high morbidity and mortality. Coagulopathy is common, affecting as many as 25% to 36% of trauma victims, and may develop early after injury [6,7]. It results from factors such as dilution and consumption of coagulation factors and platelets, fibrinolysis, acidosis, and hypothermia. Although coagulopathy correlates with the severity of trauma, it is also an independent risk factor of mortality [7]. There is little agreement in the contemporary literature as to the precise definition of coagulopathy in trauma (Table 1) [6-11]. Because objective measurement of coagulopathy is often unattainable in the clinical setting, current guidelines recommend empirical replacement therapy for the coagulopathic patient with diffuse microvascular bleeding [8,12]. Current management involves replacing coagulation factors (fresh frozen plasma [FFP], platelets, and cryoprecipitate) and correcting acidosis and hypothermia, steps that often are insufficient to stop the bleeding and prevent death.
Table 1.
Definitions of coagulopathy in the recent trauma literature
| Laboratory parameters | Source |
| PT ≥1.5 N (0) 1.5–2 N (1) >2 N (2) | Mayo et al., 2004 [11] |
| PTT ≥1.5 N (0) 1.5–2 N (1) >2 N (2) | |
| Plt >100 (0) 50–100 (1) ≥50 (2) | |
| Fib >100 (0) 50–100 (1) ≥50 (2) | |
| Total: 0 mild, 1–3 moderate, 4–8 severe | |
| INR >1.4 or Plt <100,000 or both | Dutton et al., 2004 [9] |
| PT >18 seconds or PTT >60 seconds or TT >15 seconds | Brohi et al., 2003 [6] |
| PT >14 seconds or PTT >34 seconds | MacLeod et al., 2003 [7] |
| PT >15 seconds or PTT >45 seconds or Fib <100 | Vaslef et al., 2002 [37] |
| PT or PTT twice normal | Cosgriff et al., 1997 [10] |
| PT or PTT >1.5–1.8 times control values | Stehling et al., 1996 [8] |
| Ongoing bleeding, oozing from cut surfaces, catheters, or mucous membranes | Lynn et al., 2002 [31] |
Fib, fibrinogen; INR, international normalized ratio; N, normal; Plt, platelet; PT, prothrombin time; PTT, partial thromboplastin time; TT, thrombin time.
Recombinant activated factor VII (rFVIIa) (NovoSeven®; Novo Nordisk A/S, Bagsværd, Denmark) is a hemostatic agent that acts at the site of injury to enhance thrombin generation, leading to a stable fibrin clot [13,14]. A growing number of case series and reports have described the safe and effective hemostatic properties of rFVIIa in trauma patients with uncontrolled hemorrhage refractory to conventional therapy [9,15]. These publications have described impressive results with the use of rFVIIa as a treatment option to control bleeding in high-risk, actively bleeding patients in various situations, including trauma [9,15,16], severe postpartum hemorrhage [17,18], and cardiac surgery [19-21]. Recently, our group published the first multi-center, international, randomized, placebo-controlled, double-blind study of rFVIIa in trauma and demonstrated that it is a safe and efficacious adjunctive therapy in controlling hemorrhage [22]. Considering that the majority of the patients in this study had evidence of being coagulopathic at the time of rFVIIa administration, we hypothesized that rFVIIa might have a particularly beneficial role in the treatment of diffuse coagulopathy that results from severe trauma.
To test this hypothesis, we carried out a post-hoc analysis of a subgroup of patients from the randomized prospective trial, who based on the clinical requirement for replacement therapy were identified as having coagulopathy.
Materials and methods
The study protocol was approved by the ethics committee of each participating institution (see Appendix), and the trial was conducted according to Good Clinical Practice standards and the Helsinki Declaration. Written informed consent was obtained from all patients or, where applicable, from a legally authorized representative. Due to the emergency conditions and the possible absence of relatives at enrolment in the trial, ethics committees authorized waived informed consent. However, whenever a patient was included without written informed consent, such consent was promptly solicited from a legally authorized representative and subsequently from the patient.
The methods of the study have been previously detailed [22]. Briefly, to be eligible for inclusion, patients were to have received 6 units of red blood cells (RBCs) within a four hour period and to be of known age of at least 16 years (or legally of age according to local law) and less than 65 years. Key exclusion criteria were cardiac arrest pre-hospital or in the emergency or operating rooms prior to trial drug administration; gunshot wound to the head; Glasgow Coma Scale of less than 8 unless in the presence of a normal computed tomography scan of the head; base deficit of more than 15 mEq/l or severe acidosis with pH of less than 7.00; transfusion of 8 or more units of RBCs prior to arrival to the trauma center; and injury sustained 12 or more hours before randomization.
This was a randomized, placebo-controlled, double-blind trial with two parallel treatment arms in two separate trauma populations (blunt and penetrating traumas). Upon receiving 6 units of RBCs within a four hour period, eligible patients within each trauma population were equally randomly assigned to receive either three intravenous injections of rFVIIa (200, 100, and 100 μg/kg) or three placebo injections. The first dose of trial product was to be administered immediately after transfusion of the eighth unit of RBCs, given that the patient (in the opinion of the attending physician) would require additional transfusions. The second and third doses followed one and three hours after the first dose, respectively. Trial product was administered in addition to standard treatment for injuries and bleeding at the participating hospitals, and no restrictions were imposed on procedures deemed necessary by the attending physician, including surgical interventions, resuscitation strategies, and use of blood products. To reduce the differences in standards of care between countries and institutions, each participating trauma center had to develop specific transfusion guidelines in line with the transfusion guidelines provided in the study protocol.
Subgroup selection
Patients included in the two arms of the trial (blunt and penetrating traumas) were pooled together. Because it was not possible to objectively determine a patient's coagulopathic status at study entry (due to the lack of a consensus laboratory definition for coagulopathy, time constraints, and limitations of laboratory testing in a trauma setting), a post-hoc state of coagulopathy was defined based on current transfusion guidelines [8]. For the purpose of the present analysis, coagulopathic patients were identified using the following definition: an ongoing bleeding that required the use of transfusion with FFP and RBC units at a ratio of 1 or more units of FFP for every 4 units of RBCs, and/or the use of FFP with whole blood, and/or transfusion of platelets, and/or the transfusion of cryoprecipitate. This definition was used because no consensus definition currently exists that adequately defines coagulopathy. Because traumatic brain injury (TBI) mandates a different fluid and transfusion management, carries a higher risk for coagulopathy, and has outcomes that are distinctive from other polytrauma patients, patients with TBI were also excluded from this analysis [23]. A flowchart of the present study is depicted in Figure 1.
Figure 1.
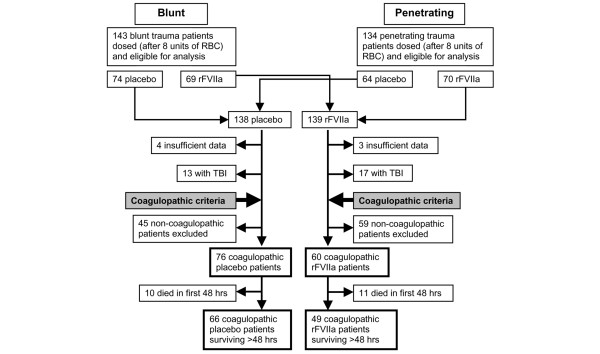
Trial profile. The figure shows the number of penetrating and blunt trauma patients eligible in the two groups (placebo and recombinant activated factor VII [rFVIIa]), the exclusion of patients because of traumatic brain injury (TBI) and insufficient data concerning the coagulopathic state, and the number of patients finally adjudicated to the placebo and rFVIIa analysis. RBC, red blood cells.
Endpoints
The primary endpoint was the number of RBC units (allogeneic RBCs, autologous RBCs, and whole blood) transfused during the 48-hour period after the first dose of trial product, as previously described [22]. Outcome of therapy was further assessed through requirement for other transfusion products, massive transfusion (defined as more than 20 units of RBCs inclusive of the 8 pre-dose units), time on ventilator, time in the intensive care unit (ICU), and serious adverse events, including the predefined critical complications of multiple organ failure (MOF), acute respiratory distress syndrome (ARDS), and death, all recorded until day 30. Because mortality is not a sensitive variable in a trauma population, we also studied a composite endpoint that comprised death, MOF, and ARDS, repeating the analysis performed in the original randomized controlled trial (RCT) [24,25]. To enable us to compare the durations of hospitalization and of ICU admission while taking into account mortality rates, we calculated the number of hospital-free days and ICU-free days within one month after trauma, with all deceased patients being given a score of 0 hospital- or ICU-free days, as previously described [26].
Separate analyses were performed in which patients who died within 48 hours were excluded, as previously described [22]. Patients who died within 48 hours were excluded because in a large proportion of these patients, care was futile and 48-hour transfusion requirements could not be objectively assessed for patients who were alive for only a few hours.
Statistical analysis
Data are expressed as mean ± standard deviation or as median and range. All statistical comparisons were two-tailed, and P less than 0.05 was considered significant. Comparison between the two groups was performed using the Wilcoxon-Mann-Whitney rank sum tests for continuous outcomes (transfusions, time on ventilator, and time in ICU), and Fisher's exact test was used for binary outcomes (massive transfusion, MOF, ARDS, and mortality). The differences between groups were estimated by the Hodges-Lehman shift with 95% confidence interval (CI) for continuous outcomes, and relative risk reductions (RRR) and numbers needed to treat (NNT) with 95% CIs were used for the binary outcomes. Patients who died within 48 hours were assigned highest rank (worst outcome) in the Mann-Whitney test and in the Hodges-Lehman estimation.
Results
Of the 277 randomly assigned patients eligible for analysis, 30 were excluded from evaluation because of TBI and seven others for insufficient data on their coagulopathic status. Thus, using the defined criteria for coagulopathy, the subgroup of coagulopathic patients comprised a total of 136 patients, 76 of whom had received placebo and 60 of whom had received rFVIIa (Figure 1). A comparative overview of baseline characteristics of the selected coagulopathic patient subgroup, according to the defined criteria, versus the non-coagulopathic patients is depicted in Table 2.
Table 2.
Baseline characteristics of coagulopathic and non-coagulopathic patients
| Coagulopathic patients (n = 136) | Non-coagulopathic patients (n = 104) | P value | |
| RBCs prior to trial drug, units (n) | 8.4 ± 1.6 (134) | 8.4 ± 1.4 (98) | 1.00 |
| FFP prior to trial drug, ml (n) | 922 ± 627 (102) | 95 ± 178 (88) | <0.001 |
| Platelets prior to trial drug, ml (n) | 126 ± 181 (128) | 0 ± 0 (100) | <0.001 |
| Cryoprecipitate prior to trial drug, ml (n) | 28 ± 78 (135) | 0 ± 0 (104) | <0.001 |
| FFP after trial drug to 48 hours, ml (n) | 1,596 ± 1,777 (102) | 1,499 ± 1,927 (88) | 0.72 |
| Platelets after trial drug to 48 hours, ml (n) | 289 ± 341 (127) | 319 ± 432 (100) | 0.57 |
| Cryoprecipitate after trial drug to 48 hours, ml (n) | 56 ± 151 (135) | 33 ± 121 (104) | 0.19 |
| Injury severity score (n) | 30 ± 13 (131) | 26 ± 13 (104) | 0.02 |
| Temperature, °C (n) | 35.1 ± 1.4 (92) | 35.2 ± 1.5 (62) | 0.68 |
| Mean arterial pressure, mm Hg (n) | 76 ± 22 (132) | 74 ± 18 (101) | 0.45 |
| pH (n) | 7.28 ± 0.11 (130) | 7.24 ± 0.12 (101) | 0.01 |
| Hematocrit, percentage (n) | 25 ± 8 (104) | 28 ± 9 (83) | 0.02 |
| aPTT, seconds (n) | 50 ± 25 (79) | 54 ± 30 (51) | 0.43 |
| PT, seconds (n) | 19 ± 6 (90) | 21 ± 6 (58) | 0.05 |
| Platelet count, × 109 (n) | 78 ± 45 (122) | 70 ± 47 (98) | 0.20 |
| Fibrinogen, g/l (n) | 1.3 ± 0.7 (90) | 1.2 ± 1.2 (58) | 0.57 |
| 48-hour mortality, n (percentage) | 21 (15) | 20 (19) | 0.44 |
| 30-day mortality, n (percentage) | 32 (24) | 29 (28) | 0.44 |
Data are mean ± standard deviation or number (percentage). aPTT, activated partial thromboplastin time; FFP, fresh frozen plasma; PT, prothrombin time; RBC, red blood cell.
Baseline characteristics were broadly concordant between non-coagulopathic and coagulopathic patients, with the exception of significant differences in the use of FFP, platelets, and cryoprecipitate (the basis for the definition of coagulopathy) and differences in hematocrit, prothrombin time (PT) and pH (also reflective of coagulopathy), and injury severity score (Table 2). Of note, the two groups had similar baseline laboratorial coagulation profiles, including activated partial thromboplastin time (aPTT), PT, platelet count, and fibrinogen levels. Table 2 also provides data on the use of FFP, platelets, and cryoprecipitate from time of administration of trial drug to 48 hours.
The remaining analysis will focus exclusively on the coagulopathic patients. The baseline characteristics of injury severity score and physiological and coagulation variables were comparable between the placebo- and rFVIIa-treated coagulopathic patient groups, with no significant differences between groups (Table 3).
Table 3.
Baseline clinical and biological characteristics of coagulopathic patients in the placebo and rFVIIa groups
| Placebo group (n = 76) | rFVIIa group (n = 60) | |
| Age (years) | 34 ± 12 | 31 ± 11 |
| Gender | ||
| Men | 63 (83%) | 51 (85%) |
| Women | 13 (17%) | 9 (15%) |
| Type of trauma | ||
| Penetrating | 38 (50%) | 35 (58%) |
| Blunt | 38 (50%) | 25 (42%) |
| Injury severity score | 30 ± 13 | 30 ± 13 |
| Number of body regions injured | ||
| 1 | 16 (21%) | 13 (22%) |
| 2–3 | 40 (53%) | 29 (48%) |
| >3 | 18 (24%) | 17 (28%) |
| Unknown | 2 (3%) | 1 (2%) |
| Systolic blood pressure (mm Hg) | 103 ± 26 | 109 ± 31 |
| Mean arterial pressure (mm Hg) | 74 ± 22 | 78 ± 23 |
| Body temperature (°C) | 35.2 ± 1.6 | 35.6 ± 1.1 |
| pH | 7.27 ± 0.11 | 7.29 ± 0.10 |
| Hematocrit (percentage) | 23 ± 8 | 26 ± 7 |
| aPTT (seconds) | 54 ± 24 | 46 ± 26 |
| PT (seconds) | 20 ± 5 | 17 ± 7 |
| Fibrinogen (g/l) | 1.3 ± 0.8 | 1.4 ± 0.6 |
| Platelets (× 109) | 70 ± 42 | 87 ± 47 |
Data are mean ± standard deviation or number (percentage). No significant statistical differences between groups were observed. aPTT, activated partial thromboplastin time; PT, prothrombin time; rFVIIa, recombinant activated factor VII.
rFVIIa significantly reduced 48-hour RBC requirements by 2.6 units (all patients) and 3.5 units (48-hour survivors) compared with placebo (Table 4). Irrespective of whether the analysis included all or only 48-hour survivors, the need for FFP was also significantly reduced by rFVIIa treatment whereas platelet requirement was significantly reduced only among the 48-hour survivors (Table 4). Massive transfusion was found to be significantly reduced in patients surviving more than 48 hours who received rFVIIa as compared with placebo (P = 0.003, RRR 79%, 95% CI 32% to 93%) (Figure 2) but not when all patients were included. Treatment with rFVIIa was associated with an even greater reduction in exposure to RBCs, FFP, and platelets in patients surviving more than 48 hours (Table 4). In these patients, all blood-product requirements were more than halved in the rFVIIa group.
Table 4.
Transfusion requirements during the 48 hours after the first dose of trial drug in the placebo and rFVIIa groups
| Placebo group | rFVIIa group | ||||||
| n | Median (range) | n | Median (range) | Differences in medians | Estimated reduction: median of differences (95% CI)a | P valueb | |
| RBC (units) | |||||||
| All patients | 76 | 6.5 (0–41) | 60 | 4.4 (0–39.9) | 2.1 | 2.6 (0.1; 5.1) | 0.02 |
| Alive at 48 hours | 65 | 6.6 (0–41) | 48 | 2.9 (0–20) | 3.7 | 3.5 (1.7; 5.7) | <0.001 |
| FFP (ml) | |||||||
| All patients | 60 | 1,360 (0–6,912) | 42 | 705 (0–9,000) | 655 | 600 (0.00; 1,320) | 0.04 |
| Alive at 48 hours | 54 | 1,400 (0–6,912) | 35 | 660 (0–9,000) | 740 | 800 (250.0; 1,420) | 0.001 |
| Platelets (ml) | |||||||
| All patients | 72 | 300 (0–1,500) | 55 | 147 (0–1,200) | 153 | 50 (0; 250) | 0.09 |
| Alive at 48 hours | 62 | 300 (0–1,500) | 46 | 100 (0–900) | 200 | 50 (0; 250) | 0.01 |
aThe Hodges-Lehman shift with 95% CI. Patients who died within 48 hours were assigned the highest rank for the Wilcoxon-Mann-Whitney test and the Hodges-Lehman estimate. bTwo-sided Wilcoxon-Mann-Whitney rank sum test. CI, confidence interval; FFP, fresh frozen plasma; RBC, red blood cell; rFVIIa, recombinant activated factor VII.
Figure 2.
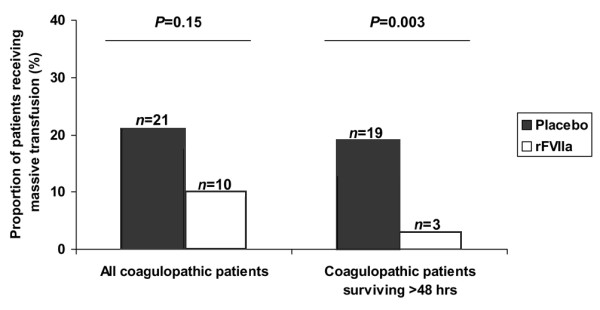
Comparison of the proportion of patients (all coagulopathic patients as well as coagulopathic patients surviving more than 48 hours) requiring massive transfusion. Massive transfusion was defined as more than 12 red blood cell (RBC) units within 48 hours of the first dose, which equals more than 20 units of RBCs (inclusive of the 8 pre-dose units) in the placebo and recombinant activated factor VII (rFVIIa) groups.
The summation of the baseline characteristics (including causes of death) of the coagulopathic patients who died early (<48 hours) is presented in Table 5. Placebo and rFVIIa groups were similar in all aspects except for a higher prevalence of penetrating injuries among those treated with rFVIIa. Sixteen of the 21 early deaths (76%) were due to exsanguination, indicating that failure to halt bleeding in patients transfused with 8 units of RBCs in the first hours is often fatal. Of note, the patients who died early had a markedly prolonged aPTT/PT but not as abnormal a platelet count or fibrinogen level.
Table 5.
Baseline clinical and biological characteristics of coagulopathic patients who died early (within 48 hours)
| Placebo group | rFVIIa group | |
| (n = 10) | (n = 11) | |
| Age (years) | 39 ± 12 | 30 ± 9 |
| Gender | ||
| Men | 7 (70%) | 11 (100%) |
| Women | 3 (30%) | 0 (0%) |
| Type of trauma | ||
| Penetrating | 4 (40%) | 8 (73%) |
| Blunt | 6 (60%) | 3 (27%) |
| Injury severity score | 34 ± 13 | 37 ± 8 |
| Number of body regions injured | ||
| 1 | 1 (10%) | 2 (18%) |
| 2–3 | 6 (60%) | 7 (64%) |
| >3 | 3 (30%) | 2 (18%) |
| Unknown | 0 (0%) | 0 (0%) |
| Systolic blood pressure (mm Hg) | 87 ± 22 | 103 ± 34 |
| Mean arterial pressure (mm Hg) | 63 ± 17 | 68 ± 32 |
| Body temperature (°C) | 34.1 ± 2.5 | 35.2 ± 1.2 |
| pH | 7.28 ± 0.10 | 7.23 ± 0.09 |
| Hematocrit (percentage) | 26 ± 14 | 19 ± 4 |
| aPTT (seconds) | 93 ± 44 | 78 ± 32 |
| PT (seconds) | 25 ± 6 | 25 ± 7 |
| Fibrinogen (g/l) | 0.8 ± 0.3 | 0.7 ± 0.3 |
| Platelets (× 109) | 42 ± 51 | 61 ± 35 |
| Causes of death | ||
| Exsanguination | 7 (70%) | 9 (82%) |
| Organ failure | 3 (30%) | 1(9%) |
| Cardiac injury | 0 (0%) | 1 (9%) |
aPTT, activated partial thromboplastin time; PT, prothrombin time; rFVIIa, recombinant activated factor VII.
Results for investigator-reported clinical complications and mortality within 30 days are summarized in Table 6. Treatment with rFVIIa significantly reduced the incidence of ARDS among all coagulopathic patients (P = 0.04, RRR 86%, 95% CI 0% to 98%, NNT 9.83, 95% CI NNT 5.15 to 88.25) and among patients surviving more than 48 hours (P = 0.04, RRR 85%, 95% CI 0% to 98%). rFVIIa also significantly reduced the combined endpoint of MOF and/or ARDS among all coagulopathic patients (P = 0.004, RRR 83%, 95% CI 29% to 96%, NNT 6.10, 95% CI NNT 3.71 to 18.23) and among patients surviving more than 48 hours (P = 0.004, RRR 90%, 95% CI 23% to 99%) (Table 6).
Table 6.
Adverse events and clinical outcomes in the placebo and rFVIIa groups
| All coagulopathic patients | Placebo group (n = 76) | rFVIIa group (n = 60) | P value |
| Thromboembolic events | 3 (4%) | 2 (3%) | 1.00 |
| Ventilator-free days | 21 (0–29) | 23 (0–29) | 0.4 |
| ICU-free days | 12 (0–29) | 18 (0–29) | 0.3 |
| Critical complication within 30 days | |||
| ARDS | 9 (12%) | 1 (2%) | 0.04 |
| MOF | 10 (13%) | 2 (3%) | 0.07 |
| ARDS/MOF | 15 (20%) | 2 (3%) | 0.004 |
| Death | 18 (24%) | 14 (24%) | 1.00 |
| ARDS/MOF/death | 25 (33%) | 14 (23%) | 0.26 |
| Death within 48 hours | 10 (13%) | 11 (18%) | 0.48 |
| Coagulopathic patients surviving more than 48 hours | Placebo group (n = 66) | rFVIIa group (n = 49) | P value |
| Thromboembolic events | 3 (5%) | 1 (2%) | 0.64 |
| Ventilator-free days | 23 (0–29) | 25 (0–29) | 0.08 |
| ICU-free days | 16 (0–29) | 20 (0–29) | 0.06 |
| Critical complications within 30 days | |||
| ARDS | 9 (14%) | 1 (2%) | 0.04 |
| MOF | 8 (12%) | 1 (2%) | 0.08 |
| ARDS/MOF | 13 (20%) | 1 (2%) | 0.004 |
| Death | 8 (12%) | 3 (6%) | 0.4 |
| ARDS/MOF/death | 15 (23%) | 3 (6%) | 0.02 |
Data are median (range) or number (percentage). ARDS, acute respiratory distress syndrome; ICU, intensive care unit; MOF, multiple organ failure; rFVIIa, recombinant activated factor VII.
Discussion
In trauma patients with coagulopathic hemorrhage, rFVIIa is emerging as a potentially valuable new damage-control tool for use when hemorrhage is refractory to standard-of-care treatment [9,15,22,27-30]. The analysis reported here is based on data from two randomized parallel controlled trials in severely injured patients [22]. In these trials, rFVIIa reduced the need for blood transfusion in blunt trauma patients surviving for 48 hours and with a trend toward less RBC transfusion in patients with penetrating trauma. At study entry, it was not possible to identify this coagulopathic subgroup of patients, because available routine laboratory testing (aPTT, PT, platelet count, and fibrinogen levels) did not accurately identify clinically significant coagulopathic bleeding. The platelet count does not reflect platelet-impaired function such as in hypothermia and acidosis, typically present in the massively bleeding trauma victim [31]. PT and aPTT are poor predictors of clinical bleeding unless a marked prolongation (that is, prolongation beyond the limit of machine measurements) is observed [30]. Because blood samples are typically re-warmed to 37°C, there is an underestimation of coagulopathy in hypothermic conditions typical of critical trauma patients [31]. In addition, the time required for these routine tests as well as for a more thorough analysis of coagulation state to be performed – approximately 45 minutes – precludes an accurate 'real time' reflection because the patients are usually massively transfused and infused during the time period elapsing between sampling to results [12]. Although there are no universally accepted laboratory standards for the definition of coagulopathy in these severely traumatized patients (see Table 1 for a summary of differing definitions found in the trauma literature), the clinical diagnosis of coagulopathy is familiar to most intensivists and surgeons. This is characterized by the clinical assessment of ongoing bleeding and the observation of oozing from cut surfaces, intravascular catheter sites, or mucus membranes [31].
Our post-hoc analyses identified patients who were believed by their treating physicians to have clinically significant coagulopathic bleeding, as reflected by the empirical replacement therapy that was administered. In this group, treatment with rFVIIa significantly reduced the need for all blood products, surrogate markers of bleeding, as well as potential donor exposure as compared with placebo during standard-of-care management of hemorrhage (Table 4). Furthermore, in these coagulopathic patients, early adjunctive treatment with rFVIIa had a significant effect on the risk for developing MOF and ARDS in the 30 days after traumatic injury (Table 5).
Our analyses of data also identified a significant effect of rFVIIa treatment on patients' requirement for massive RBC transfusion in the first 48 hours of the study in patients surviving more than 48 hours. Approximately 29% of coagulopathic patients in the placebo group required an additional 12 units of RBC transfusion (to the initial 8 units prior to trial drug) to manage ongoing hemorrhage as compared with a much-reduced need for massive transfusion in the rFVIIa-treated coagulopathic group, in which only 6% of patients required this level of transfusion (Figure 2). Massive transfusion of this type – 20 units of RBCs administered from time of injury to assessment at 48 hours after study entry – represents ongoing hemorrhage equivalent to at least two blood volumes [32,33]. The effect of rFVIIa to arrest such massive blood loss reduces patient exposure to excessive transfusion of blood products and inherent risk factors for immunological and infectious risks. It is known that with increasing transfusion requirements, there is a greater risk of morbidity and potentially fatal complications associated with traumatic hemorrhage. This may be due in part to a correlation between the severity of trauma and transfusion needs but also in part to the negative effects of transfusions per se. Indeed, the risk of developing ARDS and MOF after trauma has been shown to correlate with increasing transfusion requirements [34,35]. Our analysis of data from coagulopathic patients treated with adjunctive rFVIIa revealed a significant improvement in clinical outcome as compared with placebo. Significant reductions in the combined endpoint of ARDS and/or MOF were seen in rFVIIa-treated subjects at day 30, when these complications occurred in just 3% of patients as compared with a rate for ARDS and/or MOF of one out of every five placebo-treated coagulopathic subjects (Table 5).
RFVIIa significantly reduced the incidence of ARDS among all patients. Considering only the patients surviving more than 48 hours, ARDS (2%) or the combined endpoint of ARDS and/or MOF (2%) and the combined endpoint of ARDS/MOF/death (6%) were also significantly reduced up to day 30 in the group that received rFVIIa treatment, in contrast to a 14% rate of ARDS, a 20% rate of ARDS or MOF, and a 23% rate of death, MOF, or ARDS in placebo-treated subjects over the same follow-up period. Within this subgroup, it was shown that treatment with rFVIIa was particularly beneficial in effecting a reduction in the primary clinical endpoint of RBC requirements during 48 hours (Table 4). We noted a 3.5-unit reduction in RBC transfusion associated with treatment. The reductions in RBC requirement in this subgroup were accompanied by a similar reduction in FFP of 800 ml and reduced platelet requirements of 50 ml, in essence halving transfusion requirements (Table 4).
This study was designed with the intent of being hypothesis-generating and has limitations that deserve comment. It is a post-hoc analysis of the only RCT on the use of rFVIIa in trauma to date. The original RCT has pitfalls, some of which are inherent to clinical trials designed to study severely traumatized and actively bleeding patients during the earliest and most acute phase of resuscitation. One limitation was the difficulty of establishing uniform standards of care among 23 different institutions spread across eight countries. The original trial elected to use blood transfusion as a surrogate marker of bleeding, a widely accepted but still imperfect marker. Whereas the original RCT analyzed blunt and penetrating trauma patients separately, considering the smaller patient sample of coagulopathic patients available, the present study analyzed all coagulopathic patients combined, irrespective of the mechanism of injury. The definition of coagulopathy used is limited and imperfect because it permits a patient diagnosed as coagulopathic but for any reason not treated with blood products to be excluded from this analysis. In addition, the expectation was that coagulopathy secondary to either blunt or penetrating trauma would equally respond (or not) to the intervention. The present study also analysed the data both including all patients and excluding those who died early, thus repeating the analysis performed in the original RCT.
Despite the limitations, the findings of our post-hoc analysis of a subgroup of patients support the premise that rFVIIa is a valuable addition to the therapeutic armamentarium in the management of severe trauma, helping to arrest life-threatening coagulopathic hemorrhage, reducing transfusion requirements and associated risks, and having the potential to impact on the longer term morbidity and mortality associated with traumatic bleeding [9,15,22,27,28,36]. Moreover, our analysis identified clinically coagulopathic patients as the high-risk group of trauma patients who might benefit the most from rFVIIa therapy. Considering the limited therapeutic options and the high mortality associated with post-traumatic diffuse coagulopathy, this study supports the validity of considering the use of rFVIIa in the management of these patients. However, the hypothesis generated by this post-hoc analysis requires corroboration from other studies before any definitive recommendation can be advised.
Conclusion
This post-hoc analysis supports the assertion that coagulopathy is common in patients with severe trauma. Of the 277 trauma patients included in a clinical trial after receiving 8 units of RBCs, 49% were identified as coagulopathic (136 patients). There is, however, little agreement on a diagnosis for traumatic coagulopathy or on its objective measurement.
The results of this study suggest that the subgroup of coagulopathic trauma patients receive particular benefit from rFVIIa therapy. Compared to a control group, coagulopathic patients treated with rFVIIa required significantly less blood transfusion with reductions in RBCs, FFP, platelets, and massive transfusions. The use of rFVIIa led to a reduction in ARDS and/or MOF and did not increase thromboembolic complications. Considering the mortality and limited therapeutic options, this study supports the concept of considering rFVIIa for the management of trauma patients with coagulopathy.
Key messages
• Coagulopathy is common in severe trauma and lacks objective definition.
• Administration of rFVIIa to coagulopathic trauma patients significantly reduces the need for blood and blood-product transfusion.
• Administration of rFVIIa to coagulopathic trauma patients reduces the incidence of ARDS and/or MOF without increasing thromboembolic complications.
• Coagulopathic trauma patients appear to benefit from rFVIIa therapy.
Abbreviations
aPTT = activated partial thromboplastin time; ARDS = acute respiratory distress syndrome; CI = confidence interval; FFP = fresh frozen plasma; ICU = intensive care unit; MOF = multiple organ failure; NNT = numbers needed to treat; PT = prothrombin time; RBC = red blood cell; RCT = randomized controlled trial; rFVIIa = recombinant activated factor VII; RRR = relative risk reductions; TBI = traumatic brain injury.
Competing interests
SBR, KDB, YK, RR, and BR have received lecture and/or consultancy fees from Novo Nordisk A/S. RR has received lecture sponsorship from Novo Nordisk A/S. SBR is a member of the Scientific International Advisory Board for rFVIIa. Novo Nordisk A/S is financing the article-processing charge. MT is an employee of Novo Nordisk A/S. BW and PI declare that they have no competing interests.
Authors' contributions
All authors made substantive intellectual contributions to the making of this manuscript and have given final approval of the version to be published. SBR, KDB, BR, BW, PI, YK, and RR were co-principal investigators in the original RCT. SBR, KDB, BR, BW, PI, YK, RR, and MT made substantial contributions to the conception and design of the study and to the analysis and interpretation of data and were involved in drafting the manuscript and revising it critically. All authors read and approved the final manuscript.
Appendix
Data and safety monitoring board: Howard Champion, Annapolis, MD, USA (chairman); Abe Fingerhut Paris, France; Richard Weiskopf, San Francisco, CA, USA; Miguel A Escobar, Houston, TX, USA. Ad hoc member: Torben Sörensen (statistician), StatCon Aps, Alleroed, Denmark.
Sponsor: Novo Nordisk A/S, Bagsværd, Denmark.
Statistician: Tine Sörensen, MSc, Novo Nordisk A/S, Bagsværd, Denmark.
Investigators of the NovoSeven® Trauma Study Group and Trial centers: South Africa: KD Boffard, Johannesburg General Hospital, Johannesburg; BL Warren, Tygerberg Hospital, Cape Town; A Nicol, Groote Schuur Hospital, Cape Town; R Tracey, Unitas Hospital, Centurion; JSS Marx, Pretoria Academic Hospital, Pretoria; E Degiannis, Chris Hani Baragwanath Hospital, Johannesburg; J Goosen, Milpark Hospital, Johannesburg; F Plani, Union Hospital, Alberton; LM Fingleson, Sunninghill Hospital, Sandton. France: B Riou, Hôpital Pitié Salpêtrière, Paris; JF Payen de La Garanderie, Hôpital Michallon, Grenoble; J Marty, Hôpital Beaujon, Clichy; R Krivosic-Horber, Hôpital Roger Salengro, Lille; M Freysz, Hôpital Général, Dijon; JE de La Coussaye, Centre Hospitalier Universitaire, Nîmes; J Duranteau, Hôpital de Bicêtre, Le Kremlin Bicêtre; B Francois, Hôpital Dupuytren, Limoges; N Smail, Hôpital Purpan, Toulouse; P Petit, Hôpital Edouard Herriot, Lyon; Germany: R Rossaint, Klinik für Anästhesie Universitätsklinikum Aachen, Aachen; HK van Aken, Universitätsklinikum Münster, Münster; G Hempelmann, Universitätsklinikum Giessen, Giessen. Israel: Y Kluger, Sourasky Medical Centre, Tel Aviv; A I Rivkind, Hadassah Medical Organisation, Jerusalem; G Shaked, Soroka Medical Centre, Beer Sheva; M Michaelson, Rambam Medical Centre, Haifa. Singapore: P Iau Tsau Choong, National University Hospital; A Yeo Wan Yan, Singapore General Hospital. Canada: SB Rizoli, Sunnybrook Health Sciences Centre, Toronto; SM Hameed, Foothills Medical Centre, Calgary. United Kingdom: GS Samra, The Royal London Hospital, London. Australia: GJ Dobb, Royal Perth Hospital, Perth.
The author group contributed significantly to the development of the protocol. In addition, the following contributed: USA: JA Asensio, Los Angeles, CA; W Biffl, Denver, CO; K Mattox and J Holcomb, Houston, TX; JH Patton, Detroit, MI; F Lewis, Pittsburgh, PA; M Lynn, Miami, FL; P O'Niel, Brooklyn, NY; JT Owings, Sacramento, CA; A Pietsman and S Tisherman, Pittsburgh, PA; TM Scalea, Baltimore, MD; and M Schreiber, Portland, OR.
Contributor Information
Sandro B Rizoli, Email: sandro.rizoli@sw.ca.
Kenneth D Boffard, Email: kdboffard@pixie.co.za.
Bruno Riou, Email: bruno.riou@psl.aphp.fr.
Brian Warren, Email: blw@sun.ac.za.
Philip Iau, Email: surv6@nus.edu.sg.
Yoram Kluger, Email: y_kluger@rambam.health.gov.il.
Rolf Rossaint, Email: rossaint@post.rwth-aachen.de.
Michael Tillinger, Email: mcrc@novonordisk.com.
References
- Hoyt DB. A clinical review of bleeding dilemmas in trauma. Semin Hematol. 2004;41(1 Suppl 1):40–43. doi: 10.1053/j.seminhematol.2003.11.009. [DOI] [PubMed] [Google Scholar]
- Sauaia A, Moore FA, Moore EE, Moser KS, Brennan R, Read RA, Pons PT. Epidemiology of trauma deaths: a reassessment. J Trauma. 1995;38:185–193. doi: 10.1097/00005373-199502000-00006. [DOI] [PubMed] [Google Scholar]
- Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997;349:1269–1276. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- Peden M, McGee K, Sharma G. The Injury Chart Book: A Graphical Overview of the Global Burden of Injuries. Geneva: World Health Organization; 2002. [Google Scholar]
- WHO report 2003: The World Health Report 2003 'Shaping the Future' http://www.who.int
- Brohi K, Singh J, Heron M, Coats T. Acute traumatic coagulopathy. J Trauma. 2003;54:1127–1130. doi: 10.1097/01.TA.0000069184.82147.06. [DOI] [PubMed] [Google Scholar]
- MacLeod JB, Lynn M, McKenney MG, Cohn SM, Murtha M. Early coagulopathy predicts mortality in trauma. J Trauma. 2003;55:39–44. doi: 10.1097/01.TA.0000075338.21177.EF. [DOI] [PubMed] [Google Scholar]
- Stehling IC, Task Force Practice guidelines for blood component therapy: A report by the American Society of Anesthesiologists Task Force on Blood Component Therapy. Anesthesiology. 1996;84:732–747. doi: 10.1097/00000542-199603000-00032. [DOI] [PubMed] [Google Scholar]
- Dutton RP, McCunn M, Hyder M, D'Angelo M, O'Connor J, Hess JR, Scalea TM. Factor VIIa for correction of traumatic coagulopathy. J Trauma. 2004;57:709–719. doi: 10.1097/01.ta.0000140646.66852.ab. [DOI] [PubMed] [Google Scholar]
- Cosgriff N, Moore EE, Sauaia A, Kenny-Moynihan M, Burch JM, Galloway B. Predicting life-threatening coagulopathy in the massively transfused trauma patient: hypothermia and acidoses revisited. J Trauma. 1997;42:857–861. doi: 10.1097/00005373-199705000-00016. [DOI] [PubMed] [Google Scholar]
- Mayo A, Misgav M, Kluger Y, Geenberg R, Pauzner D, Klausner J, Ben-Tal O. Recombinant activated factor VII (NovoSeven): addition to replacement therapy in acute, uncontrolled and life-threatening bleeding. Vox Sang. 2004;87:34–40. doi: 10.1111/j.1423-0410.2004.00533.x. [DOI] [PubMed] [Google Scholar]
- Hardy JF, De Moerloose P, Samama M, Groupe d'interet en Hemostase Perioperatoire Massive transfusion and coagulopathy: pathophysiology and implications for clinical management. Can J Anaesth. 2004;51:293–310. doi: 10.1007/BF03018233. [DOI] [PubMed] [Google Scholar]
- Monroe DM, Hoffman M, Oliver JA, Roberts HR. Platelet activity of high-dose factor VIIa is independent of tissue factor. Br J Haematol. 1997;99:542–547. doi: 10.1046/j.1365-2141.1997.4463256.x. [DOI] [PubMed] [Google Scholar]
- Monroe DM, Hoffman M, Oliver JA, Roberts HR. A possible mechanism of action of activated factor VII independent of tissue factor. Blood Coagul Fibrinolysis. 1998;9 Suppl 1():S15–S20. [PubMed] [Google Scholar]
- Martinowitz U, Michaelson M, The Israeli Multidisciplinary rFVIIa Task Force Guidelines for the use of recombinant activated factor VII (rFVIIa) in uncontrolled bleeding: a report by the Israeli Multidisciplinary rFVIIa Task Force. J Thromb Haemost. 2005;3:640–648. doi: 10.1111/j.1538-7836.2005.01203.x. [DOI] [PubMed] [Google Scholar]
- Barletta JF, Ahrens CL, Tyburski JG, Wilson RF. A review of recombinant factor VII for refractory bleeding in nonhemophilic trauma patients. J Trauma. 2005;58:646–651. doi: 10.1097/01.ta.0000154561.97961.ad. [DOI] [PubMed] [Google Scholar]
- Ahonen J, Jokela R. Recombinant factor VIIa for life-threatening post-partum haemorrhage. Br J Anaesth. 2005;94:592–595. doi: 10.1093/bja/aei094. [DOI] [PubMed] [Google Scholar]
- Segal S, Shemesh IY, Blumental R, Yoffe B, Laufer N, Mankuta D, Mazor M, Zohar S, Schiff E, Martinovitz U. The use of recombinant factor VIIa in severe postpartum hemorrhage. Acta Obstet Gynecol Scand. 2004;83:771–772. doi: 10.1111/j.0001-6349.2004.00501.x. [DOI] [PubMed] [Google Scholar]
- Hyllner M, Houltz E, Jeppsson A. Recombinant activated factor VII in the management of life-threatening bleeding in cardiac surgery. Eur J Cardiothorac Surg. 2005;28:254–258. doi: 10.1016/j.ejcts.2005.04.021. [DOI] [PubMed] [Google Scholar]
- Raivio P, Suojaranta-Ylinen R, Kuitunen AH. Recombinant factor VIIa in the treatment of postoperative hemorrhage after cardiac surgery. Ann Thorac Surg. 2005;80:66–71. doi: 10.1016/j.athoracsur.2005.02.044. [DOI] [PubMed] [Google Scholar]
- Karkouti K, Beattie WS, Wijeysundera DN, Yau TM, McCluskey SA, Ghannam M, Sutton D, van Rensburg A, Karski J. Recombinant factor VIIa for intractable blood loss after cardiac surgery: a propensity score-matched case-control analysis. Transfusion. 2005;45:26–34. doi: 10.1111/j.1537-2995.2005.04216.x. [DOI] [PubMed] [Google Scholar]
- Boffard KD, Riou B, Warren B, Choong PI, Rizoli S, Rossaint R, Axelsen M, Kluger Y, NovoSeven Trauma Study Group Recombinant factor VIIa as adjunctive therapy for bleeding control in severely injured trauma patients: two parallel randomized, placebo-controlled, double-blind clinical trials. J Trauma. 2005;59:8–18. doi: 10.1097/01.ta.0000171453.37949.b7. [DOI] [PubMed] [Google Scholar]
- Stein SC, Young GS, Talucci RC, Greenbaum BH, Ross SE. Delayed brain injury after head trauma: significance of coagulopathy. Neurosurgery. 1992;30:160–165. doi: 10.1227/00006123-199202000-00002. [DOI] [PubMed] [Google Scholar]
- Riou B, Landais P, Vivien B, Stell P, Labbene I, Carli P. Distribution of the probability of survival is a strategic issue for randomized trials in critically ill patients. Anesthesiology. 2001;95:56–63. doi: 10.1097/00000542-200107000-00014. [DOI] [PubMed] [Google Scholar]
- Montori VM, Permanyer-Miralda G, Ferreira-Gonzalez I, Busse JW, Pacheco-Huergo V, Bryant D, Alonso J, Akl EA, Domingo-Salvany A, Mills E, et al. Validity of composite end points in clinical trials. BMJ. 2005;330(7491):594–596. doi: 10.1136/bmj.330.7491.594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Manach Y, Perel A, Coriat P, Godet G, Bertrand M, Riou B. Early and delayed myocardial infarction after abdominal aortic surgery. Anesthesiology. 2005;102:885–891. doi: 10.1097/00000542-200505000-00004. [DOI] [PubMed] [Google Scholar]
- Grounds M. Recombinant factor VIIa (rFVIIa) and its use in severe bleeding in surgery and trauma: a review. Blood Reviews. 2003;17:S11–S21. doi: 10.1016/S0268-960X(03)90002-6. [DOI] [PubMed] [Google Scholar]
- Spivey M, Parr MJ. Therapeutic approaches in trauma-induced coagulopathy. Minerva Anestesiol. 2005;71:281–289. [PubMed] [Google Scholar]
- Schreiber MA. Damage control surgery. Crit Care Clin. 2004;20:101–118. doi: 10.1016/S0749-0704(03)00095-2. [DOI] [PubMed] [Google Scholar]
- ASA Transfusion Practice 3rd edition: Questions and Answers About Transfusion Practices. Third http://www.asahq.org/publicationsAndServices/transfusion.pdf [Google Scholar]
- Lynn M, Jeroukhimov I, Klein Y, Martinowitz U. Updates in the management of severe coagulopathy in trauma patients. Intensive Care Med. 2002;28 Suppl 2():S241–S247. doi: 10.1007/s00134-002-1471-7. [DOI] [PubMed] [Google Scholar]
- Erber WN. Massive blood transfusion in the elective surgical setting. Transfus Apher Sci. 2002;27:83–92. doi: 10.1016/S1473-0502(02)00029-0. [DOI] [PubMed] [Google Scholar]
- Stainsby D, MacLennan S, Hamilton PJ. Management of massive blood loss: a template guideline. Br J Anaesth. 2000;85:487–491. doi: 10.1093/bja/85.3.487. [DOI] [PubMed] [Google Scholar]
- Como JJ, Dutton RP, Scalea TM, Edelman BB, Hess JR. Blood transfusion rates in the care of acute trauma. Transfusion. 2004;44:809–813. doi: 10.1111/j.1537-2995.2004.03409.x. [DOI] [PubMed] [Google Scholar]
- Gong MN, Thompson BT, Williams P, Pothier L, Boyce PD, Christiani DC. Clinical predictors of and mortality in acute respiratory distress syndrome: potential role of red cell transfusion. Crit Care Med. 2005;33:1191–1198. doi: 10.1097/01.CCM.0000165566.82925.14. [DOI] [PubMed] [Google Scholar]
- Goodnough LT, Lublin DM, Zhang L, Despotis G, Eby C. Transfusion medicine service policies for recombinant factor VIIa administration. Transfusion. 2004;44:1325–1331. doi: 10.1111/j.1537-2995.2004.04052.x. [DOI] [PubMed] [Google Scholar]
- Vaslef SN, Knudsen NW, Neligan PJ, Sebastian MW. Massive transfusion exceeding 50 units of blood products in trauma patients. J Trauma. 2002;53:291–295. doi: 10.1097/00005373-200208000-00017. [DOI] [PubMed] [Google Scholar]


