Abstract
Objective
To examine the relationship between Medicaid case-mix payment and nursing home resident acuity.
Data Sources
Longitudinal Minimum Data Set (MDS) resident assessments from 1999 to 2002 and Online Survey Certification and Reporting (OSCAR) data from 1996 to 2002, for all freestanding nursing homes in the 48 contiguous U.S. states.
Study Design
We used a facility fixed-effects model to examine the effect of introducing state case-mix payment on changes in nursing home case-mix acuity. Facility acuity was measured by aggregating the nursing case-mix index (NCMI) from the MDS using the Resource Utilization Group (Version III) resident classification system, separately for new admits and long-stay residents, and by an OSCAR-derived index combining a range of activity of daily living dependencies and special treatment measures.
Data Collection/Extraction Methods
We followed facilities over the study period to create a longitudinal data file based on the MDS and OSCAR, respectively, and linked facilities with longitudinal data on state case-mix payment policies for the same period.
Principal Findings
Across three acuity measures and two data sources, we found that states shifting to case-mix payment increased nursing home acuity levels over the study period. Specifically, we observed a 2.5 percent increase in the average acuity of new admits and a 1.3 to 1.4 percent increase in the acuity of long-stay residents, following the introduction of case-mix payment.
Conclusions
The adoption of case-mix payment increased access to care for higher acuity Medicaid residents.
Keywords: Case-mix payment, acuity, access to care, nursing homes
A number of studies have observed that access to nursing home care for Medicaid recipients is delayed relative to private-paying individuals (Feder and Scanlon 1980; Shapiro, Roos, and Kavanagh 1980; Friedman 1982; Greenless, Marshall, and Yett 1982; Gruenberg and Willemain 1982; Weissert and Cready 1988; U.S. General Accounting Office 1990; Ettner 1993; Reschovsky 1996). Moreover, many of these studies indicate that functionally more dependent, or “heavy care,” Medicaid recipients have the longest delays in obtaining care. These individuals typically receive care in the hospital, in other long-term care settings, or informally from family and friends until they gain access to a nursing home. These delays in obtaining nursing home care significantly increase patient costs due to increased hospitalizations (U.S. General Accounting Office 1990), and may negatively affect health care outcomes if patients are not receiving the appropriate care.
Over the last two decades, there has been a substantial increase in the number of states adopting case-mix adjusted Medicaid payment systems, which pay nursing homes according to resident care needs (Harrington et al. 1999). By 2002, 32 states used some form of case-mix payment, up from 19 states in 1991 and just 4 states in 1981. Although there are several case-mix methods currently in practice that use alternative formulae, the majority of systems classify residents into homogeneous categories based on their estimated resource utilization. Associated with each of these categories is a case-mix index or weight, which represents, at least relatively, the time or cost of caring for the average resident in the group (Fries 1990; Fries et al. 1994). Nursing homes with a higher case-mix index score or weight, on average, would be reimbursed a higher rate. As such, case-mix adjustment is designed to achieve a more equitable distribution of Medicaid payments among providers. By compensating homes more for the “heavy care” of more disabled residents, an objective of case-mix payment is also to encourage better access to nursing home care for functionally more dependent Medicaid residents (Schlenker 1986; Murtaugh et al. 1988; Butler and Schlenker 1989; Arling and Daneman 2002).
Previous studies have generally found support for increased access for heavy-care patients under case-mix payment (Holahan and Cohen 1987; Butler and Schlenker 1989; Feder and Scanlon 1989; Schlenker 1991; Thorpe, Gertler, and Goldman 1991; Norton 1992; Arling and Daneman 2002; Grabowski 2002; Swan and Pickard 2003). However, these studies were limited in a number of important ways. First, most existing analyses were restricted to a single state or just a few states. Despite the potential of gathering data in greater detail, such localized studies are quite limited in the extent to which they can provide a broader picture on the issue of nursing home access under case-mix payment. Second, with few exceptions, most existing studies used a cross-sectional design or a simple before- and after-case-mix introduction approach, based on data observed at only two points in time (typically between 1 or 2 years apart). Thus, these studies were unable to reveal and substantiate trends over a longer time period. Finally, most existing studies have used facility-level aggregate resident acuity information, as a crude proxy for resident case mix.
This study offers new evidence on the impact of introducing Medicaid case-mix payment on nursing home resident acuity using national longitudinal data from the most recent years (1996–2002). To our knowledge, this study is the first to examine this issue using nationwide resident-level Minimum Data Set (MDS) assessments. Importantly, the MDS is employed by state Medicaid programs for case-mix classification using variants of the Resource Utilization Group (RUG) system (Fries et al. 1994), and used by the Centers for Medicare and Medicaid Services (CMS) for reimbursement of Medicare Skilled Nursing Facility (SNF) care and quality control (Mor 2004). Thus, findings from our study have important implications for state Medicaid policy with regard to the financing and delivery of nursing home care to a vulnerable segment of the population—the frail and needy elders in the U.S.
PROVIDER RESPONSE, FINANCIAL INCENTIVES AND ACCESS TO CARE UNDER CASE-MIX PAYMENT
There is ample evidence in the research literature suggesting that nursing homes tend to respond fairly quickly to major policy changes in the industry, particularly those related to Medicare or Medicaid reimbursement policies. Following the Nursing Home Reform Act (NHRA) of 1990, for instance, quality improvements were found in nursing homes nationwide, partly due to the quality and staffing regulations stipulated by the NHRA (Zhang and Grabowski 2004). The shift to Medicaid prospective payment has spurred a wide range of nursing home managerial responses, including strategies for profit maximizing by instituting cost controls and benefiting from incentives (Reid and Coburn 1996). Following the adoption of the Medicare Prospective Payment System (PPS) for SNFs in 1998, nursing homes acted to limit transaction costs involved in the provision of rehabilitation therapy services by either exiting the rehabilitation market or exerting greater control over therapy services through managing these services in-house as opposed to outside contracting (Zinn et al. 2003). Meanwhile, in response to Medicare PPS and associated rate cuts, nursing home professional staffing levels were found to have decreased and regulatory deficiencies increased, but these negative effects were mitigated with the subsequent rate increases mandated by the Balanced Budget Refinement Act (BBRA) of 2000 (Konetzka et al. 2004).
The implementation of Medicaid case-mix reimbursement has immediate implications for nursing home financing and revenues. The chronic care nursing home market has two primary payer types: Medicaid and private-pay. State Medicaid programs are responsible for approximately 50 percent of all nursing home expenditures and Medicaid recipients constitute 70 percent of all bed days (with the remainder of care financed primarily by out-of-pocket payments). The Medicaid rate (MR) is, on average, about 70 percent of the private-pay price. Despite the different rates charged Medicaid and private-pay residents, a home is required by law to provide the same level of quality to all residents within a home regardless of payer source.
Historically, researchers have assumed an excess demand paradigm when studying the nursing home market (Norton 2000). This model builds on the assumption that Certificate of Need (CON) and moratorium policies impose a binding bed constraint within the market for nursing home care whereby certain individuals are unable to gain access to care. However, there has been a significant decline in utilization over the last two decades within the nursing home market (Bishop 1999). The national occupancy rate, an indirect measure of excess demand, declined from 93 percent in 1977 to 87 percent by 1995 (Strahan 1997), and further down to 83 percent by 2003 (Gibson et al. 2004). This decline has been attributed to the growth of nursing home substitutes such as assisted living and demographic changes among the elderly. Given this change, we follow more recent work in this area by assuming a model with free entry among providers.
In this standard market-clearing model, nursing homes have an incentive to admit Medicaid recipients until the marginal cost (MC) of caring for an additional resident equals the marginal revenue associated with the predetermined Medicaid payment rate. Several studies have found that Medicaid payment rates, on average, exceed the MC of care (Nyman 1988; Mukamel and Spector 2002; Troyer 2002). In a payment system without case-mix adjustment, the incentives are strongest to first accept lighter care patients for which the differential between the MR and MC is typically largest. Case-mix payment is hypothesized to improve access to care for high acuity residents by addressing the relative size of the differential (MR–MC) across light, moderate, and high acuity residents. The likely implication of case-mix payment adoption is that high acuity residents will not be as unprofitable as they were relative to light-care residents before the payment system change, ceteris paribus. Thus, our primary hypothesis is that the implementation of case-mix adjusted payment system will increase access to care for functionally more dependent residents.
On the other hand, the observed increase in resident dependency under Medicaid case-mix payment might in some extent reflect the “up-coding” of resident conditions to higher payment categories, driven by the financial incentives embedded in the case-mix system. Such behavior is possible under any case-mix adjusted payment system. For example, the phenomenon of “DRG creep” under Medicare PPS for hospital care has been well documented (Hsia et al. 1988; Steinwald and Dummit 1989; Chulis 1991; Hsia et al. 1992; Dugan 1997), although there is evidence that most of the increase in patient acuity appeared to be justified by the increased complexity of the patients hospitalized (Carter, Newhouse, and Relles 1990).
For nursing home care, there is an additional check in that the MDS data used for setting Medicaid case-mix payment rates are also used for quality monitoring. Thus, the incentive to game the payment system is diminished, as facilities that overreport case mix can be identified as outliers on certain quality indicators, and those that underreport quality problems will limit their RUG-based payment (Zimmerman et al. 1995). In the end, the advantages of “up-coding” (to maximize reimbursement rates) might be balanced by the advantage of “down-coding” (to minimize quality-related problems and hence boost facility reputation). Indeed, a study by the Office of Inspector General reported that “up-coding” in nursing home resident assessments was no more common than “down-coding,” and concluded that both were likely due to errors rather than strategic behavior (Office of the Inspector General 2001).
STUDY DATA AND METHODS
Data
Our primary source of case-mix acuity data was the national repository of MDS resident assessments for the period 1999–2002. The MDS is a comprehensive clinical tool designed to assess the functional status and care needs of nursing home residents. Interrater reliability of items and internal consistency of MDS summary scales are generally good to excellent (Mor 2004). Individual MDS resident assessments are performed on admission, and thereafter quarterly and annually, or upon significant change in status. For each year, we extracted resident assessments separately for new admissions (defined as having no prior admission assessment on record) and for long-stay residents (based on the resident's annual assessment, if available).
We also obtained facility aggregated case-mix acuity data from the Online Survey Certification and Reporting (OSCAR) system for 1996–2002. An administrative database maintained by the CMS, OSCAR includes organizational characteristics for all Medicare/Medicaid certified nursing homes in the U.S. and aggregate resident data routinely collected as part of the licensure and certification process. The CMS contracts with each state to conduct onsite inspections, which occur every 9–15 months (on average, about once a year). Survey results are evaluated to determine whether a Medicare/Medicaid participating nursing home meets the minimum quality and performance standards established by the CMS.
Information on state Medicaid nursing home policies through 1998, including case-mix systems, average daily payment rates and CON programs, was obtained from a series of data books compiled by Harrington and colleagues (Harrington et al. 1999; Swan et al. 2000). The parallel data for the most recent years from 1999 to 2002 were collected by the authors through a recent survey of state Medicaid offices, as described elsewhere (Grabowski et al. 2004).
The complete MDS data became available nationally in 1999. Thus, the RUG-based case-mix acuity measures (detailed below) in our analysis could not be applied to earlier years. Similarly, we did not analyze OSCAR data before 1996 because some components of the OSCAR-derived acuity index (further described below) were not complete until 1996. In addition, we excluded hospital-based facilities, because they provide postacute care predominantly to Medicare-eligible residents (Grabowski, Angelelli, and Mor 2004; Mor et al. 2004). Lastly, throughout the study we included all 48 contiguous U.S. states, excluding Alaska, Hawaii, the District of Columbia, and other U.S. territories due to the small number of nursing homes in these places.
Measures of Facility Case-Mix Acuity
We characterized nursing home case-mix acuity at the facility level, using two summary indices based on the MDS data and one index derived from the OSCAR. For each index, the higher the score, the more severe the average acuity profile of the residents in the facility.
From the MDS, we computed the annual average nursing case-mix index (NCMI) score for each facility (over all individual NCMI values for all residents), separately for new admits and the long-stay residents. The resident-level NCMI was calculated in two steps, using the RUG-III resident classification system (Fries et al. 1994). First, the CMS RUG 5.12 code (44 categories in total) was used to generate a RUG classification. Second, the RUG code was converted into a NCMI value following the CMS Proposed Rule regarding Fiscal Year 2004 SNF payment policies (Centers for Medicare and Medicaid Services 2003). We anticipate the facility average NCMI will be substantially higher for new admits than for long-stay residents, because residents newly admitted to nursing homes are more likely to be Medicare beneficiaries who receive short-term subacute care.
The OSCAR-based acuity index was a modified version of that used in the 2002 edition of Nursing Home Statistical Yearbook (Cowles 2002). This index combines a range of activity of daily living (ADL) dependencies and special treatment measures for all residents in each facility, expressed as a weighted sum of specific resident characteristics, as summarized in Table 1.
Table 1.
Elements of the OSCAR-Based Case-Mix Index
| Weight | |
|---|---|
| ADL dependencies: | |
| Proportion of residents totally dependent at eating | 3 |
| Proportion of residents requiring the assistance of one or two staff with eating | 2 |
| Proportion of residents independent or requiring supervision with eating | 1 |
| Proportion of residents totally dependent at toileting | 5 |
| Proportion of residents requiring assistance of one or two staff with toileting | 3 |
| Proportion of residents independent or requiring supervision with toileting | 1 |
| Proportion of residents totally dependent at transferring | 5 |
| Proportion of residents requiring assistance of one or two staff with transferring | 3 |
| Proportion of residents independent or requiring supervision with transferring | 1 |
| Proportion of residents who are bedfast | 5 |
| Proportion of residents who are chair-bound | 3 |
| Proportion of residents who are ambulatory | 1 |
| Special treatments: | |
| Proportion of residents receiving respiratory care | 1 |
| Proportion of residents receiving suctioning | 1 |
| Proportion of residents receiving intravenous therapy | 1 |
| Proportion of residents receiving tracheotomy care | 1 |
| Proportion of residents receiving parenteral feeding | 1 |
| Proportion of residents with mental retardation* | 1 |
| Proportion of residents with dementia* | 1 |
| Proportion of residents with documented psychiatric diagnosis (excluding dementias & depression)* | 1 |
| Proportion of residents receiving tube feeding* | 1 |
| Proportion of residents receiving physical, occupational, or speech therapies* | 1 |
Source: Adapted from Nursing Home Statistical Yearbook (Cowles 2002).
Added by the authors, which were absent from the original definition.
OSCAR, On-line Survey Certification and Reporting system; ADL, activity of daily living.
Independent Variables
The key explanatory variable of interest in this study is the adoption of Medicaid case-mix adjusted payment. We followed the earlier literature in this area by employing a single dummy variable identifying the presence of a case-mix payment system in a given state and year over the period 1996–2002. We hypothesize that states that adopt a case-mix system will experience an increase in resident acuity.
The multivariate analyses controlled for the state average Medicaid payment rate, which was inflation-adjusted using the annual Consumer Price Index (CPI) published by the Bureau of Labor Statistics. In order to account for regional differences in purchasing power and the price of medical and nursing services in nursing homes, the rate was also adjusted using the area (county) wage index that the CMS routinely uses to adjust Medicare payment rates for nursing homes (and for hospitals as well). To some extent, the acuity of nursing home residents is a function of the availability of alternative long-term care arrangements in the local market, such as assisted living. To the extent that the presence of these substitutes is time-invariant, we offer an empirical strategy below to address this issue. However, in order to model potential change in these substitutes over time, we included the following variables as proxies for nursing home substitutes in each year: an indicator for whether the state had a CON program in effect for nursing homes; the percent of total Medicaid long-term care (LTC) expenditures on home and community-based services (HCBS) per state, based on time series data compiled by Burwell and colleagues (Burwell 2003; Burwell, Sredl, and Eiken 2005); and the total number of nursing home beds (aggregated from OSCAR) per 1,000 population aged 75 and older in each county (using census and population estimates data from the Census Bureau).
At the facility level, we included the following covariates as additional controls, all obtained from OSCAR: for-profit status, chain membership, number of beds, and percent of residents primarily paid by Medicare. All continuous variables were centered at the aggregate mean with proper increments to ease the interpretation of model results. Table 2 summarizes all variables (mean, and standard deviation if continuous) in the multivariate analyses.
Table 2.
Aggregate Description of All Variables in the Multivariate Regression Analysis
| Mean (SD) | ||
|---|---|---|
| OSCAR (1996–2002) | MDS (1999–2002) | |
| Facility case-mix acuity | ||
| Acuity index | 10.83 (1.59) | — |
| Mean RUG-III NCMI (admission) | — | 0.95 (0.13) |
| Mean RUG-III NCMI (long-stay) | — | 0.72 (0.07) |
| State policies | ||
| Case-mix payment (1/0) | 0.60 | 0.64 |
| CPI-adjusted Medicaid rate (in 2002 dollars) | 107.57 (23.47) | 111.64 (22.69) |
| Percent of Medicaid LTC spending on HCBS | 27.72 (11.73) | 30.24 (12.08) |
| Certificate of Need program for NHs (1/0) | 0.72 | 0.71 |
| Facility characteristics | ||
| For profit (1/0) | 0.72 | 0.72 |
| Chain membership (1/0) | 0.57 | 0.58 |
| Total number of beds | 109 (64) | 110 (63) |
| Percent of residents paid by Medicare | 8.90 (12.65) | 9.14 (12.03) |
| Market (county) characteristics | ||
| Wage index | 0.95 (0.17) | 0.95 (0.16) |
| Number of NH beds per 1,000 population 75+ | 150 (248) | 142 (140) |
| Number of observations | ||
| States | 48 | 48 |
| Counties | 2,832 | 2,796 |
| Facilities | 15,861 | 14,817 |
| Surveys | 98,862 | 56,530 |
RUG-III NCMI, Resource Utilization Group (Version III) based Nursing Case-Mix Index; MDS, Minimum Data Set; OSCAR, On-line Survey Certification and Reporting system; LTC, long-term care; NH, nursing home.
Statistical Approach
Taking advantage of the panel nature of the analytic files, we performed multivariate regression analyses employing a facility fixed-effects model (also termed a difference-in-differences model) to examine the effect of introducing state case-mix payment on changes in nursing home case-mix acuity. The fixed-effects control for any fixed facility-specific omitted variables that are correlated with the propensity to care for higher acuity residents. For example, facilities may differ in the presence of assisted living and other potential substitutes for lower acuity nursing home residents in the local market. In addition, we included an indicator for each year of data represented in the analysis, which controls for unobserved national trends in resident acuity due to factors such as demographic changes in the elderly or Medicare policy changes. Thus, this modeling strategy implicitly purges the unobserved and potentially confounded cross-sectional heterogeneity by relying on the within-state variation in case-mix payment over time and by using states that did not change their policies as a control for unrelated time-series variation (Grabowski 2002). The fixed-effects approach is particularly useful for policy analysis and program evaluation (Wooldridge 2002), as is the case in our study.
We carried out the facility fixed-effects model using the XTREG (cross-sectional times-series linear regression) procedure (using the within-panel estimator) available in the latest version (V.9) of the Stata software (StataCorp 2005), which fits regression models to panel data. The dependent variable in the model is the continuous case-mix index score in the natural logged form. Thus, the coefficient estimates can be interpreted as the percent change in resident acuity. In addition, we applied the Huber/White/Sandwich robust variance estimator, combined with clustering on the panel variable (facility), to produce standard errors of the parameter estimates that are robust to cross-sectional heteroskedasticity and within-panel serial correlation (Wooldridge 2002).
STUDY RESULTS
In 1996, the beginning year of our study period, Medicaid nursing home case-mix payment was in place in 26 states. These states include Arizona, Arkansas, Delaware, Illinois, Kansas, Kentucky, Massachusetts, Maryland, Maine, Minnesota, Mississippi, Montana, North Dakota, Nebraska, New Jersey, Nevada, New York, Ohio, Pennsylvania, South Carolina, South Dakota, Texas, Virginia, Vermont, Wisconsin, and West Virginia. Six more states introduced case-mix payment in the 6-year period that followed: Indiana and Washington (effective October 1998 in both states), New Hampshire (February 1999), Colorado (January 2000), Idaho (July 2000), and Iowa (July 2001).
As expected, the mean NCMI score (aggregated over 1999–2002) for new admits (0.95) was considerably higher than that for long-stay residents (0.72), as shown in Table 2. The correlation between the OSCAR-based acuity index and the MDS based RUG-III NCMI score for long-stay residents was moderate (Pearson's=0.60; number not shown in table), and the correlation with the admission NCMI was relatively weak (Pearson's=0.42; number not shown in table). These correlations make intuitive sense in that the resident acuity profile from the annual OSCAR survey should resemble that of long-stay residents more than new admits as there are fewer new admits at a single point in time.
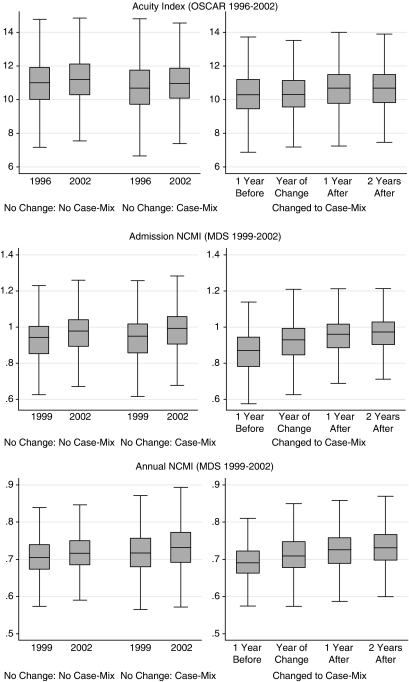
Before turning to the fixed-effects model results, we first graphed the facility averaged acuity levels in box plots, stratified by whether the state introduced a case-mix payment system during the study period (Figure 1). In states that changed to case-mix payment, we present the facility acuity profile in the year preceding the payment change, the year of the change, 1 year postchange and 2 years postchange. There was a clear upward shift in acuity in the year immediately following case-mix introduction (leveling off thereafter) relative to the precase-mix year, regardless of which acuity index was examined. In states that did not experience a policy change, we compared acuity at baseline (i.e., the beginning year) and the final year of our study period, separately in states with and without case-mix payment throughout the period (Figure 1). There was a trend of increasing acuity in these states as well, which reflects the national increase in acuity over our period of study distinct from the implementation of case-mix payment.
Figure 1.
Facility Average Acuity Index Score, by State Case-Mix Policies.
In the multivariate framework, the adoption of state case-mix payment significantly increased nursing home acuity levels over the study period across all of the acuity measures (Table 3). Specifically, the OSCAR-based acuity index increased by 1.3 percent, on average, following the adoption of state case-mix systems. There was a more salient increase in the MDS-based RUG-III NCMI score in response to states' switching to case-mix payment, by 2.5 and 1.4 percent, for admissions and long-stay residents, respectively. These effects were net of the highly significant overall trends of increasing acuity in nursing homes over time, as captured by the calendar year dummy variables.
Table 3.
The Effect of State Case-Mix Payment on Nursing Home Case-Mix Acuity: Facility Fixed-Effects Model Results
| RUG-III NCMI (MDS) | |||
|---|---|---|---|
| Acuity Index (OSCAR) | Admission | Long stay | |
| State policies | |||
| Case-mix payment (1/0) | 0.0133** | 0.0248** | 0.0144** |
| CPI-adjusted Medicaid rate (in 2002 dollars) | 0.0016* | 0.0027** | 0.0044** |
| Percent of Medicaid LTC spending on HCBS | −0.0057** | −0.0022+ | 0.0003 |
| CON for NHs (1/0)† | 0.0083** | — | — |
| Facility characteristics | |||
| For profit (1/0) | −0.0009 | 0.0034 | 0.0016 |
| Chain membership (1/0) | 0.0031 | 0.0055* | 0.0041* |
| Total number of beds | −0.0018** | 0.0021** | −0.0006 |
| Percent of residents paid by Medicare | 0.0023** | 0.0080** | 0.0020** |
| Market (county) characteristics | |||
| Wage index | 0.0085* | 0.0021 | −0.0026 |
| Number of NH beds per 1,000 population 75+ | 0.0000 | −0.0001 | 0.0000 |
| Calendar year‡ | |||
| 1997 | 0.0040** | — | — |
| 1998 | 0.0079** | — | — |
| 1999 | 0.0086** | — | — |
| 2000 | 0.0144** | 0.0090** | 0.0029** |
| 2001 | 0.0188** | 0.0209** | 0.0073** |
| 2002 | 0.0237** | 0.0345** | 0.0130** |
| Intercept | 2.3438** | −0.1112** | −0.3474** |
| R2 (overall) | 0.0015 | 0.1563 | 0.0706 |
| F-test of overall model fit | F(16, 82,457)=26.2 (p > F)=0 | F(12, 41,123)=124.9 (p > F)=0 | F(12, 40,857)=57.2 (p > F)=0 |
RUG-III NCMI, Resource Utilization Group (Version III) based Nursing Case-Mix Index; MDS, Minimum Data Set; OSCAR, On-line Survey Certification and Reporting system; CON, Certificate of Need; NH, nursing home; LTC, long-term care.
CON was excluded from the MDS-based model, because there was no change in this variable between 1999 and 2002, and the fixed-effects model only identifies time-varying covariates. Statistical significance
p < .10
p < .05
p < .01.
The base (reference) year is 1996 in the OSCAR-based model and 1999 in the MDS-based model.
A higher inflation-adjusted Medicaid payment rate (in $10 increment) was associated with higher resident acuity in all three models, although the magnitude of this effect was small. An increase in the percent of state Medicaid LTC spending on HCBS (in 10 percent increment) was associated with lower resident acuity based on the OSCAR measure, but had no significant effect on the RUG-NCMI. Moreover, the OSCAR-based acuity index appeared to be slightly higher in states with the CON program in effect. As expected, facilities with a higher proportion of residents receiving Medicare-financed care (in 10 percent increment) had a greater acuity profile. Although there was no significant difference in acuity levels between for-profit and nonprofit facilities, facilities that were part of a nursing home chain had higher RUG-NCMI scores than stand-alone facilities. In addition, facilities with an increase in bed size (increment of 10 beds) appeared to have higher-acuity levels at admission but somewhat lower acuity levels for the long-stay residents.
DISCUSSION
Our study is the first to examine the relationship between RUG-based resident acuity measures (NCMI) and state case-mix Medicaid payment systems using national longitudinal data repository of MDS assessments and a facility fixed-effects model approach. As such, our study provides the most comprehensive and definitive evidence to date regarding the impact of introducing state case-mix payment on access to nursing home care. Our findings suggest that case-mix adjusted Medicaid payment systems, which have been widely adopted by states in recent years, have increased access to nursing home care for functionally more dependent Medicaid residents.
Specifically, we observed a 2.5 percent increase in the average acuity of residents upon admission (based on RUG-NCMI from MDS) and over 1.3 percent increase in the average acuity of long-stay nursing home residents (based on both OSCAR data and MDS annual assessments), following the introduction of state case-mix payment. On the surface, our range of estimates (1–2.5 percent) would seem to imply a relatively modest effect of case-mix payment on resident acuity. However, two points are worth noting. First, our lower bound estimate of 1 percent was generated using acuity information from the OSCAR system, which is more susceptible to bias given the aggregation of acuity data at the facility level. Second, even if we take the OSCAR-based estimate at face value, a 1 percent increase in acuity implies a considerable increase in the cost of Medicaid dollars. For example, the average RUG-NCMI for the long-stay residents in 2001 was about 0.72. Based on the CMS proposed FY 2004 rates (Centers for Medicare and Medicaid Services 2003), a 1 percent increase above the NCMI of 0.72 would raise the direct care (nursing) component rate by at least 1 percent. Applying a 1 percent increase in the average Medicaid per diem rate in 2002 ($118) would cost an additional $1.18 per resident per day. Assuming an average of 100 residents per facility for roughly 15,000 freestanding facilities nationwide, the total additional cost on Medicaid to cover the extra nursing needs due to increased acuity would amount to nearly $1.8 million per day or $650 million per year. These estimates are based on the direct care (nursing) component of the rate alone, and the actual increase in costs could be even higher if other components of the rate, such as therapy, labor, and other noncase-mix components required by the increased complexity of residents, are factored in. Thus, the financial implications of our findings are substantial.
Given that a primary objective of case-mix payment is to increase access to care, our results suggest that the minority of states without a case-mix system perhaps should consider the adoption of case-mix payment. In fact, our continuous tracking of state policy changes indicates that since our study, at least three additional states have recently adopted a case-mix payment system: Georgia (effective July 2002), Louisiana and Utah (both effective January 2003).
Although the increased access for high acuity cases we observed under case-mix payment is encouraging, a full evaluation of these systems must also consider the potential implications for costs and quality of care. Case-mix payment does not generally make cost containment an explicit objective. In fact, most case-mix systems are designed to be cost increasing with the case-mix adjusted payment offering an antidote to the already strong measures to limit spending on the part of nursing homes under a prospective-based system (Feder and Scanlon 1989). Indeed, most empirical research shows higher direct and indirect care costs following the introduction of case-mix payment due to increased program administration costs and the need for more resources to care for higher-acuity residents (Schlenker 1986; Butler and Schlenker 1989; Arling and Daneman 2002; Swan and Pickard 2003).
This cost issue has not been lost on the nursing home industry. In a recent update to investors, the CEO of a multistate nursing home chain noted the strategy of strengthening the company's Medicaid business base by concentrating operations in states with case-mix payment systems (according to remarks by William R. Floyd, Chairman and Chief Executive Officer, Beverly Enterprises Inc., “Investor Update,” CIBC World Markets Healthcare Conference, New York, NY, November 9, 2004). The CEO noted that the chain's net Medicaid per diem rate averaged more than $8.50 higher in states with case-mix relative to states without such systems. If states with case-mix payment systems offer the opportunity for greater profit margins, ultimately we may expect some shift over time toward greater for-profit and chain market share in these states. The implication for nursing home quality of such a shift is an area for future research.
On the other hand, increases in access to care under case-mix payment for those sickest individuals may also generate some aggregate cost savings by reducing costly hospital days. Individuals who stay at home or in other residential care settings because of access barriers to nursing homes may receive inadequate care, increasing the risk of hospitalization, and hence, costs. From a policy perspective however, any public savings from reduced hospitalizations under Medicaid case-mix payment will generally accrue to the federal Medicare program. The interdependence of Medicare and Medicaid thus emerges as an important issue for state and federal policymakers to consider.
Improvement of quality is often cited as an objective in implementing case-mix payment (Butler and Schlenker 1989; Feder and Scanlon 1989), but most studies have found that although resident acuity increases under case-mix payment, staffing does not increase commensurately (Cohen and Dubay 1990; Grabowski 2002). Yet, numerous studies have documented the link between inadequate staffing levels and increased frequency of deficiencies and other quality of care problems (Institute of Medicine 1996; Harrington et al. 2000; Kayser-Jones et al. 2003; Office of Inspector General 1999; Schnelle 2004; Schnelle et al. 2004). The issue of limited staffing is likely to be exacerbated by a looming crisis of nurse shortages in the years ahead (General Accounting Office 2001). As the medical and functional care needs of nursing home residents become increasingly complex, a genuine concern emerges about the ability of nursing homes to care for higher-acuity residents. In this context, addressing the implications of case-mix reimbursement for quality becomes ever more important. Nevertheless, the limited evidence to date is quite mixed in regards to process and outcome based measures of quality (Schlenker et al. 1988; Butler and Schlenker 1989; Feder and Scanlon 1989; Grabowski 2002).
Ultimately, it remains unclear whether case-mix payment policies are cost-effective for state Medicaid programs. Ideally, a system could provide incentives for both better access and improved quality. One idea that has recently gained some steam in the Medicare program is the “pay for performance” concept. In the hospital setting, there is an ongoing Medicare sponsored demonstration to evaluate the effectiveness of such a system, and plans for a nursing home demonstration are currently underway. Both Sen. Ron Wyden (D-Ore.) and Rep. Phil English (R.-Pa.) recently introduced legislation that would reward nursing homes providing high quality care and penalize low quality providers. Under the proposed legislation, the top 10 percent of nursing homes would receive a bonus of 2 percent on top of their annual Medicare payment update while the top 20 percent would receive a 1 percent boost. Nursing homes that fall below a set of quality benchmarks would lose one percentage point of their annual Medicare update.
Unfortunately, there is little empirical work evaluating this payment method for chronic nursing home care. One notable exception was a controlled experiment in San Diego, which found that the use of monetary incentives had beneficial effects on the health of nursing home residents. Moreover, nursing homes in the experimental group admitted individuals with more severe disabilities and the average length-of-stay was shortened (Norton 1992). Although the cost of developing and administering such a payment system may be considerable, earmarking payments for better outcomes might be an innovative means of balancing access, quality and costs within a Medicaid payment system. However, such a system has the potential to further widen the gap between the haves and have-nots in the nursing home sector (Mor et al. 2004).
The acuity of nursing home residents is likely to be more severe in the years to come, as assisted living and other forms of home- and community-based care continue to deflect admission of lower acuity nursing home residents. In light of this trend, the implications of state Medicaid payment policy for access, costs, and quality of care for those most dependent residents will be particularly important.
Acknowledgments
This research was supported by the National Institute on Aging Grant R37 AG11624 and R01 AG20557 (PI: Vincent Mor), and data were analyzed under Data Use Agreement No. 12434. We appreciate the assistance of Jeff Hiris in the presentation of the data, and insightful comments by Jacqueline Zinn, Susan Miller, and Mark Schleinitz on earlier drafts of this paper.
References
- Arling G, Daneman B. Nursing Home Case-Mix Reimbursement in Mississippi and South Dakota. Health Services Research. 2002;37(2):377–95. doi: 10.1111/1475-6773.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop C E. Where Are the Missing Elders? The Decline in Nursing Home Use, 1985 and 1995. Health Affairs (Millwood) 1999;18(4):146–55. doi: 10.1377/hlthaff.18.4.146. [DOI] [PubMed] [Google Scholar]
- Burwell B, Sredl K, Eiken S. Medicaid Long Term Care Expenditures in FY 2004. [March 20, 2006];2005 Medstat. Available at http://www.hcbs.org/moreInfo.php/topic/207/sby/Author/lim/ALL/doc/1260/Medicaid_Long_Term_Care_Expenditures_in_FY_2004.
- Butler P A, Schlenker R E. Case-Mix Reimbursement for Nursing Homes: Objectives and Achievements. Milbank Quarterly. 1989;67(1):103–36. [PubMed] [Google Scholar]
- Carter G M, Newhouse J P, Relles D A. How Much Change in the Case Mix Index Is DRG Creep? Journal of Health Economics. 1990;9(4):411–28. doi: 10.1016/0167-6296(90)90003-l. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. Medicare Program; Prospective Payment System and Consolidated Billing for Skilled Nursing Facilities-Update; Proposed Rule. Federal Register. 2003;68(95):26757–83. [PubMed] [Google Scholar]
- Chulis G S. Assessing Medicare's Prospective Payment System for Hospitals. Medical Care Research and Review. 1991;48(2):167–206. doi: 10.1177/002570879104800203. [DOI] [PubMed] [Google Scholar]
- Cohen J W, Dubay L C. The Effects of Medicaid Reimbursement Method and Ownership on Nursing Home Costs, Case Mix, and Staffing. Inquiry. 1990;27(2):183–200. [PubMed] [Google Scholar]
- Cowles C M. Nursing Home Statistical Yearbook (2002) Montgomery Village, MD: Cowles Research Group; 2002. [Google Scholar]
- Dugan J K. Federal Government Expands Compliance Initiatives. Healthcare Financial Management. 1997;51(9):54–8. [PubMed] [Google Scholar]
- Ettner S L. Do Elderly Medicaid Patients Experience Reduced Access to Nursing Home Care? Journal of Health Economics. 1993;12(3):259–80. doi: 10.1016/0167-6296(93)90011-3. [DOI] [PubMed] [Google Scholar]
- Feder J, Scanlon W. Regulating the Bed Supply in Nursing Homes. Milbank Quarterly. 1980;58(1):54–88. [PubMed] [Google Scholar]
- Feder J, Scanlon W. Case-Mix Payment for Nursing Home Care: Lessons from Maryland. Journal of Health Politics, Policy, and Law. 1989;14(3):523–47. doi: 10.1215/03616878-14-3-523. [DOI] [PubMed] [Google Scholar]
- Friedman B. Economic Aspects of the Rationing of Nursing Home Beds. Journal of Human Resources. 1982;17(1):59–71. [PubMed] [Google Scholar]
- Fries B E. Comparing Case-Mix Systems for Nursing Home Payment. Health Care Financing Review. 1990;11(4):103–19. [PMC free article] [PubMed] [Google Scholar]
- Fries B E, Schneider D P, Foley W J, Gavazzi M, Burke R, Cornelius E. Refining a Case-Mix Measure for Nursing Homes: Resource Utilization Groups (RUG-III) Medical Care. 1994;32(7):668–85. doi: 10.1097/00005650-199407000-00002. [DOI] [PubMed] [Google Scholar]
- General Accounting Office. Nursing Workforce: Emerging Nurse Shortages Due to Multiple Factors. Washington, DC: General Accounting Office; 2001. [Google Scholar]
- Gibson M J, Gregory S R, Houser A N, Fox-Grade W. Across the States: Profiles of Long-Term Care. 6. Washington, DC: AARP Public Policy Institute; 2004. [Google Scholar]
- Grabowski D C. The Economic Implications of Case-Mix Medicaid Reimbursement for Nursing Home Care. Inquiry. 2002;39(3):258–78. doi: 10.5034/inquiryjrnl_39.3.258. [DOI] [PubMed] [Google Scholar]
- Grabowski D C, Angelelli J J, Mor V. Medicaid Payment and Risk-Adjusted Nursing Home Quality Measures. Health Affairs. 2004;23(5):243–52. doi: 10.1377/hlthaff.23.5.243. [DOI] [PubMed] [Google Scholar]
- Grabowski D C, Feng Z, Intrator O, Mor V. Recent Trends in State Nursing Home Payment Policies. Health Affairs. 2004 doi: 10.1377/hlthaff.w4.363. Web Exclusives (June 16): W4-363-373. [DOI] [PubMed] [Google Scholar]
- Greenless J S, Marshall J M, Yett D E. Nursing Home Admissions Policies under Reimbursement. Bell Journal of Economics. 1982;13(1):93–106. [Google Scholar]
- Gruenberg L W, Willemain T R. Hospital Discharge Queues in Massachusetts. Medical Care. 1982;20(2):188–201. doi: 10.1097/00005650-198202000-00006. [DOI] [PubMed] [Google Scholar]
- Harrington C, Swan J H, Wellin V, Clemena W, Carrillo H M. 1998 State Data Book on Long Term Care Program and Market Characteristics. San Francisco: Department of Social & Behavioral Sciences, University of California; 1999. [Google Scholar]
- Harrington C, Zimmerman D, Karon S L, Robinson J, Beutel P. Nursing Home Staffing and Its Relationship to Deficiencies. Journal of Gerontology. 2000;55(5):S278–87. doi: 10.1093/geronb/55.5.s278. [DOI] [PubMed] [Google Scholar]
- Holahan J, Cohen J. Nursing Home Reimbursement: Implications for Cost Containment, Access, and Quality. Milbank Quarterly. 1987;65(1):112–47. [PubMed] [Google Scholar]
- Hsia D C, Ahern C A, Ritchie B P, Moscoe L M, Krushat W M. Medicare Reimbursement Accuracy under the Prospective Payment System, 1985 to 1988. Journal of the American Medical Association. 1992;268(7):896–9. [PubMed] [Google Scholar]
- Hsia D C, Krushat W M, Fagan A B, Tebbutt J A, Kusserow R P. Accuracy of Diagnostic Coding for Medicare Patients under the Prospective-Payment System. New England Journal of Medicine. 1988;318(6):352–5. doi: 10.1056/NEJM198802113180604. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Nursing Staff in Hospitals and Nursing Homes: Is It Adequate? Washington, DC: National Academy Press; 1996. pp. 128–68. [Google Scholar]
- Kayser-Jones J, Schell E, Lyons W, Kris A E, Chan J, Beard R L. Factors That Influence End-of-Life Care in Nursing Homes: The Physical Environment, Inadequate Staffing, and Lack of Supervision. Gerontologist. 2003;43:76–84. doi: 10.1093/geront/43.suppl_2.76. Spec No 2. [DOI] [PubMed] [Google Scholar]
- Konetzka R T, Yi D, Norton E C, Kilpatrick K E. Effects of Medicare Payment Changes on Nursing Home Staffing and Deficiencies. Health Services Research. 2004;39(3):463–88. doi: 10.1111/j.1475-6773.2004.00240.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor V. A Comprehensive Clinical Assessment Tool to Inform Policy and Practice: Applications of the Minimum Data Set. Medical Care. 2004;42(4 Suppl):III50–9. doi: 10.1097/01.mlr.0000120104.01232.5e. [DOI] [PubMed] [Google Scholar]
- Mor V, Zinn J, Angelelli J, Teno J M, Miller S C. Driven to Tiers: Socioeconomic and Racial Disparities in the Quality of Nursing Home Care. Milbank Quarterly. 2004;82(2):227–56. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukamel D B, Spector W D. The Competitive Nature of the Nursing Home Industry: Price Mark Ups and Demand Elasticities. Applied Economics. 2002;34(4):413–20. [Google Scholar]
- Murtaugh C M, Cooney L M, Der Simonian R R, Smits H L, Fetter R B. Nursing Home Reimbursement and the Allocation of Rehabilitation Therapy Resources. Health Services Research. 1988;23(4):467–93. [PMC free article] [PubMed] [Google Scholar]
- Norton E C. Incentive Regulation of Nursing Homes. Journal of Health Economics. 1992;11(2):105–28. doi: 10.1016/0167-6296(92)90030-5. [DOI] [PubMed] [Google Scholar]
- Norton E C. Long-Term Care. In: Cuyler A J, Newhouse J P, editors. Handbook of Health Economics. Amsterdam: Elsevier Science; 2000. pp. 955–94. [Google Scholar]
- Nyman J A. The Marginal Cost of Nursing Home Care, New York, 1983. Journal of Health Economics. 1988;7(4):393–412. doi: 10.1016/0167-6296(88)90022-7. [DOI] [PubMed] [Google Scholar]
- Office of the Inspector General. Quality of Care in Nursing Homes: An Overview. Washington, DC: U.S. Department of Health and Human Services; 1999. [Google Scholar]
- Office of the Inspector General. Nursing Home Resident Assessment Quality of Care. Washington, DC: Office of the Inspector General; 2001. [Google Scholar]
- Reid W M, Coburn A F. Managerial Responses to Medicaid Prospective Payment in the Nursing Home Sector. Hospital and Health Services Administration. 1996;41(3):283–96. [PubMed] [Google Scholar]
- Reschovsky J D. Demand for and Access to Institutional Long-Term Care: The Role of Medicaid in Nursing Home Markets. Inquiry. 1996;33(1):15–29. [PubMed] [Google Scholar]
- Schlenker R E. Case Mix Reimbursement for Nursing Homes. Journal of Health Politics, Policy, and Law. 1986;11(3):445–61. doi: 10.1215/03616878-11-3-445. [DOI] [PubMed] [Google Scholar]
- Schlenker R E. Nursing Home Costs, Medicaid Rates, and Profits under Alternative Medicaid Payment Systems. Health Services Research. 1991;26(5):623–49. [PMC free article] [PubMed] [Google Scholar]
- Schnelle J F. Determining the Relationship between Staffing and Quality. Gerontologist. 2004;44(1):10–2. doi: 10.1093/geront/44.1.10. [DOI] [PubMed] [Google Scholar]
- Schnelle J F, Simmons S F, Harrington C, Cadogan M, Garcia E, Bates-Jensen B M. Relationship of Nursing Home Staffing to Quality of Care. Health Services Research. 2004;39(2):225–50. doi: 10.1111/j.1475-6773.2004.00225.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro E, Roos N P, Kavanagh S. Long Term Patients in Acute Care Beds: Is There a Cure? Gerontologist. 1980;20(3 Part 1):342–9. doi: 10.1093/geront/20.3_part_1.342. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 9. College Station, TX: StataCorp LP; 2005. pp. 244–65. [Google Scholar]
- Steinwald B, Dummit L A. Hospital Case-Mix Change: Sicker Patients or DRG Creep? Health Affair (Millwood) 1989;8(2):35–47. doi: 10.1377/hlthaff.8.2.35. [DOI] [PubMed] [Google Scholar]
- Strahan G W. An Overview of Nursing Homes and Their Current Residents: Data from the 1995 National Nursing Home Survey. Advance Data. 1997;(280):1–12. [PubMed] [Google Scholar]
- Swan J H, Harrington C, Clemena W, Pickard R B, Studer L, de Wit S K. Medicaid Nursing Facility Reimbursement Methods: 1979–1997. Medical Care Research and Review. 2000;57(3):361–78. doi: 10.1177/107755870005700306. [DOI] [PubMed] [Google Scholar]
- Swan J H, Pickard R B. Medicaid Case-Mix Nursing Home Reimbursement in Three States. Journal of Health and Social Policy. 2003;16(4):27–53. doi: 10.1300/J045v16n04_02. [DOI] [PubMed] [Google Scholar]
- Thorpe K E, Gertler P J, Goldman P. The Resource Utilization Group System: Its Effect on Nursing Home Case Mix and Costs. Inquiry. 1991;28(4):357–65. [PubMed] [Google Scholar]
- Troyer J L. Cross-Subsidization in Nursing Homes: Explaining Rate Differentials among Payer Types. Southern Economic Journal. 2002;68(4):750–73. [Google Scholar]
- U.S. General Accounting Office. Nursing Homes: Admission Problems for Medicaid Recipients and Attempts to Solve Them. Washington, DC: U.S. General Accounting Office; 1990. [Google Scholar]
- Weissert W G, Cready C M. Determinants of Hospital-to-Nursing Home Placement Delays: A Pilot Study. Health Services Research. 1988;23(5):619–47. [PMC free article] [PubMed] [Google Scholar]
- Wooldridge J M. Econometric Analysis of Cross Section and Panel Data. Cambridge, MA: MIT Press; 2002. pp. 247–91. [Google Scholar]
- Zhang X, Grabowski D C. Nursing Home Staffing and Quality under the Nursing Home Reform Act. Gerontologist. 2004;44(1):13–23. doi: 10.1093/geront/44.1.13. [DOI] [PubMed] [Google Scholar]
- Zimmerman D R, Karon S L, Arling G, Clark B R, Collins T, Ross R, Sainfort F. Development and Testing of Nursing Home Quality Indicators. Health Care Financing Review. 1995;16(4):107–27. [PMC free article] [PubMed] [Google Scholar]
- Zinn J S, Mor V, Intrator O, Feng Z, Angelelli J, Davis J A. The Impact of the Prospective Payment System for Skilled Nursing Facilities on Therapy Service Provision: A Transaction Cost Approach. Health Services Research. 2003;38(6, part 1):1467–85. doi: 10.1111/j.1475-6773.2003.00188.x. [DOI] [PMC free article] [PubMed] [Google Scholar]