Abstract
The VP35 protein of Ebola virus is a viral antagonist of interferon. It acts to block virus or double-stranded RNA-mediated activation of interferon regulatory factor 3, a transcription factor that facilitates the expression of interferon and interferon-stimulated genes. In this report, we show that the VP35 protein is also able to inhibit the antiviral response induced by alpha interferon. This depends on the VP35 function that interferes with the pathway regulated by double-stranded RNA-dependent protein kinase PKR. When expressed in a heterologous system, the VP35 protein enhanced viral polypeptide synthesis and growth in Vero cells pretreated with alpha/beta interferon, displaying an interferon-resistant phenotype. In correlation, phosphorylation of PKR and eIF-2α was suppressed in cells expressing the VP35 protein. This activity of the VP35 protein was required for efficient viral replication in PKR+/+ but not PKR−/− mouse embryo fibroblasts. Furthermore, VP35 appears to be a RNA binding protein. Notably, a deletion of amino acids 1 to 200, but not R312A substitution in the RNA binding motif, abolished the ability of the VP35 protein to confer viral resistance to interferon. However, the R312A substitution rendered the VP35 protein unable to inhibit the induction of the beta interferon promoter mediated by virus infection. Together, these results show that the VP35 protein targets multiple pathways of the interferon system.
Interferons are a family of cytokines that are produced in response to viral infection. They exert antiviral, cell growth-inhibitory, and immunoregulatory activities (42, 43). Expression of interferons is regulated through coordinated activation of transcription factors, including NF-κB, AP-1, interferon regulatory factor 3 (IRF-3), and IRF-7. Once bound to their cognate receptors, interferons activate the Janus tyrosine kinase (JAK)/signal transducer and activator (STAT) pathways, which lead to the induction of a wide spectrum of genes. Among these genes are the extensively characterized genes encoding 2′-5′ oligoadenylate synthetase, the Mx proteins, and the double-stranded RNA (dsRNA)-dependent protein kinase (PKR). In normal cells, PKR is present at a low level, but its expression is upregulated by interferon. Upon binding to dsRNA, PKR is activated to phosphorylate the α subunit of translation initiation factor eIF-2 (eIF-2α), which arrests protein synthesis and thereby inhibits viral replication.
Several lines of evidence indicate that Ebola virus infection interferes with host interferon responses. When endothelial cells are treated with alpha interferon, gamma interferon, or dsRNA, elevated mRNA levels of interferon-stimulated genes, such as major histocompatibility complex class I, IRF-1, PKR, and 2′-5′ oligoadenylate synthetase, are seen in mock-infected cells but not in Ebola virus-infected cells (21, 23, 24). Additionally, Ebola virus infection efficiently blocks dsRNA-mediated interferon production in macrophages, peripheral blood mononuclear cells, and dendritic cells (6, 22, 34). Accordingly, Ebola virus infection blocks maturation of dendritic cells, which impairs T-cell activation and proliferation (6, 34). Consistent with these observations, mice lacking alpha/beta interferon receptor or STAT1 resemble primates in their susceptibility to rapidly progressive, overwhelming Ebola virus infection (7). The disease is dramatically accelerated when viral challenge is accompanied by an injection of anti-alpha/beta interferon antibodies (7). Of particular interest is that Ebola virus replication is insensitive to interferon both in vivo and in cell culture (24, 30, 32).
Ebola virus, a nonsegmented negative-stranded RNA virus, belongs to the family of Filoviridae (46). The viral genome is approximately 19,000 nucleotides in length and is transcribed into eight major subgenomic mRNAs, which encode seven structural proteins (NP, VP35, VP40, GP, VP30, VP24, and L) and one nonstructural protein (sGP). The VP35 protein is an essential cofactor for the viral RNA polymerase complex (28, 35, 49). In addition, it is implicated as an interferon antagonist (3, 6). It has been demonstrated that the VP35 protein complements the growth defect of an influenza virus NS1 deletion mutant that is unable to block the interferon response (3). In mammalian cells, the VP35 protein suppresses the expression of alpha/beta interferon induced by dsRNA or virus. In doing so, it prevents the activation of IRF-3 (2). It appears the carboxyl terminus of the VP35 contains sequences sufficient to inhibit virus-induced interferon responses, whereas the amino terminus involved in oligomerization is required for its full activity (25, 40). Currently, the precise role of the Ebola virus VP35 protein is not fully understood yet.
The present study was undertaken to further explore the function of the VP35 protein in interferon responses. We report that in addition to inhibition of interferon induction by virus, the VP35 protein counteracts the antiviral effect of alpha/beta interferon mediated by PKR. We show that the VP35 protein is a RNA binding protein with a stronger affinity for dsRNA. We further demonstrate that a deletion in the amino terminus is lethal for its anti-PKR activity, whereas the R312A substitution in the RNA binding motif has no effect. Intriguingly, the R312A substitution disrupted the activity of VP35 required to inhibit induction of the beta interferon promoter by virus infection. Thus, the VP35 protein of Ebola virus interferes with multiple pathways in the interferon system. During the course of this work, Cardenas and colleagues reported that Ebola virus VP35 binds double-stranded RNA and inhibits alpha/beta interferon production by RIG-I signaling (8).
MATERIALS AND METHODS
Cells and viruses.
Vero and 293T cells were obtained from the American Type Culture Collection. Mouse embryo fibroblasts were derived from PKR+/+ and PKR−/− mice (16). Cells were propagated in Dulbecco's modified Eagle's medium supplemented with 5% or 10% fetal bovine serum. The following viruses were constructed using the bacterial artificial chromosome (BAC) system as described previously (27). Recombinant virus HSV-BAC contains the wild-type herpes simplex virus type 1 (HSV-1) strain F genome. KY0234 is a recombinant virus that lacks both copies of the γ134.5 gene (12). Recombinant virus MC0201 has both copies of the γ134.5 gene of HSV-BAC replaced with the wild-type Ebola virus subtype Zaire VP35 gene. MC0309 is a recombinant virus in which the VP35 gene of MC0201 is replaced with the wild-type γ134.5 gene. MC0301 is a recombinant virus in which the VP35 gene of MC0201 is replaced with a γ134.5 gene that contains an R215L mutation. To construct recombinant virus MC0201, plasmid pMC0201 was transformed into an Escherichia coli RR1 strain that harbored wild-type HSV-BAC by electroporation. After 2 h at 30°C in LB broth, the bacteria were plated onto plates containing zeocin and chloramphenicol (Cm) and incubated overnight at 43°C. Colonies were selected and diluted serially in LB, plated on Cm-5% sucrose (Suc) LB plates, and incubated overnight at 30°C. In a similar manner, recombinant viruses MC0309 and MC0301 were constructed by transformation of an E. coli RR1 strain that harbored MC0201 DNA by electroporation with plasmids pKY0230 and pMC0020, respectively. The recombinant HSV-BAC DNA was prepared and used to transfect Vero cells using Lipofectamine reagent (Invitrogen). Virus was harvested 3 days after transfection. Preparation of viral stocks and viral infection were carried out in accordance with all federal and university policies.
Plasmids.
Plasmid pcdna3-EBO-35 contains the VP35 gene of the Ebola virus strain Mayinga, subtype Zaire, inserted into the expression vector pcDNA3 (3). To construct pMC0201, the BamHI-NotI Klenow fragment containing the VP35 gene of pcdna3-EBO-35 was ligated into the BamHI and EcoRV sites of pKY0140 (31). In this plasmid, expression of VP35 is driven by a cytomegalovirus promoter. To construct pKY0230, the BamHI fragment of HSV-1(F) of pRB143 was cloned into the BamHI site of the pKO5Y vector. Plasmid pRB143 contains the BamHI S fragment of HSV-1(F) in the BamHI site of pRB322. To construct pMC0020, a PCR fragment was amplified with primers OBH0008 (CGCCCGCCTGGCGCTCCGCGGCTCGTGGGCC) and OBH0020 (TATATGCGCGGCTCCTGCCATCGTC), and a second PCR fragment was amplified with primers OBH0018 (CCACCCCGGCACGCTCTCTGTCTC) and OBH0009 (GGCCCACGAGCCGCGGAGCGCCAGGCGGGCG). The resulting PCR products were used as templates, and a DraIII-BspEI PCR fragment was amplified with primers OBH0018 and OBH0020 to yield pMC0005. To construct pMC0015, the DraIII-StuI fragment of pMC0005 was used to replace the corresponding region in the entire BamHI S fragment of HSV-1(F). The BamHI S fragment of pMC0015 was then cloned into the BamHI site of pKO5Y, yielding pMC0020. A modified retroviral vector expressing green fluorescent protein (GFP), HIV-GFP, was obtained from Thomas Hope. To construct pZF0601 (pVP35wt), a PCR fragment containing the wild-type VP35 gene was cloned into the BamHI and XhoI sites of human immunodeficiency virus (HIV) vector. To construct pZF0602 (pVP35R312A), a PCR fragment containing the VP35 gene with a R312A substitution was cloned into the BamHI and XhoI sites of HIV vector. To construct pZF0603 (pVP35dN200FLAG), a PCR fragment encoding amino acids 201 to 340 with a FLAG tag at the C terminus was cloned into the BamHI and XhoI sites of HIV vector. To construct pZF0417 (pVP35FLAG), a PCR fragment containing wild-type VP35 with a FLAG tag at the C terminus was cloned into pcDNA3. To construct pZF0422 (pVP35R312A), a PCR fragment containing the R312A substitution in VP35 with a FLAG tag at the C terminus was cloned into pcDNA3. All plasmid constructs were verified by DNA sequence analysis.
Southern blot analysis.
Vero cells were infected with viruses at 10 PFU per cell. At 18 h postinfection, infected cells were harvested, and viral DNA was prepared as described previously (15). VP35 and γ134.5 viral DNAs were verified by digestion with restriction enzymes, electrophoretic separation in agarose gels, transfer to nitrocellulose sheets, and hybridization with a 32P-labeled EcoRI-XhoI or NotI fragment from the VP35 or γ134.5 gene, respectively, followed by autoradiography as described previously (15).
Immunoblot analysis.
Mock-infected and virus-infected cells were rinsed, harvested, and solubilized in disruption buffer containing 50 mM Tris-HCl (pH 7.0), 5% 2-mercaptoethanol, 2% sodium dodecyl sulfate, and 2.75% sucrose. Samples were then sonicated, boiled, subjected to electrophoresis on denaturing 12% polyacrylamide gels, transferred to nitrocellulose membranes, blocked with 5% nonfat milk, and reacted with anti-γ134.5 antibody, anti-VP35 antibody, anti-HSV-1 antibody (Dako Corporation), anti-phosphorylated eIF-2α antibody (Biosource, Inc.), anti-eIF-2α antibody (Cell Signaling Technology, Inc.), anti-phosphorylated PKR (Cell Signaling Technology, Inc.), anti-PKR antibody (Santa Cruz), or anti-β-actin antibody (Sigma). The membranes were rinsed in phosphate-buffered saline and reacted with either goat anti-rabbit or goat anti-mouse antibody conjugated to horseradish peroxidase (Amersham Pharmacia Biotech, Inc.). Rabbit polyclonal antibody to VP35 was prepared as follows. Plasmid pMC0307 encodes glutathione S-transferase fused in frame to the truncated VP35 gene encoding 187 amino acids of the amino-terminal portion of VP35. Expression of the fusion protein was induced by the addition of isopropyl-β-d-thiogalactopyranoside (IPTG) to the medium with Escherichia coli BL21 cells transformed with pMC0307, followed by affinity purification of the fusion protein from bacterial lysates on agarose beads conjugated with glutathione. The fusion protein was lyophilized and used for immunization of rabbits for production of polyclonal antibody.
Plaque assays.
Cells were either untreated or pretreated with alpha interferon (1,000 U/ml) for 20 h and then infected with the recombinant viruses at 0.05 PFU per cell at 37°C. At different time points postinfection, cells were harvested, freeze-thawed three times, and titrated on Vero cells at 37°C.
Retroviral transduction.
Recombinant retroviruses were generated as described previously (36). Briefly, plasmid pFZ0601, pFZ0602, pZF0603, or HIV-GFP was transfected along with HIVtrans and vesicular stomatitis virus G into 293T cells using Lipofectamine 2000 (Invitrogen). At 48 h after transfection, supernatant was collected and used to transduce cells.
Reporter assays.
Reporter assays were carried out as described previously (2, 25). 293T cells grown on a 12-well plate were transfected with a control plasmid or plasmid vector expressing wild-type VP35 or VP35(R312A) or VP35(dN200) along with a beta interferon reporter gene expressing firefly luciferase using Lipofectamine 2000 (Invitrogen). For a control, a plasmid containing the Renilla luciferase gene driven by the HSV-1 thymidine kinase promoter was included. At 24 h after transfection, cells were infected with Sendai virus (Cantell), and luciferase activities were measured 24 h postinfection. The relative change in induction was determined by comparing plasmids expressing VP35 variants to the vector control.
RNA binding assays.
The RNA binding assay was performed as described previously (45). Briefly, poly(C)-conjugated agarose beads were purchased from Sigma. Poly(I · C)-conjugated beads were prepared by incubating poly(C) beads with poly(I) (Sigma) at 4°C overnight. Cyanogen bromide-activated agarose beads were used as controls. For pull-down assays, poly(C), poly(I · C)-conjugated beads, or empty beads were equilibrated in binding buffer containing 50 mM Tris (pH 7.5), 150 mM NaCl, 1 mM EDTA, and 1% NP-40. The beads were mixed with whole-cell extracts, which were supplemented with protease inhibitor cocktails (Sigma) and RNase inhibitor (Invitrogen), and rotated at 4°C overnight. After centrifugation, beads were washed extensively and then resuspended in sample buffer (9). Samples were incubated at 95°C for 5 min, centrifuged at 13,000 × g for 30s, separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis, and processed for immunoblot analysis.
RESULTS
Experimental design.
Reverse genetic methods have been established for constructing Ebola virus (37, 49). Nonetheless, it remains difficult to study the VP35 protein in interferon responses without altering its function essential for viral RNA replication. To bypass this limitation, we sought to develop a surrogate system, which is based on the finding that wild-type herpes simplex virus type 1 is resistant to interferon, whereas the mutant lacking the γ134.5 gene is hypersensitive to alpha/beta interferon (10). The γ134.5 gene product encodes a multifunctional protein, which is absolutely required for viral replication in vivo (13). In cell culture, the γ134.5 null mutant replicates in Vero cells that are devoid of alpha/beta interferon genes but not in cells with intact interferon genes (10, 11, 14). Thus, growth of the γ134.5 null mutant was utilized as an indicator to assess viral interferon antagonists. In an initial approach, we recombined the VP35 gene into the HSV genome lacking the γ134.5 gene. As an additional measure, we deleted the thymidine kinase gene, which is crucial for viral replication in vivo. This deletion does not affect viral infection or viral response to interferon in cell culture (9). Consequently, these modifications restrict viral replication to a limited number of cell lines, where viral response to interferon was analyzed. On the basis of the above analysis, we also developed a complement approach, in which the VP35 protein was provided in trans by a retrovirus vector in transduced cells, where growth of the γ134.5 null mutant was measured in response to interferon treatment.
Construction of recombinant viruses.
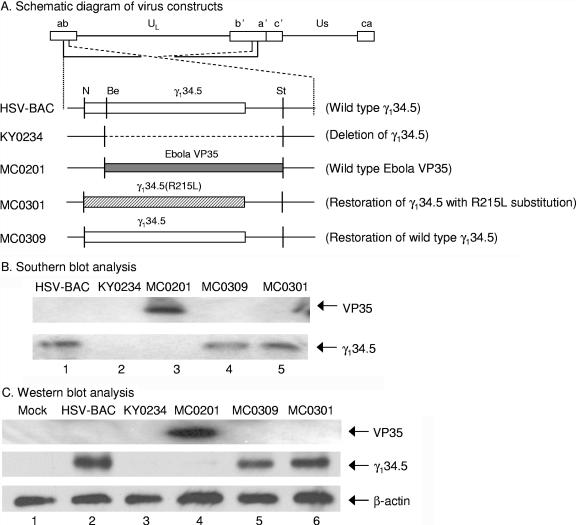
Recombinant viruses were constructed by using the bacterial artificial chromosome system as described in Materials and Methods. In this system, the thymidine kinase gene of HSV was replaced with BAC. As shown in Fig. 1A, in recombinant virus MC0201, the γ134.5 gene of HSV was replaced with the VP35 gene of Ebola virus subtype Zaire. As controls, two additional viruses were constructed. In recombinant virus MC0301, the VP35 gene of MC0201 was replaced with a mutant γ134.5 gene that contains an R215L point mutation that renders the virus sensitive to interferon (9). In MC0309, the VP35 gene of MC0201 was replaced with the wild-type γ134.5 gene. In recombinant virus KY0234, the γ134.5 gene of HSV was deleted (12). Southern blot analysis was carried out to verify virus constructs (Fig. 1B). As expected, MC0201 yielded a 785-bp fragment after digestion with EcoRI-XhoI (Fig. 1B, lane 3). HSV-BAC, MC0309, and MC0301 yielded an 822-bp fragment after digestion with NotI (lanes 1, 4, and 5). No band was detected for KY0234 due to deletion of the γ134.5 gene. To examine protein expression, Western blot analysis was performed using antibodies against the VP35 protein, the γ134.5 protein, and β-actin. The results in Fig. 1C show that in virus-infected cells, MC0201 expressed the VP35 protein (lane 4). MC0309 and MC0301 expressed comparable levels of the γ134.5 protein. HSV-BAC expressed a slightly higher level of the γ134.5 protein (lanes 2, 5, and 6). Expression of the γ134.5 protein was not detected in KY0234 by the anti-γ134.5 antibody. Levels of β-actin expression were comparable in mock-infected and virus-infected cells. These experiments indicate that the recombinant viruses constructed contain the expected VP35 and γ134.5 gene products.
FIG. 1.
(A) Schematic representation of the genome structure of HSV-1 and the recombinant viruses. The two covalently linked components of HSV DNA, L and S, each consist of unique sequences, UL and US, respectively, flanked by inverted repeats which are designated ab and b'a'. Recombinant virus HSV-BAC contains the wild-type γ134.5 gene. Recombinant virus KY0234 lacks the coding region of the γ134.5 gene (12). Recombinant virus MC0201 was constructed by the HSV-BAC system with the VP35 gene from Ebola virus subtype Zaire replacing both copies of the γ134.5 gene. Recombinant viruses MC0309 and MC0301 are repair viruses in which the VP35 gene of MC0201 was replaced with the wild-type γ134.5 gene and a γ134.5 gene containing an R215L point mutation, respectively. Restriction endonuclease abbreviations: N, NcoI; Be, BstEII; St, StuI; E, EcoRV. (B) Autoradiographic images of viral DNAs. Vero cells were infected with the indicated viruses at 10 PFU per cell. At 18 h after infection, cells were harvested and viral DNAs were prepared for Southern blot analysis as described in Materials and Methods. The VP35 and γ134.5 genes were then detected by hybridization to electrophoretically separated digestion products of viral DNA transferred to a nitrocellulose sheet with either a 32P-labeled EcoRI-XhoI or NotI fragment from the VP35 or γ134.5 gene, respectively. Fragments representing VP35 or γ134.5 are indicated on the right. (C) Expression of the VP35 or γ134.5 gene products. Vero cells were either mock infected or infected with the indicated viruses at 10 PFU per cell. At 18 h postinfection, lysates of cells were prepared and subjected to Western immunoblot analysis with either anti-VP35, anti-γ134.5, or anti-β-actin antibody. The positions of the VP35, γ134.5, and β-actin proteins are shown on the right.
The VP35 protein counteracts the antiviral response induced by alpha interferon.
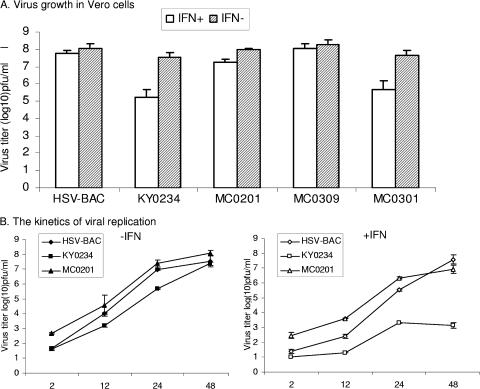
To test whether the VP35 protein blocks the antiviral response induced by interferon, we measured viral replication in untreated Vero cells or Vero cells pretreated with alpha interferon. As summarized in Fig. 2A, in the absence of interferon, recombinant virus HSV-BAC (wild-type γ134.5) reached a virus titer of 1.2 × 108 PFU/ml, and recombinant virus KY0234 (Δγ134.5) reached a virus titer of 3.5 × 107 PFU/ml, which was slightly lower. Replication of recombinant virus MC0201 (wild-type VP35) and recombinant virus MC0309 (restoration of wild-type γ134.5) is similar to that of HSV-BAC, while MC0301 (restoration of γ134.5 with R215L substitution) exhibited a growth property similar to that of KY0234. When cells were pretreated with interferon prior to infection, HSV-BAC reached a virus titer of 5.8 × 107 PFU/ml, while KY0234 showed a significant decrease in viral replication, with a virus titer of 1.7 × 105 PFU/ml. Remarkably, MC0201 displayed efficient viral replication similar to HSV-BAC, reaching a virus titer of 1.8 × 107 PFU/ml. Recombinant virus MC0309 had a virus titer similar to that of HSV-BAC, as this virus has the restored wild-type γ134.5 gene. MC0301 exhibited a growth defect similar to that of KY0234 in the presence of interferon due to the R215L substitution in the γ134.5 gene, which renders this virus sensitive to interferon (9). Moreover, addition of alpha interferon during infection did not affect growth of MC0201 in cells pretreated with alpha interferon or not treated with alpha interferon (data not shown). Thus, the ability of MC0201 to counteract the inhibitory effect of interferon is attributable to the Ebola virus VP35 protein.
FIG. 2.
(A) Viral response to interferon. Monolayers of Vero cells were not treated (IFN−) or pretreated with human leukocyte alpha interferon (IFN+) (1,000 U/ml; Sigma) for 20 h. Cells were then infected at 0.05 PFU per cell with the indicated viruses. At 72 h postinfection, cells were harvested and freeze-thawed three times, and virus yield was determined on Vero cells. Data represent the averages plus standard deviations (error bars) from three independent experiments. (B) Kinetics of viral growth. Virus infection was carried out as described above for panel A, except that cells were harvested at different time points postinfection. The data represent the averages of duplicate samples, with the standard deviations indicated by the error bars.
To examine the kinetics of viral growth, virus yields were measured at various points during a 48-h course of infection. As illustrated in Fig. 2B, recombinant viruses MC0201, HSV-BAC, and KY0234 replicated efficiently in the absence of interferon. Virus growth increased steadily as infection proceeded, with titers reaching 2.4 × 108 to 3.9 × 108 PFU/ml at 48 h postinfection. The slightly lower virus yields of KY0234 at early time points may reflect the effect of γ134.5 deletion from HSV. When cells were pretreated with interferon, MC0201 and HSV-BAC still replicated efficiently. Virus growth continued to increase over the course of infection, with titers reaching 9.3 × 106 to 4.4 × 107 PFU/ml at 48 h postinfection. However, under this condition, KY0234 replicated poorly. Virus yields barely increased, with a titer reaching only 2.35 × 103 PFU/ml at 48 h postinfection. Hence, like the wild-type γ134.5 protein, the Ebola virus VP35 protein counteracts the inhibitory effect of alpha interferon.
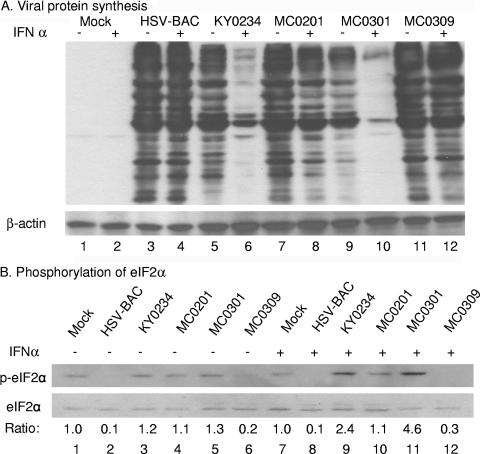
The VP35 protein facilitates viral polypeptide synthesis that inversely correlates with eIF-2α phosphorylation.
We next examined viral protein production for the recombinant viruses. This was done in Vero cells that were untreated or pretreated with alpha interferon for 20 h. At 15 h postinfection, cells were harvested, and samples were subjected to Western blot analysis with a polyclonal antibody against all HSV-1 antigens. As shown in Fig. 3A, there are significant levels of viral protein accumulation in cells either mock infected or infected with recombinant virus HSV-BAC, MC0201, or MC0309 in the presence and absence of interferon. However, in cells infected with recombinant virus KY0234 or MC0301, there is a dramatic reduction of viral protein accumulation in response to alpha interferon treatment (Fig. 3A, lanes 6 and 10). Levels of β-actin expression were comparable in mock- and virus-infected cells. On the basis of this analysis, we assessed the phosphorylation state of eIF-2α. Relative eIF-2α phosphorylation was quantitated and normalized to that in mock-infected cells. As illustrated in Fig. 3B, in the absence of interferon, no detectable level of eIF-2α phosphorylation was observed in cells infected with wild-type HSV-BAC. Only low levels of eIF-2α phosphorylation were observed in Vero cells infected with KY0234, MC0201, and MC0301, similar to the background level of eIF-2α phosphorylation in mock-infected cells. In the presence of interferon, an elevated level eIF-2α phosphorylation (two- to fourfold) was observed in cells infected with KY0234 or MC0301. Little or no eIF-2α phosphorylation was seen in cells infected with HSV-BAC or MC0309. A low background level of eIF-2α phosphorylation was detected in MC0201-infected cells. Thus, viral protein synthesis inversely correlated with eIF-2α phosphorylation in response to interferon treatment. These experiments suggest that the VP35 protein of Ebola virus facilitates viral protein synthesis by suppressing eIF-2α phosphorylation.
FIG. 3.
(A) Viral protein accumulation in the presence and absence of interferon. Monolayers of Vero cells were not treated (−) or were pretreated (+) with human leukocyte alpha interferon (IFN α) (1,000 U/ml; Sigma) for 20 h. Cells were then mock infected or infected with the indicated viruses at 1.0 PFU per cell. At 18 h postinfection, cells were harvested, washed with phosphate-buffered saline, resuspended in disruption buffer, electrophoretically separated on a denaturing 12% polyacrylamide gel, transferred to a nitrocellulose sheet, and probed with a rabbit polyclonal antibody against all HSV-1 antigens as suggested by the manufacturer (Dako Corporation). β-Actin was probed as a loading control. (B) Effect of the VP35 protein on eIF-2α phosphorylation. Vero cells, untreated or pretreated with alpha interferon, were infected with viruses (1 PFU/cell), and lysates of cells were prepared 18 h postinfection. Samples were subjected to immunoblot analysis using rabbit antibody against phospho-Ser51 eIF-2α (Biosource, Inc.) or eIF-2α (Cell Signaling Technology, Inc.). The positions of eIF-2α and phosphorylated eIF-2α (p-eIF2α) are indicated on the left. The ratio between the amounts of phosphorylated eIF-2α and total eIF-2α in each lane were quantitated by densitometry, and the numbers indicate the ratios after normalization to mock-infected cells.
The VP35 protein of Ebola virus negatively modulates the PKR pathway.
In response to virus infection, PKR is activated to phosphorylate eIF-2α at Ser51. In this process, autophosphorylation of several residues including Thr446 of PKR is required for its activation (17, 18). To determine whether the VP35 protein inhibits PKR activation, we examined the phosphorylation states of PKR and eIF-2α in cells infected with viruses including wild-type HSV-BAC, the γ134.5 null mutant virus KY0234, and the VP35-expressing virus MC0201. Cells were infected with viruses, and samples were processed for Western blot analysis using antibodies that recognize PKR, phosphorylated Thr446 on PKR, phosphorylated Ser51 on eIF-2α, or eIF-2α. Figure 4 shows that in the absence of interferon, while PKR was detected in all cells, little PKR phosphorylation was seen in cells infected with the γ134.5 null mutant KY0234. This band was not seen in cells mock infected or infected with wild-type HSV-BAC or the VP35-expressing virus MC0201 (Fig. 4, lanes 1 to 4). In this experiment, levels of total eIF-2α were comparable. A basal level of eIF-2α phosphorylation was seen in cells mock infected or infected with MC0201. A slight increase in eIF-2α phosphorylation in cells infected with KY0234 may result from activation of a low level of PKR or other eIF-2α kinases. Obviously, eIF-2α phosphorylation was reduced in cells infected with HSV-BAC, which is attributable to dephosphorylation of eIF-2α mediated by the γ134.5 protein. In the presence of interferon, the PKR phosphorylation level was elevated significantly in cells infected with KY0234 but not in cells mock infected or infected with HSV-BAC (Fig. 4, lanes 5 and 6). PKR was phosphorylated in MC0201-infected cells, but to an extent much less than that in KY0234-infected cells (Fig. 4, lanes 7 and 8). A significant increase in eIF-2α phosphorylation was seen in cells infected with KY0234 compared to that in mock-infected cells. Only a marginal increase in eIF-2α phosphorylation was detected in cells infected with MC0201. This increase was not observed in cells infected with HSV-BAC (Fig. 4, lanes 5 to 8). These results suggest that the VP35 protein inhibits activation of PKR induced by virus infection.
FIG. 4.
Inhibition of PKR activity by the VP35 protein. Vero cells were left untreated (−IFN-α) or pretreated with human alpha interferon (+IFN-α) (1,000 units/ml; Sigma) for 20 h. Cells were then mock infected or infected with the indicated viruses at 1 PFU per cell. At 18 h postinfection, cells were harvested. Cell lysates were prepared and subjected to immunoblotting using rabbit antibody against PKR, phospho-Thr446 PKR (P-PKR), phospho-Ser51eIF-2α (P-eIF2α), or eIF-2α. The ratio between phosphorylated eIF-2α and total eIF-2α in each lane were measured as described in the legend to Fig. 3.
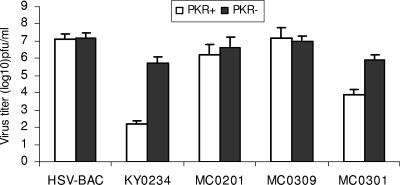
To further investigate the link between the VP35 protein and PKR, we measured replication of the recombinant viruses in embryo fibroblasts derived from PKR+/+ and PKR−/− mice. Monolayers of PKR+/+ and PKR−/− cells were pretreated with mouse alpha/beta interferon and then infected with the recombinant viruses. At 48 h postinfection, cells were harvested and virus yields were measured. As shown in Fig. 5, in PKR+/+ cells, recombinant virus HSV-BAC replicated efficiently, and virus yield reached 1.3 × 107 PFU/ml. In contrast, recombinant virus KY0234 reached a titer of only 1.6 × 102 PFU/ml. Replication of recombinant virus MC0201 reached a titer of 1.7 × 106 PFU/ml, which is only a 10-fold decrease from that of HSV-BAC. MC0309 also showed efficient virus replication compared to HSV-BAC, while MC0301 replicated poorly and is similar to the γ134.5 deletion virus KY0234. In PKR−/− cells, replication of the recombinant viruses was not affected by alpha/beta interferon. These data indicate that the VP35 protein renders virus replication resistant to the interferon-induced PKR response.
FIG. 5.
(A) Effect of alpha/beta interferon on replication of recombinant viruses in PKR+/+ and PKR−/− mouse fibroblast cells. Cells were pretreated with mouse alpha/beta interferon (1,000 U/ml) for 20 h. Cells were then either mock infected (PKR−) or infected with the recombinant viruses (PKR+) at 0.05 PFU per cell and incubated at 37°C for 48 h. Cells were harvested and freeze-thawed three times, and virus yield was determined on Vero cells. The data represent the averages of triplicate samples, with the standard deviations indicated by error bars.
Mutations in the VP35 protein have differential effects on viral interferon responses.
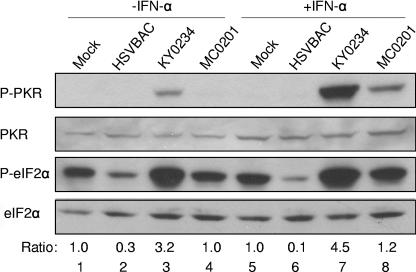
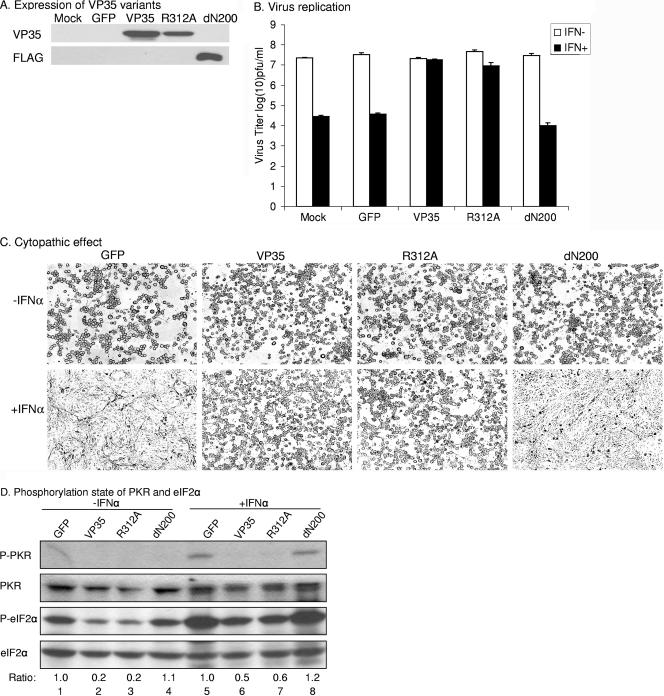
To determine which portion of the VP35 protein blocks the PKR response, we constructed lentiviral vectors expressing either wild-type VP35, an amino-terminal truncation mutant dΝ200, or a mutant VP35 with an R312A substitution. Vero cells were transduced with these viral constructs, and the expression of VP35 was verified by Western blot analysis using antibodies against the amino terminus of VP35 (VP35 and R312A) and FLAG (dN200) (Fig. 6A). The γ134.5 deletion mutant was then used to challenge the cells pretreated or untreated with alpha interferon, and viral yields were measured. As shown in Fig. 6B, in the absence of interferon, the γ134.5 deletion mutant replicated efficiently in control cells or cells expressing VP35 variants, with titers ranging from 2.0 × 107 to 3.4 × 107 PFU/ml. In correlation, these cells displayed dramatic morphological changes after exposure to the γ134.5 null mutant (Fig. 6C). In the presence of interferon, the γ134.5 null mutant replicated efficiently only in cells expressing wild-type VP35 or the VP35 mutant with an R312A substitution, with titers reaching 1.8 × 107 and 9.4 × 106 PFU/ml, respectively. As expected, these cells exhibited extensive cytopathic effects (Fig. 6C). In sharp contrast, in control cells and cells expressing mutant dN200, replication of the γ134.5 null mutant decreased drastically, with titers ranging from 1.0 ×104 to 3.6 × 104 PFU/ml (Fig. 6B). Accordingly, no obvious cytopathic effects were observed due to poor viral replication (Fig. 6C). Western blot analysis revealed that unlike cells expressing wild-type VP35 and VP35 with R312A, cells expressing GFP or dN200 exhibited elevated phosphorylation of PKR and eIF-2α after interferon treatment (Fig. 6D). Therefore, a deletion of amino acids 1 to 200, but not an R312A substitution in the VP35 protein, abrogated the function required to block the PKR response.
FIG. 6.
Mutational analysis of the VP35 protein. (A) Expression of VP35 variants. Retroviral vectors expressing GFP, VP35, VP35(R312A), or VP35(dN200) were transfected together with HIVtrans and vesicular stomatitis virus G into 293T cells. Forty-eight hours after transfection, supernatant was used to transduce Vero cells. Expression of VP35 from transduced Vero cells was examined by Western blotting using anti-VP35 and anti-FLAG antibodies. (B) Effects of VP35 variants on viral resistance to interferon. Transduced Vero cells were either treated with 1,000 U/ml human alpha interferon (IFN+) (Sigma) for 20 h or left untreated (IFN−) and infected with a Δγ134.5 mutant at 0.05 PFU per cell. Viruses were harvested at 72 h after infection, and the virus titers on Vero cells were determined. The data represent the averages of three experiments with the standard deviations indicated by error bars. (C) Cytopathic effects. Images were taken from a representative experiment as described above for panel B. (D) Phosphorylation states of PKR and eIF-2α. Transduced Vero cells were either treated with human alpha interferon (+IFNα) (Sigma) or left untreated (−IFNα) and then infected with a Δγ134.5 mutant infection at 1.0 PFU per cell. Infected-cell lysates were prepared at 24 h after infection and subjected to immunoblot analysis using the indicated antibody. The ratio between phosphorylated eIF-2α and total eIF-2α in each lane was measured as described in the legend to Fig. 3. P-PKR, phosphorylated PKR.
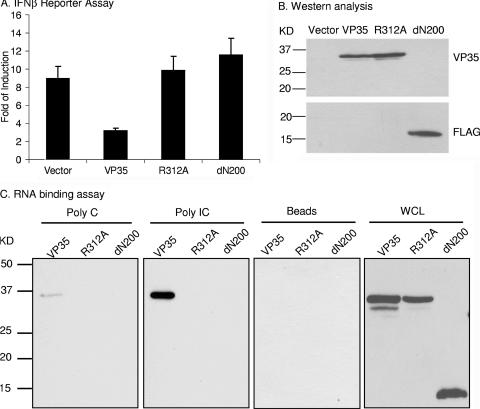
In a parallel experiment, we also assessed the effects of VP35 variants on expression of the beta interferon promoter. As shown in Fig. 7A, in reporter assays, wild-type VP35, but not the mutant with the R312A substitution, blocked the induction of the beta interferon promoter by Sendai virus, which is consistent with the results of previous studies (2, 25). Moreover, the amino-terminal truncation mutant dN200 failed to inhibit the induction of the beta interferon promoter. Western blot analysis showed that VP35 variants were expressed at comparable levels in transfected cells (Fig. 7B). Because R312 is located in a predicted RNA binding motif in the VP35 protein (25), we further tested whether this region serves as a RNA binding domain. In this experiment, lysates of cells transfected with VP35 variants were tested for binding of either single-stranded RNA or dsRNA. After incubation, samples were processed for Western blot analysis. As shown in Fig. 7C, wild-type VP35 was able to bind both poly(C) and poly(I · C), but it had a higher affinity for poly(I · C). Wild-type VP35 and its derivatives did not bind the control beads. This suggests that VP35 is a RNA binding protein that binds double-stranded RNA and probably single-stranded RNA. Notably, the R312A and dN200 mutants were not able to bind either poly(C) or poly(I · C). Collectively, these results suggest that both the amino-terminal and carboxyl-terminal domains of the VP35 protein are crucial to evade interferon responses. Moreover, the ability of the VP35 protein to bind RNA is likely required for inhibition of beta interferon induction, but not PKR activity.
FIG. 7.
(A) Effects of VP35 variants on the beta interferon promoter. Plasmids expressing GFP, VP35, VP35(R312A), or dN200 were transfected along with 50 ng beta interferon reporter gene and Renilla luciferase gene under the thymidine kinase promoter. Twenty-four hours after transfection, cells were infected with Sendai virus. The luciferase activities were measured 24 h after infection. The relative beta interferon promoter activities were normalized to Renilla luciferase activity. Data represent the averages plus standard deviations (error bars) from two independent experiments. (B) The expression of VP35 variants in panel A was analyzed by Western blot analysis using antibodies against VP35 (VP35 and R312A) and FLAG (dN200). (C) RNA binding analysis. 293T cells were transfected with plasmid constructs expressing FLAG-tagged VP35, VP35 (R312A), and dN200. Whole-cell lysates (WCL) were prepared and incubated with poly(C), poly(I · C)-conjugated beads (Poly IC), or empty beads. After centrifugation, samples were subjected to electrophoresis and immunoblot analysis with anti-FLAG antibody. As controls for protein expression, aliquots of whole-cell lysates were used to detect the expression of VP35 variants. The positions of molecular mass markers (in kilodaltons) are shown to the left of the gels in panels B and C.
DISCUSSION
Ebola virus suppresses host interferon responses, which contributes to the pathogenesis of viral infection (3, 6, 7, 25, 30, 40). In this context, the VP35 protein blocks interferon production induced by virus or double-stranded RNA, which involves the inhibition of IRF-3 activation (2). In this study, we established that the VP35 protein counteracts the antiviral action of interferon in infected cells. This activity depends on the ability of the VP35 protein to suppress the pathway regulated by double-stranded RNA-dependent protein kinase PKR. These observations support the notion that the VP35 protein interferes with one or more components of the interferon pathways, which facilitates rapid spread and dissemination of Ebola virus.
Our experimental results showed that the VP35 protein functions at a step after interferon production. This observation extended the previous finding that the VP35 functions as an interferon antagonist (2, 3). In response to pretreatment with alpha interferon, replication of the VP35 recombinant virus was similar to that of wild-type virus in Vero cells, whereas the γ134.5 deletion virus was sensitive to interferon. When VP35 of Ebola virus was replaced with a γ134.5 mutant (R215L substitution) that is sensitive to interferon (9), virus replication was decreased more than 1,000-fold in Vero cells pretreated with alpha interferon. We further observed that growth of the VP35-expressing Ebola virus remained efficient in the continuous presence of alpha interferon (data not shown). These results correlated well with profiles of viral protein synthesis in Vero cells, which are unable to produce endogenous interferon. As the JAK/STAT signaling pathway is operative in Vero cells, it is apparent that the VP35 protein functions to target a downstream effector molecule induced by alpha/beta interferon.
Ebola virus is insensitive to interferon, although phosphorylation of STAT1 and STAT2 was not affected (30, 32). This raises the possibility that Ebola virus blocks one or more steps after STAT phosphorylation. Indeed, a recent study revealed that Ebola virus VP24 binds to karyopherin α1 and inhibits STAT1 nuclear accumulation (41). Because induction of interferon-inducible genes is reduced but not completely blocked in Ebola virus-infected cells (32), it is reasonable to hypothesize that Ebola virus has additional ways to cope with the antiviral activity of effector molecules. In this context, our data suggest that the VP35 protein may be required to overcome the antiviral action of interferon during Ebola virus infection. Two lines of evidence indicate that the VP35 protein interferes with the PKR pathway. First, the VP35 protein inhibited phosphorylation of PKR and eIF-2α. Although we noticed some variations in the extent of PKR and eIF-2α phosphorylation in infected cells, PKR phosphorylation in general correlated well with eIF-2α phosphorylation. These results were reproducible in several experiments. It is possible that variations in the extent of eIF-2α phosphorylation may stem from a compounding effect of PKR and possibly other eIF-2α kinases. Second, in the presence of interferon, the VP35 protein was required for viral replication in PKR+/+ cells but not in PKR−/− cells. Hence, in addition to inhibiting interferon production, the VP35 protein counteracts the activity of PKR.
PKR is a key component in mediating the interferon-induced antiviral response (18). In response to virus infection, PKR forms a homodimer and autophosphorylates on multiple serine, threonine, and tyrosine residues (17, 18, 44). These series of events convert PKR into an active enzyme that phosphorylates eIF-2α at serine 51. Interpreted within the framework of this model, our data strongly suggest that in cells infected with Ebola virus, the VP35 protein may serve to block the activation of PKR and thereby abrogate the first line of host defense. While inhibition of the PKR response by the VP35 protein provides a favorable environment for viral infection, the mechanism by which it works remains elusive. We failed to detect the physical interaction of Ebola virus VP35 with PKR in pull-down assays and dephosphorylation of eIF-2α by Ebola virus VP35 (data not shown). These results do not prove but imply that the VP35 protein may regulate the PKR activity by a different mechanism(s). It is generally believed that double-stranded RNA produced in virus-infected cells is the activator of PKR. The VP35 protein, in principle, may act as a decoy of double-stranded RNA. Experiments to test this hypothesis thus far yielded a negative result. We found that VP35 is a RNA binding protein and that the R312A substitution disrupted this activity. These results confirmed the prediction that Ebola virus VP35 has an RNA binding domain (25). It is also in line with a recent observation that Ebola virus VP35 is a dsRNA binding protein in which both R312 and K309 are essential for its dsRNA binding activity (8). Unexpectedly, the R312A mutant remained competent to antagonize the interferon response mediated by PKR in our study. In this regard, the VP35 protein appears to act independently of its RNA binding activity. An intriguing possibility is that the VP35 protein may subvert the activity of PACT, a cellular protein that activates PKR under stress conditions (29, 38). Alternatively, the VP35 protein may act on an unidentified cellular component(s) that regulates PKR. Additional experimentation is necessary to define the precise role of the VP35 protein.
Mutational analysis suggests that the amino terminus is required to inhibit interferon responses. Deletion of amino acids 1 to 200 compromised the ability of the VP35 protein to inhibit the PKR activity and the expression of beta interferon. It is noteworthy that the region containing amino acids 82 to 118 is predicted to form a coiled-coil domain, which is required for the oligomerization of the VP35 protein (40). This raises the possibility that oligomerization of the VP35 protein plays a role not only in blocking interferon production but also in the PKR response. Currently, work is in progress to test this hypothesis.
The carboxyl terminus of the VP35 protein is involved in blocking activation of IRF-3, which stimulates the synthesis of beta interferon (2, 25, 40). In agreement with these findings, we observed that protein inhibited the induction of the beta interferon promoter mediated by Sendai virus and the R312A substitution abolished this activity. While the carboxyl terminus is highly conserved among the VP35 proteins encoded by different filoviruses (25), the region encompassing arginine 312 is homologous to a RNA binding region in the NS1 protein of influenza A virus (25). Since the mutant with the R312A substitution failed to bind RNA, we speculate that the VP35 protein competes for dsRNA with RIG-I or melanoma differentiation-associated gene 5 (MDA5), an RNA receptor that triggers interferon production in host cells (1, 45, 50). Recent studies suggest that in addition to inhibition of the RIG-I-mediated activity, Ebola virus VP35 blocks activation of the beta interferon promoter induced by overexpression of beta interferon promoter stimulator 1 (IPS-1) or overexpression of the IRF-3 kinases TANK-binding kinase 1 (TBK1) and IκB kinase ɛ independently of its RNA binding activity, suggesting that additional mechanisms of inhibition exist at a point proximal to the IRF-3 kinases (8). We provided evidence that Ebola virus VP35 interferes with the PKR pathway and that this function does not require its RNA binding activity. This is similar to the observation that mutations in the RNA binding motif of the NS1 protein of influenza A virus have no effect on its abilities to bind and inhibit the PKR activity (33). It remains to be established whether other regions of the carboxyl-terminal domain in VP35 are required to inhibit the PKR response. Taken in combination, these data suggest that the VP35 protein interacts with multiple pathways of the interferon system.
To date, many viruses studied have evolved a variety of mechanisms to counteract PKR by preventing the activation of PKR or the phosphorylation of eIF-2α or by promoting the degradation of PKR (18). For example, adenovirus VAI RNA, vaccinia virus K3L protein, and influenza virus-induced p58IPK protein interact with PKR and block its activation (4, 19, 39, 48). Similarly, the NS5A and E2 proteins of hepatitis C virus bind to and inhibit PKR activation (20, 47). In addition, the herpes simplex virus γ134.5 protein directs the cellular protein phosphatase 1 to dephosphorylate eIF-2α (26), and poliovirus employs cellular proteinase to degrade PKR (5). The fact that the Ebola virus VP35 protein interferes with PKR activity suggests that this function encoded by the VP35 protein may contribute to the pathogenesis of Ebola virus infection.
Acknowledgments
This work was supported by grant AI 053386 from the National Institute of Allergy and Infectious Diseases to B.H.
We are grateful to Irene Klain, Kui Yang, and Dustin Verpooten for assistance. We thank Hans-Dieter Klenk, Peter Palese, and Christopher F. Basler for plasmid pcdna3-EBO-35. We are also grateful to Bernard Roizman, Thomas Hope, and Bryan Williams for valuable reagents.
Footnotes
Published ahead of print on 25 October 2006.
REFERENCES
- 1.Andrejeva, J., K. S. Childs, D. F. Young, T. S. Carlos, N. Stock, S. Goodbourn, and R. E. Randall. 2004. The V proteins of paramyxoviruses bind the IFN-inducible RNA helicase, mda-5, and inhibit its activation of the IFN-beta promoter. Proc. Natl. Acad. Sci. USA 101:17264-17269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Basler, C. F., A. Mikulasova, L. Martinez-Sobrido, J. Paragas, E. Muhlberger, M. Bray, H. D. Klenk, P. Palese, and A. Garcia-Sastre. 2003. The Ebola virus VP35 protein inhibits activation of interferon regulatory factor 3. J. Virol. 77:7945-7956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Basler, C. F., X. Wang, E. Muhlberger, V. Volchkov, J. Paragas, H. D. Klenk, A. Garcia-Sastre, and P. Palese. 2000. The Ebola virus VP35 protein functions as a type I IFN antagonist. Proc. Natl. Acad. Sci. USA 97:12289-12294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beattie, E., J. Tartaglia, and E. Paoletti. 1991. Vaccinia virus-encoded eIF-2 alpha homolog abrogates the antiviral effect of interferon. Virology 183:419-422. [DOI] [PubMed] [Google Scholar]
- 5.Black, T. L., B. Safer, A. Hovanessian, and M. G. Katze. 1989. The cellular 68,000-Mr protein kinase is highly autophosphorylated and activated yet significantly degraded during poliovirus infection: implications for translational regulation. J. Virol. 63:2244-2251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bosio, C. M., M. J. Aman, C. Grogan, R. Hogan, G. Ruthel, D. Negley, M. Mohamadzadeh, S. Bavari, and A. Schmaljohn. 2003. Ebola and Marburg viruses replicate in monocyte-derived dendritic cells without inducing the production of cytokines and full maturation. J. Infect. Dis. 188:1630-1638. [DOI] [PubMed] [Google Scholar]
- 7.Bray, M. 2001. The role of the type I interferon response in the resistance of mice to filovirus infection. J. Gen. Virol. 82:1365-1373. [DOI] [PubMed] [Google Scholar]
- 8.Cárdenas, W. B., Y. M. Loo, M. Gale, Jr., A. L. Hartman, C. R. Kimberlin, L. Martnez-Sobrido, E. O. Saphire, and C. F. Basler. 2006. Ebola virus VP35 protein binds double-stranded RNA and inhibits alpha/beta interferon production induced by RIG-I signaling. J. Virol. 80:5168-5178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cerveny, M., S. Hessefort, K. Yang, G. Cheng, M. Gross, and B. He. 2003. Amino acid substitutions in the effector domain of the γ134.5 protein of herpes simplex virus 1 have differential effects on viral response to interferon-α. Virology 307:290-300. [DOI] [PubMed] [Google Scholar]
- 10.Cheng, G., M. E. Brett, and B. He. 2001. Val193 and Phe195 of the γ134.5 protein of herpes simplex virus 1 are required for viral resistance to interferon α/β. Virology 290:115-120. [DOI] [PubMed] [Google Scholar]
- 11.Cheng, G., M. Gross, M. E. Brett, and B. He. 2001. AlaArg motif in the carboxyl terminus of the γ134.5 protein of herpes simplex virus type 1 is required for the formation of a high-molecular-weight complex that dephosphorylates eIF-2α. J. Virol. 75:3666-3674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheng, G., K. Yang, and B. He. 2003. Dephosphorylation of eIF-2α mediated by the γ134.5 protein of herpes simplex virus type 1 is required for viral response to interferon but is not sufficient for efficient viral replication. J. Virol. 77:10154-10161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chou, J., E. R. Kern, R. J. Whitley, and B. Roizman. 1990. Mapping of herpes simplex virus-1 neurovirulence to γ134.5, a gene nonessential for growth in culture. Science 250:1262-1266. [DOI] [PubMed] [Google Scholar]
- 14.Chou, J., and B. Roizman. 1992. The γ134.5 gene of herpes simplex virus 1 precludes neuroblastoma cells from triggering total shutoff of protein synthesis characteristic of programmed cell death in neuronal cells. Proc. Natl. Acad. Sci. USA 89:3266-3270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chou, J., and B. Roizman. 1994. Herpes simplex virus 1 γ134.5 gene function, which blocks the host response to infection, maps in the homologous domain of the genes expressed during growth arrest and DNA damage. Proc. Natl. Acad. Sci. USA 91:5247-5251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Der, S. D., Y. L. Yang, C. Weissmann, and B. R. Williams. 1997. A double-stranded RNA-activated protein kinase-dependent pathway mediating stress-induced apoptosis. Proc. Natl. Acad. Sci. USA 94:3279-3283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dey, M., C. Cao, A. C. Dar, T. Tamura, K. Ozato, F. Sicheri, and T. E. Dever. 2005. Mechanistic link between PKR dimerization, autophosphorylation, and eIF2alpha substrate recognition. Cell 122:901-913. [DOI] [PubMed] [Google Scholar]
- 18.Gale, M., Jr., and M. G. Katze. 1998. Molecular mechanisms of interferon resistance mediated by viral-directed inhibition of PKR, the interferon-induced protein kinase. Pharmacol. Ther. 78:29-46. [DOI] [PubMed] [Google Scholar]
- 19.Gale, M., Jr., S. L. Tan, M. Wambach, and M. G. Katze. 1996. Interaction of the interferon-induced PKR protein kinase with inhibitory proteins P58IPK and vaccinia virus K3L is mediated by unique domains: implications for kinase regulation. Mol. Cell. Biol. 16:4172-4181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gale, M. J., Jr., M. J. Korth, N. M. Tang, S. L. Tan, D. A. Hopkins, T. E. Dever, S. J. Polyak, D. R. Gretch, and M. G. Katze. 1997. Evidence that hepatitis C virus resistance to interferon is mediated through repression of the PKR protein kinase by the nonstructural 5A protein. Virology 230:217-227. [DOI] [PubMed] [Google Scholar]
- 21.Gibb, T. R., D. A. Norwood, Jr., N. Woollen, and E. A. Henchal. 2002. Viral replication and host gene expression in alveolar macrophages infected with Ebola virus (Zaire strain). Clin. Diagn. Lab. Immunol. 9:19-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gupta, M., S. Mahanty, R. Ahmed, and P. E. Rollin. 2001. Monocyte-derived human macrophages and peripheral blood mononuclear cells infected with Ebola virus secrete MIP-1alpha and TNF-alpha and inhibit poly-IC-induced IFN-alpha in vitro. Virology 284:20-25. [DOI] [PubMed] [Google Scholar]
- 23.Harcourt, B. H., A. Sanchez, and M. K. Offermann. 1998. Ebola virus inhibits induction of genes by double-stranded RNA in endothelial cells. Virology 252:179-188. [DOI] [PubMed] [Google Scholar]
- 24.Harcourt, B. H., A. Sanchez, and M. K. Offermann. 1999. Ebola virus selectively inhibits responses to interferons, but not to interleukin-1β, in endothelial cells. J. Virol. 73:3491-3496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hartman, A. L., J. S. Towner, and S. T. Nichol. 2004. A C-terminal basic amino acid motif of Zaire ebolavirus VP35 is essential for type I interferon antagonism and displays high identity with the RNA-binding domain of another interferon antagonist, the NS1 protein of influenza A virus. Virology 328:177-184. [DOI] [PubMed] [Google Scholar]
- 26.He, B., M. Gross, and B. Roizman. 1997. The γ134.5 protein of herpes simplex virus 1 complexes with protein phosphatase 1alpha to dephosphorylate the alpha subunit of the eukaryotic translation initiation factor 2 and preclude the shutoff of protein synthesis by double-stranded RNA-activated protein kinase. Proc. Natl. Acad. Sci. USA 94:843-848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Horsburgh, B. C., M. M. Hubinette, D. Qiang, M. L. MacDonald, and F. Tufaro. 1999. Allele replacement: an application that permits rapid manipulation of herpes simplex virus type 1 genomes. Gene Ther. 6:922-930. [DOI] [PubMed] [Google Scholar]
- 28.Huang, Y., L. Xu, Y. Sun, and G. Nabel. 2002. The assembly of Ebola virus nucleocapsid requires virion-associated proteins 35 and 24 and posttranslational modification of nucleoprotein. Mol. Cell 10:307-316. [DOI] [PubMed] [Google Scholar]
- 29.Ito, T., M. Yang, and W. S. May. 1999. RAX, a cellular activator for double-stranded RNA-dependent protein kinase during stress signaling. J. Biol. Chem. 274:15427-15432. [DOI] [PubMed] [Google Scholar]
- 30.Jahrling, P. B., T. W. Geisbert, J. B. Geisbert, J. R. Swearengen, M. Bray, N. K. Jaax, J. W. Huggins, J. W. LeDuc, and C. J. Peters. 1999. Evaluation of immune globulin and recombinant interferon-alpha2b for treatment of experimental Ebola virus infections. J. Infect. Dis. 179(Suppl. 1):S224-S234. [DOI] [PubMed] [Google Scholar]
- 31.Jing, X., M. Cerveny, K. Yang, and B. He. 2004. Replication of herpes simplex virus 1 depends on the γ134.5 functions that facilitate virus response to interferon and egress in the different stages of productive infection. J. Virol. 78:7653-7666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kash, J. C., E. Muhlberger, V. Carter, M. Grosch, O. Perwitasari, S. C. Proll, M. J. Thomas, F. Weber, H. D. Klenk, and M. G. Katze. 2006. Global suppression of the host antiviral response by Ebola- and Marburgviruses: increased antagonism of the type I interferon response is associated with enhanced virulence. J. Virol. 80:3009-3020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li, S., J. Y. Min, R. M. Krug, and G. C. Sen. 2006. Binding of the influenza A virus NS1 protein to PKR mediates the inhibition of its activation by either PACT or double-stranded RNA. Virology 349:13-21. [DOI] [PubMed] [Google Scholar]
- 34.Mahanty, S., K. Hutchinson, S. Agarwal, M. McRae, P. E. Rollin, and B. Pulendran. 2003. Cutting edge: impairment of dendritic cells and adaptive immunity by Ebola and Lassa viruses. J. Immunol. 170:2797-2801. [DOI] [PubMed] [Google Scholar]
- 35.Mühlberger, E., M. Weik, V. E. Volchkov, H. D. Klenk, and S. Becker. 1999. Comparison of the transcription and replication strategies of Marburg virus and Ebola virus by using artificial replication systems. J. Virol. 73:2333-2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Naldini, L., U. Blomer, F. H. Gage, D. Trono, and I. M. Verma. 1996. Efficient transfer, integration, and sustained long-term expression of the transgene in adult rat brains injected with a lentiviral vector. Proc. Natl. Acad. Sci. USA 93:11382-11388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Neumann, G., H. Feldmann, S. Watanabe, I. Lukashevich, and Y. Kawaoka. 2002. Reverse genetics demonstrates that proteolytic processing of the Ebola virus glycoprotein is not essential for replication in cell culture. J. Virol. 76:406-410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Patel, R. C., and G. C. Sen. 1998. PACT, a protein activator of the interferon-induced protein kinase, PKR. EMBO J. 17:4379-4390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Polyak, S. J., N. Tang, M. Wambach, G. N. Barber, and M. G. Katze. 1996. The P58 cellular inhibitor complexes with the interferon-induced, double-stranded RNA-dependent protein kinase, PKR, to regulate its autophosphorylation and activity. J. Biol. Chem. 271:1702-1707. [DOI] [PubMed] [Google Scholar]
- 40.Reid, S. P., W. B. Cardenas, and C. F. Basler. 2005. Homo-oligomerization facilitates the interferon-antagonist activity of the ebolavirus VP35 protein. Virology 341:179-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Reid, S. P., L. W. Leung, A. L. Hartman, O. Martinez, M. L. Shaw, C. Carbonnelle, V. E. Volchkov, S. T. Nichol, and C. F. Basler. 2006. Ebola virus VP24 binds karyopherin α1 and blocks STAT1 nuclear accumulation. J. Virol. 80:5156-5167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sen, G. C. 2001. Viruses and interferons. Annu. Rev. Microbiol. 55:255-281. [DOI] [PubMed] [Google Scholar]
- 43.Stark, G. R., I. M. Kerr, B. R. Williams, R. H. Silverman, and R. D. Schreiber. 1998. How cells respond to interferons. Annu. Rev. Biochem. 67:227-264. [DOI] [PubMed] [Google Scholar]
- 44.Su, Q., S. Wang, D. Baltzis, L. K. Qu, A. H. Wong, and A. E. Koromilas. 2006. Tyrosine phosphorylation acts as a molecular switch to full-scale activation of the eIF2α RNA-dependent protein kinase. Proc. Natl. Acad. Sci. USA 103:63-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sumpter, R., Jr., Y. M. Loo, E. Foy, K. Li, M. Yoneyama, T. Fujita, S. M. Lemon, and M. Gale, Jr. 2005. Regulating intracellular antiviral defense and permissiveness to hepatitis C virus RNA replication through a cellular RNA helicase, RIG-I. J. Virology 79:2689-2699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Takada, A., and Y. Kawaoka. 2001. The pathogenesis of Ebola hemorrhagic fever. Trends Microbiol. 9:506-511. [DOI] [PubMed] [Google Scholar]
- 47.Taylor, D. R., S. T. Shi, P. R. Romano, G. N. Barber, and M. M. Lai. 1999. Inhibition of the interferon-inducible protein kinase PKR by HCV E2 protein. Science 285:107-110. [DOI] [PubMed] [Google Scholar]
- 48.Thimmappaya, B., C. Weinberger, R. J. Schneider, and T. Shenk. 1982. Adenovirus VAI RNA is required for efficient translation of viral mRNAs at late times after infection. Cell 31:543-551. [DOI] [PubMed] [Google Scholar]
- 49.Volchkov, V. E., V. A. Volchkova, E. Muhlberger, L. V. Kolesnikova, M. Weik, O. Dolnik, and H. D. Klenk. 2001. Recovery of infectious Ebola virus from complementary DNA: RNA editing of the GP gene and viral cytotoxicity. Science 291:1965-1969. [DOI] [PubMed] [Google Scholar]
- 50.Yoneyama, M., M. Kikuchi, K. Matsumoto, T. Imaizumi, M. Miyagishi, K. Taira, E. Foy, Y. M. Loo, M. Gale, Jr., S. Akira, S. Yonehara, A. Kato, and T. Fujita. 2005. Shared and unique functions of the DExD/H-box helicases RIG-I, MDA5, and LGP2 in antiviral innate immunity. J. Immunol. 175:2851-2858. [DOI] [PubMed] [Google Scholar]