Abstract
Infection with Histoplasma capsulatum occurs commonly in areas in the Midwestern United States and Central America, but symptomatic disease requiring medical care is manifest in very few patients. The extent of disease depends on the number of conidia inhaled and the function of the host's cellular immune system. Pulmonary infection is the primary manifestation of histoplasmosis, varying from mild pneumonitis to severe acute respiratory distress syndrome. In those with emphysema, a chronic progressive form of histoplasmosis can ensue. Dissemination of H. capsulatum within macrophages is common and becomes symptomatic primarily in patients with defects in cellular immunity. The spectrum of disseminated infection includes acute, severe, life-threatening sepsis and chronic, slowly progressive infection. Diagnostic accuracy has improved greatly with the use of an assay for Histoplasma antigen in the urine; serology remains useful for certain forms of histoplasmosis, and culture is the ultimate confirming diagnostic test. Classically, histoplasmosis has been treated with long courses of amphotericin B. Today, amphotericin B is rarely used except for severe infection and then only for a few weeks, followed by azole therapy. Itraconazole is the azole of choice following initial amphotericin B treatment and for primary treatment of mild to moderate histoplasmosis.
INTRODUCTION
Histoplasmosis was first described a little over a century ago by an American physician, Samuel Darling, who was working in the Canal Zone in Panama. He described the disseminated form of the disease in a fatal case from Martinique (19). It took decades to prove that Histoplasma capsulatum is a dimorphic fungus, that histoplasmosis is primarily a pulmonary disease, and that the environmental reservoir is soil (25, 33).
There are two varieties of H. capsulatum that are pathogenic to humans, H. capsulatum var. capsulatum and H. capsulatum var. duboisii, and a third variety that is an equine pathogen, H. capsulatum var. farciminosum (63). H. capsulatum var. duboisii exists in Africa, and cases have been reported in both Africa and Europe, when patients from Africa seek care there. This review will focus solely on disease manifestations of H. capsulatum var. capsulatum, hereafter referred to as H. capsulatum.
H. capsulatum exists as a mold in the environment and forms a white to tan colony on Sabouraud dextrose agar at 25 to 30°C. Two types of conidia are formed. The macroconidia or tuberculate conidia are 8 to 15 μm in diameter and have a thick wall with distinctive projections on the surface; the microconidia are tiny, smooth structures that are 2 to 4 μm in diameter and are the infectious form. At 37°C in vitro and in tissues, the organism converts into the yeast phase that is composed of tiny 2- to 4-μm oval budding yeasts that are found both inside and outside macrophages. The organism is not encapsulated, although in tissues, it appears to be surrounded by a clear zone that was misinterpreted as being a capsule by Darling (19).
H. capsulatum occurs most commonly in North America and Central America, but the organism exists in many diverse areas around the world (63). In the United States, H. capsulatum is endemic in the Mississippi and Ohio River valleys and also exists in localized foci in many mideastern states. Soil containing large amounts of bird or bat guano, especially that found under blackbird roosts or next to chicken coops, supports luxuriant growth of the mold (11). Once contaminated, soil yields H. capsulatum for many years after birds no longer roost in the area. Caves can be highly contaminated by H. capsulatum that thrives on the bat guano (77).
Infection with H. capsulatum occurs during day-to-day activities in areas where H. capsulatum is highly endemic or in the course of occupational and recreational activities that disrupt the soil or accumulated dirt and guano in old buildings, on bridges, and in caves where bats have roosted (11, 59). Outbreaks that involve anywhere from a handful to tens of thousands of individuals have been described (8, 131, 136).
Every year, hundreds of thousands of individuals in the United States and Central America are infected with H. capsulatum. Most do not realize that they have had a fungal infection. The true extent of infection with H. capsulatum in the Ohio and Mississippi River valleys was defined only after the development of a skin test antigen that could be used in epidemiological studies (12). The seminal studies by Christie and Peterson and Palmer established the relationship of histoplasmin skin test positivity to pulmonary calcifications in tuberculin-negative persons (12, 95). Subsequent large-scale population studies by the Public Health Service defined the area where H. capsulatum is endemic (32) and demonstrated that over 80% of young adults from the states bordering the Ohio and Mississippi Rivers had been previously infected with H. capsulatum.
This review will focus on the clinical, diagnostic, and therapeutic aspects of infection with this dimorphic fungus.
CLINICAL MANIFESTATIONS
Exposure to H. capsulatum is exceedingly common for persons living within areas of endemicity, but symptomatic infection is uncommon (63). The vast majority of infected persons have either no symptoms or a very mild illness that is never recognized as being histoplasmosis. The clinical manifestations described below are those that occur in the small number (<1%) of persons who develop symptoms when infected with H. capsulatum.
Pulmonary Histoplasmosis
Acute pulmonary histoplasmosis.
The usual case of acute pulmonary histoplasmosis is a self-limited illness occurring mostly in children exposed to the organism for the first time. Symptoms include fever, malaise, headache, and weakness; substernal chest discomfort and dry cough are helpful symptoms pointing toward acute pneumonia (49). Rales are heard in a minority of patients. Chest radiographs show a patchy pneumonia in one or more lobes; enlarged hilar and mediastinal lymph nodes are frequently noted (51, 156). Improvement is prompt in the majority of cases, but in some patients, fatigue may linger for several months. In some patients, chest radiographs are obtained only after the pulmonary infiltrate has cleared, and hilar lymphadenopathy is the primary finding.
Acute self-limited pulmonary histoplasmosis is accompanied by rheumatologic and/or dermatologic manifestations in approximately 5% of patients. Erythema nodosum and erythema multiforme are the most common skin manifestations; they occur most frequently in young women and are thought to be associated with a hypersensitivity response to the antigens of H. capsulatum (88, 94, 115). Myalgias and arthralgias are common symptoms during acute infection; however, a minority of patients may develop self-limited, polyarticular, symmetrical arthritis (108). Joint symptoms usually resolve over several weeks and respond to nonsteroidal anti-inflammatory agents. Patients who have hilar lymphadenopathy, arthralgias, and erythema nodosum can be mistakenly given the diagnosis of sarcoidosis (125, 144).
Included in the differential diagnosis of acute pulmonary histoplasmosis is acute pulmonary blastomycosis and atypical community-acquired pneumonias, such as those due to Mycoplasma, Legionella, and Chlamydia (see Table 1). Hilar or mediastinal lymphadenopathy is common with histoplasmosis and can be seen with blastomycosis but would be extremely uncommon with the above-listed agents that cause community-acquired pneumonia.
TABLE 1.
Differential diagnosis of pulmonary histoplasmosis
| Differential diagnosis |
|---|
| Acute pulmonary histoplasmosis |
| Blastomycosis |
| Coccidioidomycosis |
| Mycoplasma pneumonia |
| Chlamydia pneumonia |
| Legionella pneumonia |
| Chronic pulmonary histoplasmosis |
| Tuberculosis |
| Nontuberculous mycobacterial infection |
| Blastomycosis |
| Coccidioidomycosis |
| Sporotrichosis |
| Paracoccidioidomycosis |
| Sarcoidosis |
A careful history of possible exposure to H. capsulatum in the activities of daily living or during the course of travel is crucial to arriving at the correct diagnosis. Discovering that others with whom the patient has been associated have a similar illness is extremely useful information when a diagnosis of histoplasmosis is being sought (11).
The above-described picture changes when either the host is immunosuppressed or the inoculum of H. capsulatum conidia is massive. In the host who has deficient cell-mediated immunity, the pulmonary infection will frequently progress to involve multiple lobes. The patient is acutely ill with fever, chills, cough, and marked dyspnea. Rales can often be heard throughout the lung fields. Chest radiographs show bilateral diffuse reticulonodular infiltrates, and adult respiratory distress syndrome can ensue.
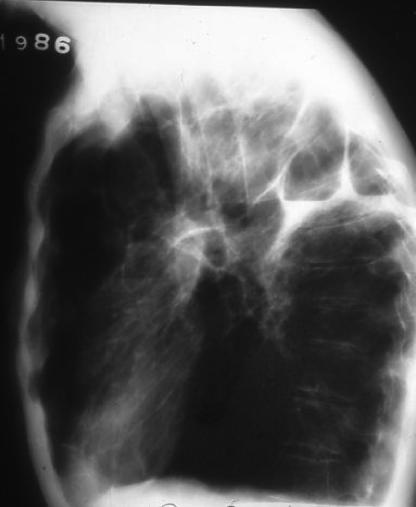
Acute severe pulmonary infection also occurs when a person is exposed to a large inoculum of H. capsulatum (49, 154). The onset of illness is abrupt, and the patient presents with fever, chills, malaise, dyspnea, cough, and chest pain. Rales may be heard throughout the lungs. Chest radiographs show diffuse pulmonary infiltrates that usually are described as reticulonodular; coalescence of nodules sometimes occurs in discrete areas of the lung (Fig. 1). Acute respiratory distress syndrome can occur within a few days (62, 164). Pleural involvement is rare. Mediastinal and hilar lymphadenopathy may or may not be present. Many patients will recover without treatment, but severe disease should always be treated, because respiratory compromise can occur and recovery without an antifungal agent is slow. As the pneumonia resolves, the remaining nodules often calcify, leaving the appearance of “buckshot” throughout the lung fields (49, 51).
FIG. 1.
Severe acute pulmonary histoplasmosis in a man who was exposed to a large inoculum of H. capsulatum while cleaning accumulated bird and bat guano from a bridge abutment.
Chronic cavitary pulmonary histoplasmosis.
Chronic cavitary pulmonary histoplasmosis is unique among fungal infections in that it appears to have a predilection for patients who are older. This may be because emphysema is intimately associated with the development of this form of histoplasmosis (47). It is distinctly unusual for a patient without preexisting pulmonary disease to develop this form of histoplasmosis. In their classic study, Goodwin et al. noted that interstitial inflammation caused by the fungal infection was usually adjacent to emphysematous bullae and frequently involved the apical and apical posterior segments of the lungs (47). Thickening of the walls of the bullae with subsequent necrosis and increasing fibrosis is common and ultimately results in the formation of large persistent cavities (Fig. 2). Volume loss of the upper lobes due to increasing fibrosis ensues. Unique to chronic cavitary histoplasmosis is the so-called “marching cavity” in which continuing necrosis increases the size of the cavity, which ultimately can consume an entire lobe. Spillage of fungal antigen into dependent portions of the lung is the presumed, but not verified, mechanism for the development of interstitial fibrosis in the lower lobes.
FIG. 2.
Lateral chest radiograph from a patient who had severe emphysema and who was severely ill with chronic cavitary pulmonary histoplasmosis.
Pleural thickening adjacent to apical cavitary lesions is common, but pleural effusions are uncommon (49). Calcified nodes may be seen in the mediastinum, but it is uncommon for patients to have mediastinal or hilar lymphadenopathy that is noted on chest radiographs in this form of histoplasmosis (156). Dissemination to other organs was not noted for the 228 patients described by Goodwin et al. (47).
Wheat et al. reported that a small proportion of persons involved in the large outbreak of histoplasmosis in Indianapolis, Indiana, in the late 1970s developed cavitary pulmonary disease (140). Not all the patients had a history of chronic obstructive pulmonary disease, and 11% appeared to resolve the cavitary lesions and all symptoms without antifungal therapy. One patient had subsequent development of disseminated histoplasmosis, a rare event in this form of histoplasmosis. The difference between the observations of this outbreak and those cases described by Goodwin et al. probably relate to the time course of infection and presentation for medical care. It is likely that the patients described by Goodwin et al., who were seen in a chest disease hospital and a Veterans Affairs medical center beginning in 1955, had more extensive disease before the diagnosis was made, and the patients described by Wheat et al., who were seen acutely in the midst of or soon after a large outbreak in the late 1970s, sought medical care and had the diagnosis of histoplasmosis made much more quickly.
The systemic manifestations of chronic cavitary pulmonary histoplasmosis include fatigue, fever, night sweats, anorexia, and weight loss. Specific pulmonary symptoms include cough, sputum production, hemoptysis, and dyspnea, which are similar to the symptoms of chronic obstructive pulmonary disease experienced by those patients. Hemoptysis is generally mild; if massive, it suggests the development of an aspergilloma in a cavity lesion (47, 60). The differential diagnosis of chronic cavitary pulmonary histoplasmosis includes, first and foremost, tuberculosis (Table 1). Nontuberculous mycobacterial infections, especially Mycobacterium avium complex and Mycobacterium kansasii; other endemic fungal infections, including blastomycosis, sporotrichosis, and coccidioidomycosis; and sarcoidosis are also possible differential diagnoses. The natural history of untreated chronic pulmonary histoplasmosis is one of progressive pulmonary insufficiency leading to death (39, 47, 96). The patients do not appear to die of overwhelming infection but rather of the consequences of the infection in lungs that are already damaged.
Granulomatous mediastinitis.
Granulomatous mediastinitis, or mediastinal granuloma, is a complication of the almost uniform infection of mediastinal lymph nodes that occurs with pulmonary infection. However, instead of enlargement of a few nodes that eventually recede and ultimately calcify as the host handles the infection, granulomatous mediastinitis is characterized by the massive enlargement of multiple nodes that are often matted together and undergo caseation necrosis. This mass of nodes remains enlarged for months to even years. The center of the mass can contain putty-like necrotic material or liquefied material. Yeast forms typical of H. capsulatum can sometimes be seen in the midst of necrotic material that is obtained by needle aspiration or tissue biopsy.
Many patients are asymptomatic, and the nodes are discovered on a chest radiograph. However, others experience symptoms related to the encroachment of this mass of nodes around mediastinal structures. These nodes can impinge on the superior vena cava, the bronchi, or the esophagus, with symptoms varying according to the structures involved. The nodes also can spontaneously drain into adjacent soft tissues of the neck, into the airways, or even into the pericardium. Although it was initially thought that granulomatous mediastinitis progressed to fibrosing mediastinitis, current thinking is that these are two separate complications of pulmonary histoplasmosis (22).
Radiographs show enlarged hilar, subcarinal, or paratracheal lymph nodes. Computed tomography (CT) scans of the chest best define the extent of nodal enlargement, the presence of necrosis, and encroachment on adjacent structures (Fig. 3). Bronchoscopy and esophagoscopy document extrinsic compression, traction diverticulae, and fistulae that are rare complications of granulomatous mediastinitis. Most patients will have resolution of this process and ultimately calcify the involved nodes.
FIG. 3.
CT scan of a young woman with granulomatous mediastinitis showing large left hilar lymphadenopathy that had persisted for over 1 year.
Mediastinal fibrosis.
Mediastinal fibrosis, or fibrosing mediastinitis, is an uncommon, but frequently lethal, complication of pulmonary histoplasmosis. Excessive fibrosis progressively envelops the structures of the mediastinum (22, 48, 78). The condition arises following infection of mediastinal lymph nodes with H. capsulatum. Most patients are young adults between the ages of 20 and 40; there is a slight predominance of women (78). The pathogenesis involves an uncontrolled fibrotic response to caseous nodes, resulting in the encasement of not only the nodes but also the vital structures of the mediastinum. Mature collagen, not granulomas, is seen on biopsy or autopsy specimens. There are no convincing data that patients with granulomatous mediastinitis go on to develop mediastinal fibrosis (78). It appears that mediastinal fibrosis occurs in a specific group of patients who, for unknown reasons, respond to infection with H. capsulatum with the production of inappropriate fibrous tissue.
The disease progresses slowly over years, gradually encroaching upon the superior vena cava, the pulmonary arteries and veins, or the bronchi. Less often, the thoracic duct, recurrent laryngeal nerve, and right atrium are involved. Symptoms include increasing dyspnea, cough, hemoptysis, and chest pain. Signs of superior vena cava syndrome or right heart failure may be prominent (82), but many patients have no abnormalities upon physical examination. Systemic signs of infection, such as fever, chills, and night sweats, are usually absent.
Chest radiographs show subcarinal or superior mediastinal widening. CT scans reveal the extent of invasion into mediastinal structures (22, 117). Angiography also helps define the constriction of the large vessels, and ventilation-perfusion lung scans reveal perfusion abnormalities caused by the constriction of pulmonary arteries. Mediastinal fibrosis that involves structures supplying both lungs is almost uniformly fatal. If only one lung is involved, patients may survive for decades with stable disease (22); however, regression of the fibrosis does not occur.
Other manifestations of pulmonary histoplasmosis.
A small proportion of patients with acute pulmonary histoplasmosis develop pericarditis as a complication of the infection. In the large outbreak of histoplasmosis in Indianapolis, pericarditis was identified in 6% of patients (137). This complication occurs predominantly in younger patients. The disease is self-limited in almost all patients, but the course can be protracted, and recurrences are common. The presentation is typical of that of acute pericarditis, with substernal chest pain and dyspnea as the prominent symptoms. Most patients have a pleural effusion, and many have mediastinal lymphadenopathy as well as pneumonia (101, 137) (Fig. 4). The pericardial and pleural fluids are exudative and frequently hemorrhagic, but tamponade is uncommon. The organism is rarely found in the fluid (167). It is thought that this manifestation occurs as a result of the host immune response to the fungus, and treatment with nonsteroidal anti-inflammatory agents relieves the symptoms. In some patients, corticosteroids may be required to dampen the immune response. Calcification of portions of the pericardium has been documented years later, but constrictive pericarditis rarely follows (101).
FIG. 4.
Pericarditis accompanying acute pulmonary histoplasmosis in a 10-year-old child. The heart shadow is increased due to a large pericardial effusion, and paratracheal lymphadenopathy is present. The child did well with treatment with nonsteroidal anti-inflammatory agents.
Pleural disease is uncommon during the course of pulmonary histoplasmosis with the exception of the exudative, culture-negative pleural effusions associated with pericarditis, as noted above (49, 101). Individual case reports have documented culture-positive effusions (111), massive pleural effusion and fibrosis associated with trapped lung (67), and the development of a bronchopleuralcutaneous fistula (55).
Broncholithiasis occurs when a calcified node adjacent to a bronchus erodes into the bronchus, causing obstruction, inflammation, and subsequent bronchial scarring. Lithoptysis, the spitting of stones, which is more often the spitting of tiny pieces of gravel-like material, can result (49, 51, 114). Cough, with or without hemoptysis, and localized wheezing can occur. The broncholith can be identified on a chest CT scan, which will also document postobstructive atelectasis and pneumonitis (51). When the calcified mass is coughed up or removed through the bronchoscope, the symptoms resolve.
Disseminated Histoplasmosis
Important to the understanding of clinical disease due to H. capsulatum is the realization that most patients infected with this organism experience asymptomatic hematogenous dissemination throughout the reticuloendothelial system via parasitized macrophages (50, 113). When T lymphocytes develop immunity to H. capsulatum antigens and activate macrophages to kill the organism, the host is able to control the infection (23, 91, 163). Even with the development of cell-mediated immunity, patients can have remaining foci of viable H. capsulatum in various organs, similar to the situation with tuberculosis. These organisms are held in check by the immune response but are not completely killed, and thus, reactivation of infection years later is possible. This has been documented to occur in patients who have not returned to the area of endemicity for many years (21, 64, 80, 109). For patients residing in areas of endemicity, it is not possible to ascertain whether disease is due to a new infection or the reactivation of an old infection.
Patient groups at risk for disseminated histoplasmosis.
The development of disease associated with the initial dissemination of H. capsulatum is dependent on the host. Patients who are immunosuppressed and are unable to develop effective cell-mediated immunity against the organism are likely to manifest symptomatic disease during the period of acute dissemination (Table 2). This includes patients with AIDS, transplant recipients, those with hematologic malignancies, and those on corticosteroids (37, 57, 64, 139, 146). Infants, presumably because of the immaturity of their cell-mediated immune system, are a special group that develops severe life-threatening infection when exposed to H. capsulatum (35, 50, 92). A person who develops an immunosuppressive condition years after leaving the area of endemicity may reactivate a focus of infection and, through that mechanism, develop severe disseminated histoplasmosis (64, 80).
TABLE 2.
Risk factors for disseminated histoplasmosis
| Risk factor |
|---|
| Age (infants) |
| AIDS |
| Hematologic malignancies |
| Solid organ transplant |
| Hematopoietic stem cell transplant |
| Immunosuppressive agents |
| Corticosteroids |
| Tumor necrosis factor antagonists |
| Congenital T-cell deficiencies |
| Gamma interferon receptor deficiency |
| Hyperimmunoglobulin M syndrome |
| Others |
AIDS has helped redefine the spectrum of illness seen with disseminated histoplasmosis (57, 146). Patients with CD4 counts of <150 cells/μl are at most risk (52, 87). In the years before highly active antiretroviral therapy became available, subclinical or symptomatic histoplasmosis occurred in 12/100 patient years in a cohort of human immunodeficiency virus-infected patients who lived in one area of endemicity (87) and in 10/1,000 patients with AIDS in another (30). Disease tends to be more severe with marked immunosuppression (17) and is often an AIDS-defining illness (52, 87). With the advent of effective antiretroviral therapy, disseminated histoplasmosis is seen much less frequently in the human immunodeficiency virus-infected population in the United States but remains a significant opportunistic infection in Central America (52).
Recently, other immunosuppressive conditions have highlighted the importance of cell-mediated immunity in the defense against disseminated histoplasmosis. The most dramatic are cases of severe histoplasmosis in patients receiving tumor necrosis factor antagonists such as etanerecept (Enbrel) and imfliximab (Remicade) (18, 162, 165). Deficiency of the gamma interferon receptor has been described as a risk factor for refractory and recurrent disseminated histoplasmosis (168), and hyperimmunoglobulin M syndrome, which has T-cell defects in addition to immunoglobulin deficiencies, has also been associated with disseminated histoplasmosis (54).
Chronic progressive disseminated histoplasmosis is a term used to describe the slowly progressive and generally fatal infection due to H. capsulatum that occurs mostly in older adults who are not overtly immunosuppressed (50, 104, 119). The majority of the cases described by Parsons and Zarafonetis in 1945 in their classic description of disseminated histoplasmosis fall into this category (97). These patients have no obvious immunosuppression, but their macrophages clearly cannot effectively kill H. capsulatum. It is thought that there is a specific defect in the cellular immune response to this specific organism (50). The time course of the infection in these patients is measured in months, and the disease is uniformly fatal if not treated. This is in contrast to the rapidly fatal acute form of dissemination that occurs in infants and immunosuppressed patients (57, 92).
Symptoms, signs, and laboratory findings with disseminated disease.
The symptoms of disseminated histoplasmosis include fever, malaise, anorexia, and weight loss. Physical examination will often show hepatosplenomegaly, lymphadenopathy, pallor and petechiae if pancytopenia is present, and, in some patients, mucous membrane ulcerations as well as skin ulcers, nodules, or molluscum-like papules (50, 104, 119). Laboratory studies reveal elevated alkaline phosphatase levels, pancytopenia, an increased Westergren sedimentation rate, elevated C-reactive protein levels, high lactate dehydrogenase levels, and increased ferritin expression, none of which are specific for disseminated histoplasmosis but all of which are highly suggestive of this diagnosis in the appropriate patient (16, 50, 68). Hypercalcemia occurs uncommonly and is similar to that described for a number of other granulomatous diseases (90). Chest radiographs may be normal or show a diffuse reticulonodular infiltrate. Many of the manifestations are similar to those of sarcoidosis; the latter diagnosis should not be considered established unless histoplasmosis is definitely excluded (144, 166).
Severe disease can present as sepsis syndrome with hypotension, disseminated intravascular coagulation, renal failure, and acute respiratory distress. This has been described mostly for infants and patients with AIDS (17, 50, 146, 154). Reactive hemophagocytic syndrome in AIDS patients with severe disseminated histoplasmosis has been described (72). Rarely, transmission across the placenta to the fetus has been described (158).
Gastrointestinal tract involvement is common during disseminated infection as determined by autopsy studies but remains asymptomatic or with only vague abdominal symptoms in many patients (50). Symptomatic infection appears to be more common in AIDS patients and can mimic other AIDS-associated opportunistic infections that cause diarrhea. Intermittent abdominal pain and tenderness are common, and severe diarrhea can lead to malabsorption (74, 93). The diagnosis of histoplasmosis is often not made until a tissue biopsy obtained by laparotomy or colonoscopy shows typical yeast forms of H. capsulatum (122). The colon is most commonly involved, followed by the small bowel; ulcerations, polypoid lesions, strictures, and perforations have been noted.
Several unique manifestations occur more frequently with histoplasmosis than with other disseminated fungal infections. This includes Addison's disease, which occurs when there is extensive destruction of both adrenal glands by the infection. The patient exhibits fever, malaise, orthostatic hypotension, nausea, and vomiting (110, 119). Hyperkalemia, hyponatremia, and eosinophilia are usually present. CT scan shows markedly enlarged adrenals, often with necrosis in the central area (160). Adrenal insufficiency was a frequent cause of death in earlier years (110). Mucous membrane lesions are also more frequently seen in disseminated histoplasmosis than in other endemic mycoses, with the exception of paracoccidioidomycosis (50, 104, 119). The tongue, gingival and buccal mucosa, lips, pharynx, and larynx can be involved. Superficial ulcerations, deeper ulcerations with heaped-up borders, nodular masses, and verrucous lesions have been noted. Although localized oral lesions in patients with no other symptoms of disseminated infection have been described (89), this is very uncommon, and mucocutaneous lesions should always be considered a manifestation of disseminated disease.
Histoplasmosis can involve every organ system during the course of dissemination, but symptomatic disease is rare at some sites. In some instances, patients have obvious systemic infection with widespread dissemination, and in other instances, focal disease in a single organ is the only manifestation of dissemination. For example, genitourinary tract involvement, although frequently documented at autopsy in patients with disseminated infection (64, 97), is rarely symptomatic. Testicular abscess, prostatic abscess, epididymitis, penile lesions, and bladder ulcerations have been reported for a few patients each (38, 65, 84, 112). The patients are often thought to have a tumor of the prostate, testes, or epididymis until a biopsy specimen reveals the typical yeast-like forms of H. capsulatum. In a few cases, immune complex glomerulonephritis with H. capsulatum antigen demonstrated in the mesangium has been described (9, 10).
Osteoarticular infection with H. capsulatum is another uncommon manifestation of histoplasmosis. Involvement can primarily involve tendons, presenting as carpal tunnel syndrome (121), or be manifest by septic arthritis of either native or prosthetic joints (20, 36) and, rarely, osteomyelitis (58). The diagnosis is generally not entertained until culture of surgical material or synovial fluid yields H. capsulatum. Sites such as gall bladder, breast, thymus, and thyroid gland are rarely infected and usually discovered only at autopsy (42, 113).
Endocarditis and vascular infection.
Histoplasma endocarditis is a rare manifestation of disseminated histoplasmosis. Infection can occur on native valves, prosthetic valves, and even atrial myxomas (3, 6, 41, 107). The patient has symptoms typical of chronic disseminated histoplasmosis and also has cardiac findings and embolic phenomena. The diagnosis is often delayed, and the patient is usually labeled as having culture-negative endocarditis. The outcome is dismal unless the diagnosis is made in a timely fashion so that effective antifungal therapy can be given (3). Infection of vascular grafts has also been described in a few cases (83).
Central nervous system infection.
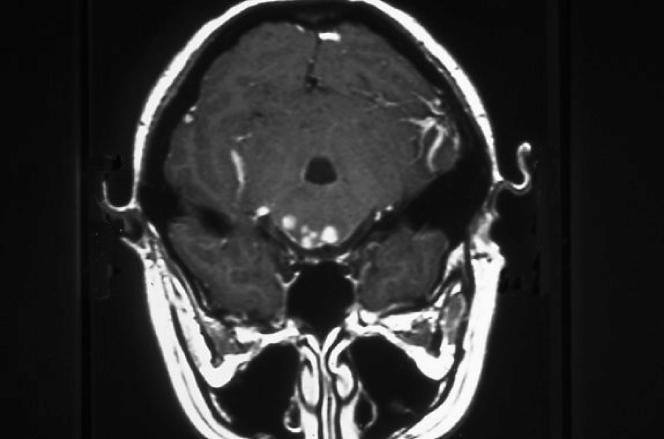
Patients can have involvement of the central nervous system (CNS) either as one manifestation of a disseminated infection or as an isolated focal infection (145, 157). CNS involvement occurs as a result of hematogenous dissemination to the meninges or brain. Chronic meningitis is the most common manifestation and is characterized by basilar meningeal involvement that can lead to communicating hydrocephalus. With the increased use of magnetic resonance imaging (MRI) scans, it has become clear that small ring-enhancing lesions can frequently be found throughout the brain and spinal cord (Fig. 5). These occur with meningitis or exist as isolated lesions without meningeal involvement. Larger, more typical brain abscesses can also be found (70).
FIG. 5.
Multiple enhancing lesions in midbrain and temporoparietal areas in a woman who had chronic Histoplasma meningitis.
Symptoms of meningitis include headache, mental status changes, and cranial nerve palsies. Behavioral changes and ataxia also can occur. Focal findings sometimes correlate with discrete lesions seen on the MRI scan but are entirely asymptomatic in other patients. The cerebrospinal fluid changes with meningitis are similar to those noted for other fungal meningitides and tuberculous meningitis. Protein is elevated, the glucose is modestly low, and white blood cells usually number between 50 and 500 cells/μl, and they are predominantly mononuclear.
DIAGNOSIS
Culture
Samples of tissue or body fluids sent to the laboratory for culture are plated onto Sabouraud's dextrose agar and incubated at 25°C to allow for growth of the mycelial phase of H. capsulatum. After several weeks, and sometimes as long as 6 weeks, growth of a white to light tan mold occurs. Two types of conidia are produced on the hyphae. The macroconidia, or tuberculate conidia, are 8 to 15 μm in diameter and have distinctive projections on their surface; the microconidia are small (2 to 4 μm) and smooth walled. Identification of the tuberculate macroconidia allows a presumptive diagnosis of histoplasmosis; however, it should be noted that fungi belonging to the genus Sepedonium also form similar tuberculate macroconidia. A definitive test to verify that the mold is H. capsulatum should always be performed. A commercially available chemiluminescent DNA probe for H. capsulatum (AccuProbe; GenProbe, Inc., San Diego, CA) is the confirmatory test most often used for definitive identification (120). This test is highly specific; false-positive tests are very rare but have been reported (7). The exoantigen test for the identification of H. capsulatum is more time-consuming and complicated and has been supplanted by the DNA probe assay (26, 66). The laborious task to convert the mold phase to the yeast phase in vitro is no longer required for the definitive identification of H. capsulatum.
For patients who have disseminated infection, samples can be taken from blood, bone marrow, liver, skin lesions, or any other site of infection. The lysis-centrifugation (Isolator tube) system has been shown to be more sensitive than automated systems for growing H. capsulatum from blood (98, 99, 161). When sputum or bronchoalveolar lavage fluid is sent for culture, a selective medium that adds ammonium hydroxide to the surface of the agar to increase the pH is very helpful; it decreases the growth of commensal fungi, thus allowing the slowly growing H. capsulatum to appear (118).
The greatest yield of culture positivity occurs in those patients who have disseminated infection, chronic cavitary pulmonary histoplasmosis, and acute pulmonary histoplasmosis following exposure to a large inoculum of the organism. For other forms of histoplasmosis, including mild to moderate acute pulmonary infection, granulomatous mediastinitis, mediastinal fibrosis, and chronic meningitis, cultures usually remain negative. Cultures usually yield no growth from cerebrospinal fluid, and the diagnosis must be made in a different manner.
Histopathology
For a patient who is acutely ill, tissue biopsy should be done as soon as possible to look for H. capsulatum. Finding the distinctive 2- to 4-μm, oval, narrow-based budding yeasts allows a tentative diagnosis of histoplasmosis (98, 113). Other organisms can mimic the appearance of H. capsulatum in tissues, but generally, the clinical picture will separate histoplasmosis from the others. Leishmania has kinetoplasts present in the small intracellular protozoa, and leishmaniasis can be differentiated clinically in most cases. Candida glabrata does not cause the same clinical syndrome as histoplasmosis. Other yeasts that cause symptoms similar to those of histoplasmosis have different appearances on histopathological examination.
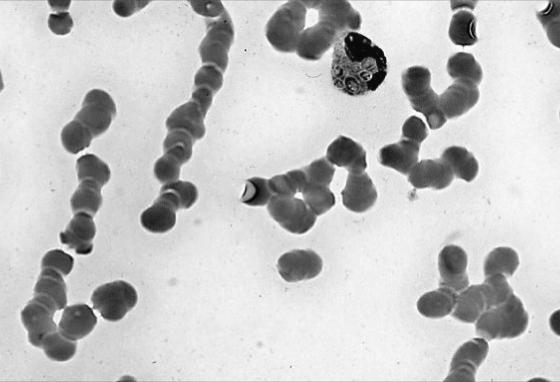
Routine hematoxylin and eosin stains generally will not allow the visualization of the tiny yeasts, although when a large number of organisms are present, one gets the impression that the macrophages are filled with something; however, the exact nature of the substance cannot be evaluated (113). Tissue should be stained with methenamine silver or periodic acid-Schiff stains to best visualize H. capsulatum. Yeasts are typically found within macrophages but can also be seen free in tissues (Fig. 6).
FIG. 6.
Typical small oval budding yeast seen in the peritoneum of a patient who had AIDS and who died of disseminated histoplasmosis.
In patients with disseminated infection, bone marrow, liver, skin, and mucocutaneous lesions usually reveal organisms. Routine peripheral blood smears will sometimes show yeasts within neutrophils in patients who are seriously ill with disseminated histoplasmosis (Fig. 7). Patients who are severely ill with diffuse pulmonary infiltrates are likely to have organisms that are apparent on a lung biopsy specimen, but those with milder disease often have no organisms seen in biopsy samples. In those with granulomatous mediastinitis, caseous material taken from necrotic nodes may contain a few yeast-like organisms typical of H. capsulatum. Biopsy of fibrotic tissue from fibrosing mediastinitis typically reveals no organisms.
FIG. 7.
Yeast forms of H. capsulatum found in a neutrophil on a peripheral blood smear.
Antigen Detection
Detection of circulating H. capsulatum polysaccharide antigen in urine and serum was first described in 1986 (142). Originally developed as a solid-phase radioimmunoassay, the assay was converted to a more easily performed sandwich enzyme immunoassay (EIA) that uses H. capsulatum polysaccharide antigen, polyclonal rabbit anti-Histoplasma immunoglobulin G conjugated to biotin, and horseradish peroxidase (31, 153). Both the initial radioimmunoassay and the current EIA are more sensitive when urine, rather than serum, is tested. This assay was initially used for patients with a variety of different manifestations of histoplasmosis (142). However, the greatest experience was obtained in AIDS patients who had disseminated histoplasmosis and who had a large burden of organisms (146, 147, 148). In this population, Histoplasma antigen was detected in urine in 95% of patients and in serum in 86% of patients (154). Fewer data are available for the use of the antigen assay in non-AIDS patients with disseminated histoplasmosis, but it appears to be a sensitive assay in this population also. Published reports note that 92% of patients have antigenuria, but only approximately 50% have antigenemia (151, 159).
In addition to patients with disseminated histoplasmosis, the antigen assay is most useful for those patients who have acute pulmonary histoplasmosis following exposure to a large number of conidia. In this group, antigenuria is detected in approximately 75% of patients within the first few weeks of illness (151). However, only 10 to 20% of patients who have less severe acute pulmonary histoplasmosis or chronic cavitary pulmonary histoplasmosis will have antigen detected in urine (151). Patients with granulomatous mediastinitis and mediastinal fibrosis generally do not have Histoplasma antigen detected in serum or urine.
There are few data on the usefulness of the Histoplasma antigen assay for bronchoalveolar lavage fluid obtained from patients with diffuse pulmonary infiltrates due to histoplasmosis (149). The 27 patients studied were all AIDS patients, and antigen was detected in 19 (70%) of those patients, a sensitivity less than that of urine, which was 93%. There have been no reported data on the usefulness of this assay on bronchoalveolar lavage fluid from non-AIDS patients. Antigen was shown to be present in cerebrospinal fluid of patients with Histoplasma meningitis by using the original radioimmunoassay (143). The sensitivity of the EIA has been reported to be from 40 to 66%, with the higher rates noted in immunosuppressed patients who presumably had a higher burden of organisms in the central nervous system (151).
False-positive reactions for Histoplasma antigen in urine are common among patients who have other endemic mycoses (Table 3). In one study, 8 of 9 patients with paracoccidioidomycosis, 12 of 19 with blastomycosis, and 17 of 18 with penicilliosis had urine antigen tests that were positive for Histoplasma antigen (133). There do not appear to be false-positive tests in patients with coccidioidomycosis. In North America, there is little concern about this lack of specificity, except for those patients who have blastomycosis, because only the areas of endemicity of histoplasmosis and blastomycosis overlap (40). Diagnosis should not be based on a urine antigen test alone; almost always, other serologic and culture data are available to confirm the diagnosis of histoplasmosis.
TABLE 3.
Causes of false-positive tests for Histoplasma antigen
| Possible cause of false-positive result |
|---|
| Urine antigen assay |
| Blastomycosis |
| Penicilliosis |
| Paracoccidioidomycosis |
| African histoplasmosis (Histoplasma capsulatum var. duboisii) |
| Serum antigen assay |
| Treatment with rabbit antithymocyte globulin |
| Rheumatoid factor |
Positive serum antigen assays but negative urine assays are exceedingly uncommon and should make one suspect a false-positive serum assay. In transplant recipients who have been given rabbit antithymocyte globulin (thymoglobulin), this scenario has occurred and has been shown to be due to the presence of human anti-rabbit antibodies that develop in response to the antithymocyte globulin. These antibodies develop by approximately week 2 after administration of the agent and are usually cleared by week 8. They cause a false-positive test result with the enzyme immunoassay for Histoplasma antigen in serum but not in urine (155).
The amount of Histoplasma antigen detected in urine can be used to monitor a patient's response to therapy (147, 148, 150, 152). Most of the reported studies were done with AIDS patients. Antigenuria should be expected to fall to below the level of detection with successful therapy (148, 150, 152). A subsequent rise in antigen levels with recrudescent infection has been noted (147). Follow-up antigen studies of non-AIDS patients have not been reported but presumably should be useful.
An inhibition EIA for the detection of Histoplasma antigens that uses a murine monoclonal antibody, rather than a polyclonal antibody, has been developed and appears to be more sensitive in serum than in urine (44, 45). However, this assay is not currently commercially available.
PCR Assays
Several laboratories are working on developing PCR assays that might help with a more rapid identification of a mold as H. capsulatum in vitro in the laboratory and in infected tissues obtained by biopsy (24, 81, 105). At this point, no PCR assay for routine use is commercially available. A real-time PCR assay that correctly identified H. capsulatum from among a variety of fungi grown in the laboratory appears promising. Using this assay, positive identification of H. capsulatum was shown in tissue biopsies and bronchoalveolar lavage fluid from three patients who had documented histoplasmosis (81). Two different seminested PCR assays have also shown promise when applied to blood and tissue scrapings obtained from patients with histoplasmosis (5, 105) and mice experimentally infected with H. capsulatum (4). The future role of PCR-based methods for the diagnosis of histoplasmosis is not yet clear.
Antibody Tests
Antibody tests play an important role in the diagnosis of several forms of histoplasmosis but are not terribly useful in others. The standard assays are the complement fixation (CF) test that uses two separate antigens, yeast and mycelial (or histoplasmin), and the immunodiffusion (ID) assay. Diagnosis is based on a fourfold rise in CF antibody titer; a single titer of ≥1:32 is suggestive but not diagnostic. CF antibodies persist for years after infection; thus, the presence of a single low CF titer means little other than that the patient was exposed to H. capsulatum at some time. The CF test appears to be less specific than the ID assay; cross-reactions occur with other fungal infections and other granulomatous processes, including tuberculosis and sarcoidosis (102, 141).
The ID assay tests for the presence of M and H precipitin bands. An M band develops with acute infection, is often present in chronic forms of histoplasmosis, and persists for months to years after the infection has resolved. An H band is much less common, is rarely, if ever, found without an M band, and is indicative of chronic or severe acute forms of histoplasmosis (2, 102). The ID assay is approximately 80% sensitive but is more specific than the CF assay. Several investigators have shown that the detection of H and M precipitating antibodies by counterimmunoelectrophoresis is more sensitive than that by immunodiffusion (69, 102, 124). However, this technique has not been commercialized, and the standard immunodiffusion assay is the only assay available. A radioimmunoassay has been described, but false-positive reactions appear to be higher than those noted with the CF assay, and standardization has not been established (138). This assay is currently not available.
Tests for antibody are most useful in patients who have chronic forms of histoplasmosis that have allowed enough time for antibody to develop and in patients who have acute pulmonary histoplasmosis, in whom documentation of a fourfold rise in antibody titer to H. capsulatum can be diagnostic. Because 2 to 6 weeks may be required for the appearance of antibodies, these assays are less useful for patients who have severe acute infection and in immunosuppressed patients, who mount a poor response (64). For those patients who have mediastinal lymphadenopathy, antibody assays may or may not be positive and cannot be relied upon to make a definitive diagnosis. Tissue biopsy is always required in these instances. False-positive CF tests occur in patients with lymphoma, tuberculosis, sarcoidosis, and other fungal infections, all of which may present as a mediastinal mass.
One unique circumstance in which the presence of antibodies may be the only assay leading to a diagnosis of histoplasmosis is in a patient who has chronic meningitis due to H. capsulatum. In this case, the presence of either CF or ID antibodies against H. capsulatum in the cerebrospinal fluid allows one to make the diagnosis of Histoplasma meningitis even when the culture shows no growth (128, 145).
Skin Tests
Historically, the histoplasmin skin test reagent was critically essential in defining the area where H. capsulatum is endemic and the unsuspected high frequency of asymptomatic infection in this area (12, 32). The skin test was not a very helpful diagnostic test because of problems with cross-reactions with other fungi, especially Blastomyces dermatitidis, interference with subsequent complement fixation antibody assays, and insensitivity in ill patients who had disseminated infection. For these reasons, the skin test reagents are no longer commercially available.
TREATMENT
Treatment Options
Treatment is not needed for most patients who have acute histoplasmosis; however, chronic forms of the infection and severe acute pulmonary histoplasmosis must be treated. Until the azole era began in the 1990s, amphotericin B deoxycholate was the only therapeutic option. Treatment options have increased considerably since then (Table 4). A series of clinical trials that established the effectiveness of amphotericin B was performed in the 1950s and 1960s by the National Communicable Disease Center (forerunner of the Centers for Disease Control and Prevention) Cooperative Mycoses Study Group and the Veterans Administration-Armed Forces Cooperative Study on Histoplasmosis (39, 96, 110, 123). In the same time period, investigators at the National Institutes of Health and the Missouri State Sanitorium reported on their experiences with treatment of disseminated histoplasmosis with amphotericin B (104, 119). Although neither controlled nor randomized, these early studies established several key points regarding the chronic cavitary pulmonary and chronic progressive disseminated forms of histoplasmosis.
TABLE 4.
Treatment options for histoplasmosis
| Agent | Description |
|---|---|
| Amphotericin B | Used for severe pulmonary or disseminated disease for a few wk until patient is improved; lipid formulations preferred, but cost is often prohibitive |
| Itraconazole | Preferred agent for mild to moderate pulmonary or disseminated disease; oral solution gives more consistent serum levels than capsules |
| Fluconazole | Second-line agent; not as efficacious as itraconazole |
| Ketoconazole | Rarely used because of toxicity |
| Voriconazole | May be effective; little clinical experience |
| Posaconazole | May be effective; little clinical experience |
| Echinocandins | Not active; should not be used |
Those studies verified earlier reports that chronic pulmonary and progressive disseminated histoplasmosis were often fatal if not treated (97). Mortality in those who had disseminated disease and who were not treated was 83%, compared with 23% in amphotericin B-treated patients (39). Similarly, Reddy et al. reported that 100% of untreated patients died, compared with 7% for those who were deemed to have received an adequate amount of amphotericin B (104). Among 100 patients with chronic cavitary pulmonary histoplasmosis who were not treated, the mortality rate was 50% at 5 years, and another 18% had progression of disease, compared with a mortality rate of 28% and progression in 15% in the group receiving amphotericin B (96).
Those studies also established an effective total dose of amphotericin B to be used for these forms of histoplasmosis. For the next 30 years, patients generally received a total dosage of 25 to 35 mg/kg amphotericin B over several months, often with resultant serious toxicity (39, 96, 104). By the time that the first Mycoses Study Group/Infectious Diseases Society of America (IDSA) guidelines for the management of histoplasmosis were published in 2000, treatment with amphotericin B for the entire course of therapy was unusual. Amphotericin B was listed as the preferred regimen only for severe disease and then only for initial therapy, with a step down to an azole agent when the patient had begun to show improvement (135).
With the introduction of ketoconazole, the hopes of treating histoplasmosis in the outpatient setting with an oral medication were finally realized. This azole was found to be effective for both disseminated and pulmonary forms of histoplasmosis; the overall success rate was 85% if the drug was taken for at least 6 months (27). Although less toxic than amphotericin B, side effects were significant, occurring in 60% of patients. At the higher dosage of 800 mg daily, interference with steroid metabolism was common, leading to gynecomastia, decreased libido, menstrual irregularities, and even hypoadrenalism (27). Ketoconazole is now rarely used for the treatment of histoplasmosis.
In the late 1980s and early 1990s, the NIAID Mycoses Study Group carried out open-label clinical trials of itraconazole for the treatment of pulmonary and disseminated histoplasmosis. The drug proved to be more effective than ketoconazole and with many fewer side effects (28). In AIDS patients who had mild to moderate disseminated histoplasmosis, itraconazole also proved to be effective therapy (130). Itraconazole has remained the drug of choice for the treatment of mild to moderate histoplasmosis for more than a decade (135).
Fluconazole is less effective than itraconazole in both patients with AIDS and those without AIDS (85, 132). Success rates of 63% for patients without AIDS (85) and 50% for those with AIDS (132) were noted. Fluconazole remains a second-line agent for the treatment of histoplasmosis.
Clinical data on the new azoles, voriconazole and posaconazole, for the treatment of histoplasmosis are limited. Both agents have activity in vitro against H. capsulatum (34, 46, 76, 127). Posaconazole has been shown to be more effective than itraconazole in both immunocompetent and immunocompromised mice infected with H. capsulatum (14, 15); voriconazole has not been tested in animal models of histoplasmosis.
Voriconazole, which is similar to fluconazole in structure, has resulted in success in the treatment of a few patients (37, 100). In one series of six transplant recipients with histoplasmosis, three were treated with voriconazole after initial therapy with other agents, and all three appeared to be cured of their infection (37). Posaconazole, which is similar to itraconazole in structure, was reported to be effective in six of seven patients, four of whom had disseminated infection and all of whom had failed or were intolerant of other therapy (104a). One of these seven patients, who had meningitis, was also later reported as having been successfully treated with posaconazole (103). One other patient who had disseminated histoplasmosis was also successfully treated with posaconazole (13). The echinocandins do not have in vitro activity against H. capsulatum and are ineffective in animal models of infection (73); they should not be used for treating histoplasmosis. Treatment options for each form of histoplasmosis are discussed below and generally reflect IDSA guidelines, which are currently undergoing revision and will be published in 2007 (135).
Acute Pulmonary Histoplasmosis
Most patients with acute pulmonary histoplasmosis recover within 4 to 6 weeks after developing symptoms and do not require treatment with an antifungal agent. Those who remain symptomatic for longer periods of time should be treated. Oral itraconazole, 200 mg once or twice daily, for 6 to 12 weeks is recommended in such cases (135).
Patients who have acute severe pulmonary histoplasmosis with diffuse reticulonodular infiltrates and hypoxemia should definitely receive antifungal therapy. When amphotericin B was the only treatment option available, these patients generally were not treated. Most patients recovered but only after many months, and some died. Current recommendations are to treat patients with severe acute pulmonary infection (135). Initial treatment should be amphotericin B, 0.7 to 1 mg/kg daily, or a lipid formulation of amphotericin B, 3 to 5 mg/kg daily, until the patient begins to show improvement; therapy can then be switched to itraconazole, 200 mg orally twice daily, for a total of approximately 3 months, depending on the clinical and radiographic response. Some patients may require therapy for as long as 6 months. Corticosteroids, given as intravenous methylprednisolone for several days or 60 mg prednisone orally daily for a week with tapering over the next 1 to 2 weeks, appear to be beneficial, but there are no controlled studies that verify this practice.
Chronic Cavitary Pulmonary Histoplasmosis
All patients with chronic pulmonary histoplasmosis should be treated with an antifungal agent. Without therapy, the disease will likely progress to respiratory insufficiency, and many patients will die (47, 96). Itraconazole, 200 mg twice daily, has supplanted amphotericin B as the therapy of choice. Most patients are chronically ill and will not require initial therapy with amphotericin B. The total length of treatment with itraconazole is 12 to 24 months, with careful follow-up for the detection of relapses.
Complications of Pulmonary Histoplasmosis
Most physicians caring for patients with granulomatous mediastinitis will offer treatment with oral itraconazole, 200 mg once or twice daily, for 6 to 12 months. This is based on the premise that there is ongoing granulomatous inflammation, and it is reasonable to expect a response to antifungal therapy. Whether such treatment is beneficial has not been proven, but there are anecdotal case reports of successful therapy with azoles (79). If the patient is severely ill with obstructive symptoms, initial treatment with amphotericin B until there is improvement, followed by itraconazole for 6 to 12 months, is recommended by IDSA guidelines (135). If there is no decrease in obstruction of mediastinal structures, surgical intervention to debulk the mass of nodes can be attempted (22).
Mediastinal fibrosis does not respond to antifungal therapy. Oral itraconazole is given out of a desire to do something, but there is no evidence that it has any positive effect. Corticosteroids and nonsteroidal anti-inflammatory agents also are not effective. Surgery has been advocated in the past, but current recommendations are to avoid surgery because the operative mortality rates are high and there has been no evidence of benefit (78, 82, 135). The most effective intervention appears to be the placement of intravascular stents in vessels that are shown to be impinged upon by the fibrosis (22, 29). This should be performed after careful review of angiograms and CT scans by an interventional radiologist who is experienced in the treatment of this disease. For vessels identified as the source of hemoptysis, angiographic embolization can be attempted.
Pericarditis associated with acute pulmonary histoplasmosis responds to treatment with nonsteroidal anti-inflammatory agents; rarely, corticosteroids may have to be used (137). Antifungal agents should not be used, because the pericarditis reflects an inflammatory reaction to H. capsulatum rather than an active infection of the pericardium. In the exceptional case associated with tamponade, pericardiocentesis and the creation of a pericardial window are important therapeutic measures (101).
Disseminated Histoplasmosis
Occasionally, patients with symptomatic disseminated histoplasmosis are able to clear the infection without antifungal therapy, but this is not typical, and in general, all patients with disseminated histoplasmosis should be treated with an antifungal agent (135). Patients who are not severely ill can be treated with oral itraconazole, 200 mg twice daily (28, 130). Most patients with chronic progressive disseminated disease will fall into this category. Fluconazole is less effective than itraconazole (85) and is considered to be a second-line agent. When fluconazole must be used, the dosage is 400 to 800 mg daily. In AIDS patients, the dosage should be 800 mg daily because of a failure rate of 50% in a cohort who had mild to moderately severe disseminated histoplasmosis and who were treated with 600 mg daily (132). In that same study, the relapse rate while patients were on maintenance fluconazole therapy was 30%, and subsequent in vitro studies with these isolates noted the development of resistance to fluconazole (132, 134).
Patients with severe disseminated infection should be treated initially with amphotericin B at a dosage of 0.7 to 1 mg/kg daily or a lipid formulation of amphotericin B at a dosage of 3 to 5 mg/kg daily. Current practice is to use lipid formulations of amphotericin B in most patients because of their reduced toxicity. A randomized, blinded, comparative trial in AIDS patients with severe disseminated histoplasmosis showed that not only was liposomal amphotericin B less toxic than standard amphotericin B deoxycholate, it also led to a more prompt resolution of fever and improved survival (56). Continuing amphotericin B throughout the entire course of therapy is no longer the standard of care. For almost all patients, as their condition improves, generally within a few weeks, their therapy is switched to oral itraconazole at a dosage of 200 mg twice daily (135).
It is not clear whether patients have better outcomes if they receive an initial few weeks of therapy with an amphotericin B formulation before itraconazole is prescribed. A retrospective analysis of the length of time that AIDS patients remained fungemic and had persistent antigenuria when treated with either itraconazole or liposomal amphotericin B showed that those patients who received liposomal amphotericin B had more rapid clearance of both fungemia and antigenuria than those who received itraconazole (150). It must be emphasized that this was not a controlled prospective analysis of these two treatment regimens; however, if anything, the results would likely be biased in favor of itraconazole because those patients were less ill.
The length of therapy depends on the severity of the infection and the immune status of the host. IDSA guidelines recommend 6 to 18 months total. This wide range emphasizes the fact that it is the immune response of the host that determines when and if azole therapy is stopped. The minimum period of treatment should be 6 months for the relatively healthy host; most patients will be treated for 12 months. Patients with chronic progressive dissemination often respond slowly, and treatment may have to continue for a total of 18 to 24 months.
Because of the high rate of relapse, it has been standard practice for AIDS patients who have histoplasmosis to be placed on maintenance azole therapy for life after their initial response to antifungal therapy (129). However, this has changed with the use of highly active antiretroviral therapy that restores CD4 cell numbers to normal or at least higher levels. Studies have shown a very low risk of relapse when CD4 counts have remained at >200 cells/μl for a year (43). The current practice is to discontinue antifungal therapy for patients achieving this level of CD4 reconstitution. For those who do not achieve immune reconstitution, maintenance therapy with 200 mg itraconazole daily should continue for life. It has also been established that prophylaxis with 200 mg itraconazole daily is effective at preventing histoplasmosis in patients with AIDS who have CD4 counts below 150 cells/μl (86). However, with the use of effective antiretroviral therapy, rates of histoplasmosis have fallen in the AIDS population, and prophylaxis is no longer recommended.
Endocarditis
Endocarditis due to H. capsulatum is best treated with amphotericin B as well as valve replacement (3, 6, 41, 61). Lipid formulations of amphotericin B, because of their lessened toxicity, are appropriate. If, for any reason, surgical extirpation of the valve cannot be performed, lifelong suppression with itraconazole should be maintained.
Central Nervous System Histoplasmosis
CNS histoplasmosis is a difficult disease to treat. Amphotericin B should be used for initial therapy in all patients. For most, this will be given as a lipid formulation, either liposomal amphotericin B or amphotericin B lipid complex, at a dosage of 3 to 5 mg/kg daily for 3 to 4 months (135, 157). Amphotericin B should be followed by an oral azole agent for an undetermined period of time. Some patients have received lifelong azole therapy, and others have had the azole stopped after 6 to 12 months (157). Repeated lumbar punctures for cerebrospinal fluid analysis should be done to determine the response to therapy and should assess Histoplasma antigen levels, white blood cell counts, and CF antibody titers. Resolution of abnormal findings should be expected and can help determine the length of therapy.
The azole of choice is not clear; fluconazole and itraconazole were both recommended as possible agents by IDSA guidelines (135). Itraconazole does not achieve adequate cerebrospinal fluid levels but has been used successfully for the treatment of cryptococcal and coccidioidal meningitis. Fluconazole achieves higher cerebrospinal fluid concentrations but is less active against H. capsulatum than itraconazole. The failure of fluconazole in a murine model of CNS histoplasmosis has been noted (53, 75). Both azoles have been used successfully for secondary treatment following induction therapy with amphotericin B (1, 70, 126). The dosage suggested for itraconazole is 200 mg twice or thrice daily, and that for fluconazole is 800 mg daily. Primary azole therapy of CNS histoplasmosis should be discouraged. Although success has been reported in a few cases, failures rates are high (71, 106, 116, 130).
Enhancing lesions in the brain or spinal cord should be treated in the same manner as meningitis. Surgical excision is not necessary. MRI scans are the appropriate test to be followed to ensure resolution. Antifungal therapy should continue for several months after all the lesions have resolved on an MRI scan (157).
REFERENCES
- 1.Bamberger, D. M. 1999. Successful treatment of multiple cerebral histoplasmomas with itraconazole. Clin. Infect. Dis. 28:915-916. [DOI] [PubMed] [Google Scholar]
- 2.Bauman, D. S., and C. D. Smith. 1975. Comparison of immunodiffusion and complement fixation tests in the diagnosis of histoplasmosis. J. Clin. Microbiol. 2:77-80. [PMC free article] [PubMed] [Google Scholar]
- 3.Bhatti, S., L. Vilenski, R. Tight, and R. A. Smego, Jr. 2004. Histoplasma endocarditis: clinical and mycologic features and outcomes. J. Infect. 51:2-9. [DOI] [PubMed] [Google Scholar]
- 4.Bialek, R., F. Ernst, K. Dietz, L. K. Najvar, J. Knobloch, J. R. Graybill, and G. Schaumburg-Lever. 2002. Comparison of staining methods and a nested PCR assay to detect Histoplasma capsulatum in tissue sections. Am. J. Clin. Pathol. 117:597-603. [DOI] [PubMed] [Google Scholar]
- 5.Bracca, A., M. E. Tosello, J. E. Girardini, S. L. Amigot, C. Gomez, and E. Serra. 2003. Molecular detection of Histoplasma capsulatum var. capsulatum in human clinical samples. J. Clin. Microbiol. 41:1753-1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bradsher, R. W., C. G. Wickre, A. M. Savage, W. E. Harston, and R. H. Alford. 1980. Histoplasma capsulatum endocarditis cured by amphotericin B combined with surgery. Chest 78:791-795. [DOI] [PubMed] [Google Scholar]
- 7.Brandt, M. E., D. Gaunt, N. Iqbal, S. McClinton, S. Hambleton, and L. Sigler. 2005. False-positive Histoplasma capsulatum Gen-Probe chemiluminescent test result caused by a Chrysosporium species. J. Clin. Microbiol. 43:1456-1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brodsky, A. L., M. B. Gregg, L. Kaufman, and G. F. Mallison. 1973. Outbreak of histoplasmosis associated with the 1970 Earth Day activities. Am. J. Med. Sci. 54:333-342. [DOI] [PubMed] [Google Scholar]
- 9.Bullock, W. E., R. P. Artz, D. Bhathena, and H. S. K. Tung. 1979. Histoplasmosis: association with circulating immune complexes, eosinophilia, and mesangiopathic glomerulonephritis. Arch. Intern. Med. 139:700-702. [DOI] [PubMed] [Google Scholar]
- 10.Burke, D. G., S. N. Emancipator, M. C. Smith, and R. A. Salata. 1997. Histoplasmosis and kidney disease in patients with AIDS. Clin. Infect. Dis. 25:281-284. [DOI] [PubMed] [Google Scholar]
- 11.Cano, M., and R. A. Hajjeh. 2001. The epidemiology of histoplasmosis: a review. Semin. Respir. Infect. 16:109-118. [DOI] [PubMed] [Google Scholar]
- 12.Christie, A., and J. C. Peterson. 1946. Histoplasmin sensitivity. J. Pediatr. 29:417-432. [DOI] [PubMed] [Google Scholar]
- 13.Clark, B., R. Foster, A. Tunbridge, and S. Green. 2005. A case of disseminated histoplasmosis successfully treated with the investigational drug posaconazole. J. Infect. 51:177-180. [DOI] [PubMed] [Google Scholar]
- 14.Connolly, P. J., J. Wheat, C. Schnizlein-Bick, M. Durkin, S. Kohler, M. Smedema, J. Goldberg, E. Brizendine, and D. Loebenberg. 1999. Comparison of a new triazole antifungal agent, Schering 56592, with itraconazole and amphotericin B for treatment of histoplasmosis in immunocompetent mice. Antimicrob. Agents Chemother. 43:322-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Connolly, P. J., L. J. Wheat, C. Schnizlein-Bick, M. Durkin, S. Kohler, M. Smedema, J. Goldberg, E. Brizendine, and D. Loebenberg. 2000. Comparison of a new triazole, posaconazole, with itraconazole and amphotericin B for treatment of histoplasmosis following pulmonary challenge in immunocompromised mice. Antimicrob. Agents Chemother. 44:2604-2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Corcoran, G. R., H. Al-Abdely, C. D. Flanders, J. Geimer, and T. F. Patterson. 1997. Markedly elevated serum lactate dehydrogenase levels are a clue to the diagnosis of disseminated histoplasmosis in patients with AIDS. Clin. Infect. Dis. 24:942-944. [DOI] [PubMed] [Google Scholar]
- 17.Couppie, P., M. Sobesky, C Aznar, S. Bichat, E. Clyti, F. Bissuel, M. El Guedj, F. Alvarez, M. Demar, D. Louvel, R. Pradinaud, and B. Carme. 2004. Histoplasmosis and acquired immunodeficiency syndrome: a study of prognostic factors. Clin. Infect. Dis. 38:134-138. [DOI] [PubMed] [Google Scholar]
- 18.Crum, N. F., E. R. Lederman, and M. R. Wallace. 2005. Infections associated with tumor necrosis factor-alpha antagonists. Medicine (Baltimore) 84:291-302. [DOI] [PubMed] [Google Scholar]
- 19.Darling, S. T. 1906. A protozoan general infection producing pseudotubercles in the lungs and focal necroses in the liver, spleen, and lymph nodes. JAMA 46:1283-1285. [Google Scholar]
- 20.Darouiche, R. O., R. M. Cadle, G. J. Zenon, M. F. Weinert, R. J. Hamill, and M. D. Lidsky. 1992. Articular histoplasmosis. J. Rheumatol. 19:1991-1993. [PubMed] [Google Scholar]
- 21.Davies, S. F., M. Khan, and G. A. Sarosi. 1978. Disseminated histoplasmosis in immunologically suppressed patients. Am. J. Med. 64:94-100. [DOI] [PubMed] [Google Scholar]
- 22.Davis, A., D. Pierson, and J. E. Loyd. 2001. Mediastinal fibrosis. Semin. Respir. Infect. 16:119-130. [DOI] [PubMed] [Google Scholar]
- 23.Deepe, G. S., Jr. 1988. Protective immunity in murine histoplasmosis: functional comparison of adoptively transferred T-cell clones and splenic T cells. Infect. Immun. 56:2350-2355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Matos Guedes, H. L., A. J. Guimarães, M. M. Muniz, C. V. Pizzini, A. J. Hamilton, J. M. Peralta, G. S. Deepe, Jr., and R. M. Zancopé-Oliveira. 2003. PCR assay for identification of Histoplasma capsulatum based on the nucleotide sequence of the M antigen. J. Clin. Microbiol. 41:535-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.De Monbreun, W. A. 1934. Cultivation and cultural characteristics of Darling's Histoplasma capsulatum. Am. J. Trop. Med. 14:93-125. [Google Scholar]
- 26.DiSalvo, A. F., A. S. Sekhon, G. A. Land, and W. H. Fleming. 1980. Evaluation of the exoantigen test for identification of Histoplasma species and Coccidioides immitis cultures. J. Clin. Microbiol. 11:238-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dismukes, W. E., G. Cloud, C. Bowles, and the NIAID Mycoses Study Group. 1985. Treatment of blastomycosis and histoplasmosis with ketoconazole: results of a prospective randomized clinical trial. Ann. Intern. Med. 103:861-872. [PubMed] [Google Scholar]
- 28.Dismukes, W. E., R. W. Bradsher, Jr., G. C. Cloud, C. A. Kauffman, S. W. Chapman, R. B. George, D. A. Stevens, W. M. Girard, M. S. Saag, C. Bowles-Patton, and the NIAID Mycoses Study Group. 1992. Itraconazole therapy for blastomycosis and histoplasmosis. Am. J. Med. 93:489-497. [DOI] [PubMed] [Google Scholar]
- 29.Doyle, T. P., J. E. Loyd, and I. M. Robbins. 2001. Percutaneous pulmonary artery and vein stenting: a novel treatment for mediastinal fibrosis. Am. J. Respir. Crit. Care Med. 164:657-660. [DOI] [PubMed] [Google Scholar]
- 30.Dupont, B., H. H. C. Brown, K. Westermann, M. D. Martins, J. H. Rex, O. Lortholary, and C. A. Kauffman. 2000. Mycoses in AIDS. Med. Mycol. 38(Suppl. 1):259-268. [PubMed] [Google Scholar]
- 31.Durkin, M. M., P. A. Connolly, and L. J. Wheat. 1997. Comparison of radioimmunoassay and enzyme-linked immunoassay methods for detection of Histoplasma capsulatum var. capsulatum antigen. J. Clin. Microbiol. 35:2252-2255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Edwards, L. B., S. A. Acquaviva, V. T. Livesay, F. W. Cross, and C. E. Palmer. 1969. An atlas of sensitivity to tuberculin, PPD-B, and histoplasmin in the United States. Annu. Rev. Respir. Dis. 99:1-18. [PubMed] [Google Scholar]
- 33.Emmons, C. W. 1949. Isolation of Histoplasma capsulatum from soil. Public Health Rep. 64:892-896. [PubMed] [Google Scholar]
- 34.Espinel-Ingroff, A. 1998. Comparison of in vitro activities of the new triazole SCH56592 and the echinocandins MK-0991 [L-743,872] and LY303366 against opportunistic filamentous and dimorphic fungi and yeasts. J. Clin. Microbiol. 36:2950-2956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fosson, A. R., and W. E. Wheeler. 1975. Short-term amphotericin B treatment of severe childhood histoplasmosis. J. Pediatr. 86:32-36. [DOI] [PubMed] [Google Scholar]
- 36.Fowler, V. G., Jr., F. M. Nacinovich, J. A. Alspaugh, and G. R. Corey. 1998. Prosthetic joint infection due to Histoplasma capsulatum: case report and review. Clin. Infect. Dis. 26:1017. [DOI] [PubMed] [Google Scholar]
- 37.Freifeld, A. G., P. C. Iwen, B. L. Lesiak, R. K. Gilroy, R. B. Stevens, and A. C. Kalil. 2005. Histoplasmosis in solid organ transplant recipients at a large Midwestern university transplant center. Transpl. Infect. Dis. 7:109-115. [DOI] [PubMed] [Google Scholar]
- 38.Friskel, E., S. A. Klotz, W. Bartholomew, and A. Dixon. 2000. Two unusual presentations of urogenital histoplasmosis and a review of the literature. Clin. Infect. Dis. 31:189-191. [DOI] [PubMed] [Google Scholar]
- 39.Furcolow, M. L. 1963. Comparison of treated and untreated severe histoplasmosis. JAMA 183:121-127.13994290 [Google Scholar]
- 40.Garner, J. A., and D. Kernodle. 1995. False-positive Histoplasma antigen test in a patient with pulmonary blastomycosis. Clin. Infect. Dis. 21:1054. [DOI] [PubMed] [Google Scholar]
- 41.Gaynes, R. P., P. Gardner, and W. Causey. 1981. Prosthetic value endocarditis caused by Histoplasma capsulatum. Arch. Intern. Med. 141:1533-1537. [PubMed] [Google Scholar]
- 42.Goldani, L. Z., C. Klock, A. Diehl, A. C. Monteiro, and A. L. Maia. 2000. Histoplasmosis of the thyroid. J. Clin. Microbiol. 38:3890-3891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Goldman, M., R. Zackin, C. J. Fichtenbaum, D. K. Skiest, S. L. Koletar, R. Hafner, L. J. Wheat, P. M. Nyangweso, C. T. Yiannoutsos, C. T. Schnizlein-Bick, S. Owens, J. A. Aberg, and the AIDS Clinical Trial Group A5038 Study Group. 2004. Safety of discontinuation of maintenance therapy for disseminated histoplasmosis after immunologic response to antiretroviral therapy. Clin. Infect. Dis. 38:1485-1489. [DOI] [PubMed] [Google Scholar]
- 44.Gomez, B. L., J. I. Figueroa, A. J. Hamilton, B. L. Ortiz, M. A. Robledo, A. Restrepo, and R. J. Hay. 1997. Development of a novel antigen detection test for histoplasmosis. J. Clin. Microbiol. 35:2618-2622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gomez, B. L., J. I. Figueroa, A. J. Hamilton, S. Diez, M. Rojas, A. Tobon, A. Restrepo, and R. J. Hay. 1999. Detection of the 70-kilodalton Histoplasma capsulatum antigen in serum of histoplasmosis patients: correlation between antigenemia and therapy during follow-up. J. Clin. Microbiol. 37:675-680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gonzalez, G. M., A. W. Fothergill, D. A. Sutton, and M. G. Rinaldi. 2005. In vitro activities of new and established triazoles against opportunistic and dimorphic fungi. Med. Mycol. 43:281-284. [DOI] [PubMed] [Google Scholar]
- 47.Goodwin, R. A., Jr., F. T. Owens, J. D. Snell, W. W. Hubbard, R. D. Buchanan, R. T. Terry, and R. M. des Prez. 1976. Chronic pulmonary histoplasmosis. Medicine (Baltimore) 55:413-452. [DOI] [PubMed] [Google Scholar]
- 48.Goodwin, R. A., Jr., J. A. Nickell, and R. M. des Prez. 1972. Mediastinal fibrosis complicating healed primary histoplasmosis and tuberculosis. Medicine (Baltimore) 51:227-246. [DOI] [PubMed] [Google Scholar]
- 49.Goodwin, R. A., Jr., J. E. Loyd, and R. M. des Prez. 1981. Histoplasmosis in normal hosts. Medicine (Baltimore) 60:231-266. [DOI] [PubMed] [Google Scholar]
- 50.Goodwin, R. A., Jr., J. L. Shapiro, G. H. Thurman, S. S. Thurman, and R. M. des Prez. 1980. Disseminated histoplasmosis: clinical and pathological correlations. Medicine (Baltimore) 59:1-33. [PubMed] [Google Scholar]
- 51.Gurney, J. W., and D. J. Conces, Jr. 1996. Pulmonary histoplasmosis. Radiology 199:297-306. [DOI] [PubMed] [Google Scholar]
- 52.Gutierrez, M. E., A. Canton, N. Sosa, E. Puga, and L. Talavera. 2005. Disseminated histoplasmosis in patients with AIDS in Panama: a review of 104 cases. Clin. Infect. Dis. 40:1199-1202. [DOI] [PubMed] [Google Scholar]
- 53.Haynes, R. R., P. A. Connolly, M. M. Durkin, A. M. LeMonte, M. L. Smedema, E. Brizendine, and L. J. Wheat. 2002. Antifungal therapy for central nervous system histoplasmosis, using a newly developed intracranial model of infection. J. Infect. Dis. 185:1830-1832. [DOI] [PubMed] [Google Scholar]
- 54.Hofstoffer, R. W., M. Berger, H. T. Clark, and J. Schreiber. 1994. Disseminated Histoplasma capsulatum in a patient with hyper IgM immunodeficiency. Pediatrics 94:234-236. [PubMed] [Google Scholar]
- 55.Johns, L. E., R. G. Garrison, and T. G. White. 1973. Bronchopleuralcutaneous fistula due to infection with Histoplasma capsulatum. Chest 63:638-641. [DOI] [PubMed] [Google Scholar]
- 56.Johnson, P. C., L. J. Wheat, G. A. Cloud, M. Goldman, D. Lancaster, D. M. Bamberger, W. G. Powderly, R. Hafner, C. A. Kauffman, W. E. Dismukes, and the NIAID Mycoses Study Group. 2002. Safety and efficacy of liposomal amphotericin B compared with conventional amphotericin B for induction therapy of histoplasmosis in patients with AIDS. Ann. Intern. Med. 137:105-109. [DOI] [PubMed] [Google Scholar]
- 57.Johnson, P. C., N. Khardori, A. F. Najjar, F. Butt, P. W. A. Mansell, and G. A. Sarosi. 1988. Progressive disseminated histoplasmosis in patients with the acquired immunodeficiency syndrome. Am. J. Med. 85:152-158. [DOI] [PubMed] [Google Scholar]
- 58.Jones, R. C., and R. A. Goodwin. 1981. Histoplasmosis of bone. Am. J. Med. 70:864-866. [DOI] [PubMed] [Google Scholar]
- 59.Jones, T. F., G. L. Swinger, A. S. Craig, M. M. McNeil, L. Kaufman, and W. Schaffner. 1999. Acute pulmonary histoplasmosis in bridge workers: a persistent problem. Am. J. Med. 106:480-482. [DOI] [PubMed] [Google Scholar]
- 60.Judson, M. A. 2004. Noninvasive Aspergillus pulmonary disease. Semin. Respir. Crit. Care Med. 25:203-219. [DOI] [PubMed] [Google Scholar]
- 61.Kanawaty, D. S., M. J. B. Stalker, and P. W. Munt. 1991. Nonsurgical treatment of Histoplasma endocarditis involving a bioprosthetic valve. Chest 99:253-256. [DOI] [PubMed] [Google Scholar]
- 62.Kataria, Y. P., P. B. Campbell, and B. T. Burlingham. 1981. Acute pulmonary histoplasmosis presenting as adult respiratory distress syndrome: Effect of therapy on clinical and laboratory features. South. Med. J. 74:534-537. [DOI] [PubMed] [Google Scholar]
- 63.Kauffman, C. A. 2003. Histoplasmosis, p. 285-298. In W. E. Dismukes, P. G. Pappas, and J. D. Sobel (ed.), Clinical mycology. Oxford University Press, New York, NY.
- 64.Kauffman, C. A., K. S. Israel, J. W. Smith, A. C. White, J. Schwarz, and G. F. Brooks. 1978. Histoplasmosis in immunosuppressed patients. Am. J. Med. 64:923-932. [DOI] [PubMed] [Google Scholar]
- 65.Kauffman, C. A., T. G. Slama, and L. J. Wheat. 1981. Histoplasma capsulatum epididymitis. J. Urol. 125:434-435. [DOI] [PubMed] [Google Scholar]
- 66.Kaufman, L., and P. Standard. 1978. Improved version of the exoantigen test for identification of Coccidioides immitis and Histoplasma capsulatum cultures. J. Clin. Microbiol. 8:42-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kilburn, C. D., and D. S. McKinsey. 1991. Recurrent massive pleural effusion due to pleural, pericardial, and epicardial fibrosis in histoplasmosis. Chest 100:1715-1717. [DOI] [PubMed] [Google Scholar]
- 68.Kirn, D. H., D. Fredericks, J. A. McCutchan, D. Stites, and M. Shuman. 1995. Serum ferritin levels correlate with disease activity in patients with AIDS and disseminated histoplasmosis. Clin. Infect. Dis. 21:1048-1049. [DOI] [PubMed] [Google Scholar]
- 69.Kleger, B., and L. Kaufman. 1973. Detection and identification of diagnostic Histoplasma capsulatum precipitates by counterelectrophoresis. Appl. Microbiol. 26:231-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Klein, C. J., R. P. Dinapoli, Z. Temesgen, and F. B. Meyer. 1999. Central nervous system histoplasmosis mimicking a brain tumor: difficulties in diagnosis and treatment. Mayo Clin. Proc. 74:803-807. [DOI] [PubMed] [Google Scholar]
- 71.Knapp, S., M. Turnherr, G. Dekan, B. Willinger, G. Stingl, and A. Rieger. 1999. A case of HIV-associated histoplasmosis successfully treated with fluconazole. Eur. J. Clin. Microbiol. Infect. Dis. 18:658-661. [DOI] [PubMed] [Google Scholar]
- 72.Koduri, P. R., V. Chindi, P. DeMarais, B. A. Mizock, A. R. Patel, and R. A. Weinstein. 1995. Reactive hemophagocytic syndrome: a new presentation of disseminated histoplasmosis in patients with AIDS. Clin. Infect. Dis. 21:1463-1465. [DOI] [PubMed] [Google Scholar]
- 73.Kohler, S., L. J. Wheat, P. Connolly, C. Schnizlein-Bick, M. Durkin, M. Smedema, J. Goldberg, and E. Brizendine. 2000. Comparison of the echinocandin caspofungin with amphotericin B for treatment of histoplasmosis following pulmonary challenge in a murine model. Antimicrob. Agents Chemother. 44:1850-1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lamps, L. W., C. P. Molina, A. B. West, R. C. Haggit, and M. A. Scott. 2000. The pathological spectrum of gastrointestinal and hepatic histoplasmosis. Am. J. Clin. Pathol. 113:64-72. [DOI] [PubMed] [Google Scholar]
- 75.LeMonte, A., K. Washum, M. Smedema, C. Schnizlein-Bick, R. Kohler, and L. J. Wheat. 2000. Amphotericin B combined with itraconazole or fluconazole for treatment of histoplasmosis. J. Infect. Dis. 182:545-550. [DOI] [PubMed] [Google Scholar]
- 76.Li, R. K., M. A. Ciblak, N. Nordoff, L. Pasarell, D. W. Warnock, and M. R. McGinnis. 2000. In vitro activities of voriconazole, itraconazole, and amphotericin B against Blastomyces dermatitidis, Coccidioides immitis, and Histoplasma capsulatum. Antimicrob. Agents Chemother. 44:1734-1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lottenberg, O., R. H. Waldman, L. Ajello, G. L. Hoff, W. Bigler, and S. R. Zellner. 1979. Pulmonary histoplasmosis associated with exploration of a bat cave. Am. J. Epidemiol. 110:156-161. [DOI] [PubMed] [Google Scholar]
- 78.Loyd, J. E., B. F. Tillman, J. B. Atkinson, and R. M. des Prez. 1988. Mediastinal fibrosis complicating histoplasmosis. Medicine (Baltimore) 67:295-310. [DOI] [PubMed] [Google Scholar]
- 79.Maholtz, M. S., J. H. Dauber, and S. A. Yousem. 1994. Fluconazole therapy in Histoplasma mediastinal granuloma. Am. J. Med. Sci. 307:274-277. [DOI] [PubMed] [Google Scholar]
- 80.Mandell, W., D. M. Goldberg, and H. C. Neu. 1986. Histoplasmosis in patients with the acquired immune deficiency syndrome. Am. J. Med. 81:974-978. [DOI] [PubMed] [Google Scholar]
- 81.Martagon-Villamil, J., N. Shrestha, M. Sholtis, C. M. Isada, G. S. Hall, T. Byrne, B. A. Lodge, L. B. Reller, and G. W. Procop. 2003. Identification of Histoplasma capsulatum from culture extracts by real-time PCR. J. Clin. Microbiol. 41:1295-1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mathisen, D. J., and H. C. Grillo. 1992. Clinical manifestations of mediastinal fibrosis and histoplasmosis. Ann. Thorac. Surg. 54:1053-1058. [DOI] [PubMed] [Google Scholar]
- 83.Matthay, R. A., D. C. Levin, A. B. Wicks, and J. H. Ellis, Jr. 1976. Disseminated histoplasmosis involving an aortofemoral graft. JAMA 235:1478-1479. [PubMed] [Google Scholar]
- 84.Mawhorter, S. D., G. V. Curley, E. D. Kursh, and C. E. Farver. 2000. Prostatic and central nervous system histoplasmosis in an immunocompetent host: case report and review of the prostatic histoplasmosis literature. Clin. Infect. Dis. 30:595-598. [DOI] [PubMed] [Google Scholar]
- 85.McKinsey, D. S., C. A. Kauffman, P. G. Pappas, G. A. Cloud, W. M. Girard, P. K. Sharkey, R. J. Hamill, C. J. Thomas, W. E. Dismukes, and the NIAID Mycoses Study Group. 1996. Fluconazole therapy for histoplasmosis. Clin. Infect. Dis. 23:996-1001. [DOI] [PubMed] [Google Scholar]
- 86.McKinsey, D. S., L. J. Wheat, G. A. Cloud, M. Pierce, J. R. Black, D. M. Bamberger, M. Goldman, C. J. Thomas, H. M. Gutsch, B. Moskovitz, W. E. Dismukes, C. A. Kauffman, and the NIAID Mycoses Study Group. 1999. Itraconazole prophylaxis for fungal infections in patients with advanced human immunodeficiency virus infection: randomized, placebo-controlled, double-blind study. Clin. Infect. Dis. 28:1049-1056. [DOI] [PubMed] [Google Scholar]
- 87.McKinsey, D. S., R. A. Spiegel, L. Hutwanger, J. Stanford, M. R. Driks, J. Brewer, M. R. Gupta, D. L. Smith, M. C. O'Connor, and L. Dall. 1997. Prospective study of histoplasmosis in patients infected with human immunodeficiency virus: incidence, risk factors, and pathophysiology. Clin. Infect. Dis. 24:1195-1203. [DOI] [PubMed] [Google Scholar]
- 88.Medeiros, A. A., S. D. Marty, F. E. Tosh, and T. D. Y. Chin. 1966. Erythema nodosum and erythema multiforme as clinical manifestations of histoplasmosis in a community outbreak. N. Engl. J. Med. 274:415-420. [DOI] [PubMed] [Google Scholar]
- 89.Mignogna, M. D., S. Fedele, L. Lo Russo, E. Ruoppo, and L. Lo Muzio. 2001. A case of oral localized histoplasmosis in an immunocompetent patient. J. Clin. Microbiol. Infect. Dis. 20:753-755. [DOI] [PubMed] [Google Scholar]
- 90.Murray, J. J., and C. R. Heim. 1985. Hypercalcemia in disseminated histoplasmosis. aggravation by vitamin D. Am. J. Med. 78:881-884. [DOI] [PubMed] [Google Scholar]
- 91.Newman, S. L. 2001. Cell-mediated immunity to Histoplasma capsulatum. Semin. Respir. Infect. 16:102-108. [DOI] [PubMed] [Google Scholar]
- 92.Odio, C. M., M. Navarrete, J. M. Carrillo, L. Mora, and A. Carranza. 1999. Disseminated histoplasmosis. Pediatr. Infect. Dis. J. 18:1065-1068. [DOI] [PubMed] [Google Scholar]
- 93.Orchard, J. L., F. Luparello, and D. Brunskill. 1979. Malabsorption syndrome occurring in the course of disseminated histoplasmosis. Am. J. Med. 66:331-336. [DOI] [PubMed] [Google Scholar]
- 94.Ozols, I. I., and L. J. Wheat. 1981. Erythema nodosum in an epidemic of histoplasmosis in Indianapolis, Indiana. Arch. Dermatol. 117:709-712. [PubMed] [Google Scholar]
- 95.Palmer, C. E. 1945. Non-tuberculous pulmonary calcification and sensitivity to histoplasmin. Public Health Rep. 60:513-520. [Google Scholar]
- 96.Parker, J. D., G. A. Sarosi, I. L. Doto, R. E. Bailey, and F. E. Tosh. 1970. Treatment of chronic pulmonary histoplasmosis. N. Engl. J. Med. 283:225-229. [DOI] [PubMed] [Google Scholar]
- 97.Parsons, R. J., and C. J. D. Zarafonetis. 1945. Histoplasmosis in man, report of seven cases and a review of seventy-one cases. Arch. Intern. Med. 75:1-23. [Google Scholar]
- 98.Paya, C. V., G. D. Roberts, and F. R. Cockerill III. 1987. Laboratory methods for the diagnosis of disseminated histoplasmosis: clinical importance of the lysis-centrifugation blood culture technique. Mayo Clin. Proc. 62:480-485. [DOI] [PubMed] [Google Scholar]
- 99.Paya, C. V., G. D. Roberts, and F. R. Cockerill III. 1987. Transient fungemia in acute pulmonary histoplasmosis: detection by new blood-culturing techniques. J. Infect. Dis. 156:313-315. [DOI] [PubMed] [Google Scholar]
- 100.Perfect, J. R., K. A. Marr, T. J. Walsh, R. N. Greenberg, B. Dupont, J. de la Torre-Cisneros, G. Just-Nubling, H. T. Schlamm, I. Lutsar, A. Espinel-Ingroff, and E. Johnson. 2003. Voriconazole treatment for less-common, emerging, or refractory fungal infections. Clin. Infect. Dis. 36:1122-1131. [DOI] [PubMed] [Google Scholar]
- 101.Picardi, J. L., C. A. Kauffman, J. Schwarz, J. C. Holmes, J. P. Phair, and N. O. Fowler. 1976. Pericarditis caused by Histoplasma capsulatum. Am. J. Cardiol. 37:82-88. [DOI] [PubMed] [Google Scholar]
- 102.Picardi, J. L., C. A. Kauffman, J. Schwarz, and J. P. Phair. 1976. Detection of precipitating antibodies to Histoplasma capsulatum by counterimmunoelectrophoresis. Am. Rev. Respir. Dis. 114:171-176. [DOI] [PubMed] [Google Scholar]
- 103.Pitisuttithum, P., R. Negroni, J. R. Graybill, B. Bustamante, P. Pappas, S. Chapman, R. S. Hare, and C. J. Hardalo. 2005. Activity of posaconazole in the treatment of central nervous system fungal infections. J. Antimicrob. Chemother. 56:745-755. [DOI] [PubMed] [Google Scholar]
- 104.Reddy, P., D. F. Gorelick, C. A. Brasher, and H. Larsh. 1970. Progressive disseminated histoplasmosis as seen in adults. Am. J. Med. 48:629-636. [DOI] [PubMed] [Google Scholar]
- 104a.Restrepo, A., B. Clark, D. R. Graham, S. Greene, R. Hare, G. Corcoran, C. Hardalo, T. Moore, R. Negroni, and J. Graybill. 7 July 2006, posting date. Salvage treatment of histoplasmosis with posaconazole. J. Infect. doi: 10.1016/j.jinf.2006.05.006. [DOI] [PubMed]
- 105.Rickets, V., R. Bialek, K. Tintlenot, V. Jacobi, and G. Just-Nubling. 2002. Rapid PCR-based diagnosis of disseminated histoplasmosis in an AIDS patient. Eur. J. Clin. Microbiol. Infect. Dis. 21:821-823. [DOI] [PubMed] [Google Scholar]
- 106.Rivera, I., R. Curless, F. Indacochea, and G. Scott. 1992. Chronic progressive CNS histoplasmosis presenting in childhood: response to fluconazole therapy. Pediatr. Neurol. 8:151-153. [DOI] [PubMed] [Google Scholar]
- 107.Rogers, E. W., A. E. Weyman, R. J. Noble, and S. C. Bruins. 1978. Left atrial myxoma infected with Histoplasma capsulatum. Am. J. Med. 64:683-690. [DOI] [PubMed] [Google Scholar]
- 108.Rosenthal, J., K. D. Brandt, L. J. Wheat, and T. G. Slama. 1983. Rheumatologic manifestations of histoplasmosis in the recent Indianapolis epidemic. Arthritis Rheum. 26:1065-1070. [DOI] [PubMed] [Google Scholar]
- 109.Saidinejad, M., M. M. Burns, and M. B. Harper. 2004. Disseminated histoplasmosis in a nonendemic area. Pediatr. Infect. Dis. J. 23:781-782. [DOI] [PubMed] [Google Scholar]
- 110.Sarosi, G. A., D. W. Voth, B. A. Dahl, I. L. Doto, and F. E. Tosh. 1971. Disseminated histoplasmosis: results of long-term follow-up. Ann. Intern. Med. 75:511-516. [DOI] [PubMed] [Google Scholar]
- 111.Schub, H. M., C. G. Spivey, and G. D. Baird. 1966. Pleural involvement in histoplasmosis. Am. Rev. Respir. Dis. 94:225-232. [DOI] [PubMed] [Google Scholar]
- 112.Schuster, T. G., B. K. Hollenbeck, C. A. Kauffman, S. W. Chensue, and J. T. Wei. 2000. Testicular histoplasmosis. J. Urol. 164:1652. [PubMed] [Google Scholar]
- 113.Schwarz, J. 1981. Histoplasmosis. Praeger Publishers, New York, NY.
- 114.Schwarz, J., M. D. Schaen, and J. L. Picardi. 1976. Complications of the arrested primary histoplasmic complex. JAMA 236:1157-1161. [DOI] [PubMed] [Google Scholar]
- 115.Sellers, T. F., W. N. Price, and W. M. Newberry. 1965. An epidemic of erythema multiforme and erythema nodosum caused by histoplasmosis. Ann. Intern. Med. 62:1244-1262. [DOI] [PubMed] [Google Scholar]
- 116.Sharkey-Mathis, P. K., J. Velez, R. Fetchick, and J. R. Graybill. 1993. Histoplasmosis in the acquired immunodeficiency syndrome (AIDS): treatment with itraconazole and fluconazole. J. Acquir. Immune Defic. Syndr. 6:809-819. [PubMed] [Google Scholar]
- 117.Sherrick, A. D., L. R. Brown, G. F. Harms, and J. L. Myers. 1994. The radiographic findings of fibrosing mediastinitis. Chest 106:484-489. [DOI] [PubMed] [Google Scholar]
- 118.Smith, C. D., and N. L. Goodman. 1975. Improved culture method for the isolation of Histoplasma capsulatum and Blastomyces dermatitidis from contaminated specimens. Am. J. Clin. Pathol. 63:276-280. [DOI] [PubMed] [Google Scholar]
- 119.Smith, J. W., and J. P. Utz. 1972. Progressive disseminated histoplasmosis, a prospective study of 26 patients. Ann. Intern. Med. 76:557-565. [DOI] [PubMed] [Google Scholar]
- 120.Stockman, L., K. A. Clark, J. M. Hunt, and G. D. Roberts. 1993. Evaluation of commercially available acridinium ester-labeled chemiluminescent DNA probes for culture identification of Blastomyces dermatitidis, Coccidioides immitis, Cryptococcus neoformans, and Histoplasma capsulatum. J. Clin. Microbiol. 31:845-850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Strayer, D. S., M. B. Gutwein, D. Herbold, and R. Bresalier. 1981. Histoplasmosis presenting as the carpal tunnel syndrome. Am. J. Surg. 141:286-288. [DOI] [PubMed] [Google Scholar]
- 122.Suh, K. N., T. Anekthananon, and P. R. Mariuz. 2001. Gastrointestinal histoplasmosis in patients with AIDS: case report and review. 32:483-491. [DOI] [PubMed]
- 123.Sutliff, W. D., C. E. Andrews, E. Jones, R. T. Terry, et al. 1964. Histoplasmosis cooperative study. Am. Rev. Respir. Dis. 89:641-650.14145215 [Google Scholar]
- 124.Sweet, G. H., R. S. Cimprich, A. C. Cook, and D. E. Sweet. 1979. Antibodies in histoplasmosis detected by use of yeast and mycelial antigens in immunodiffusion and electroimmunodiffusion. Am. Rev. Respir. Dis. 120:441-448. [DOI] [PubMed] [Google Scholar]
- 125.Thornberry, D. K., L. J. Wheat, K. Brandt, and J. Rosenthal. 1982. Histoplasmosis presenting with joint pain and hilar adenopathy: “pseudosarcoidosis.” Arthritis Rheum. 25:1396-1402. [DOI] [PubMed] [Google Scholar]
- 126.Tiraboschi, I., I. Casas Parera, R. Pikielny, G. Scattini, and F. Micheli. 1992. Chronic Histoplasma capsulatum infection of the central nervous system successfully treated with fluconazole. Eur. Neurol. 32:70-73. [DOI] [PubMed] [Google Scholar]
- 127.Torres, H. A., R. Y. Hachem, R. F. Chemaly, D. P. Kontoyiannis, and I. I. Raad. 2005. Posaconazole: a broad-spectrum triazole antifungal. Lancet Infect. Dis. 5:775-785. [DOI] [PubMed] [Google Scholar]
- 128.Wheat, J., M. French, B. Batteiger, and R. Kohler. 1985. Cerebrospinal fluid Histoplasma antibodies in central nervous system histoplasmosis. Arch. Intern. Med. 145:1237-1240. [PubMed] [Google Scholar]
- 129.Wheat, J., R. Hafner, M. Wulfson, P. Spencer, K. Squires, W. Powderly, B. Wong, M. Rinaldi, M. Saag, R. Hamill, R. Murphy, P. Connolly-Stringfield, N. Briggs, S. Owens, et al. 1993. Prevention of relapse of histoplasmosis with itraconazole in patients with the acquired immunodeficiency syndrome. Ann. Intern. Med. 118:610-616. [DOI] [PubMed] [Google Scholar]
- 130.Wheat, J., R. Hafner, A. H. Korzun, M. T. Limjoco, P. Spencer, R. A. Larsen, G. F. M. Hecht, W. Powderly, and the AIDS Clinical Trial Group. 1995. Itraconazole treatment of disseminated histoplasmosis in patients with the acquired immunodeficiency syndrome. Am. J. Med. 98:336-342. [DOI] [PubMed] [Google Scholar]
- 131.Wheat, J. 1997. Histoplasmosis: experience during outbreaks in Indianapolis and review of the literature. Medicine (Baltimore) 76:339-354. [DOI] [PubMed] [Google Scholar]
- 132.Wheat, J., S. MaWhinney, R. Hafner, D. McKinsey, D. Chen, A. Korzun, K. Skahan, P. Johnson, R. Hamill, D. Bamberger, P. Pappas, J. Stansell, S. Koletar, K. Squires, R. A. Larsen, T. Cheung, N. Hyslop, K. K. Lai, D. Schneider, C. Kauffman, M. Saag, W. Dismukes, W. Powderly, et al. 1997. Treatment of histoplasmosis with fluconazole in patients with acquired immunodeficiency syndrome. Am. J. Med. 103:223-232. [DOI] [PubMed] [Google Scholar]
- 133.Wheat, J., H. Wheat, P. Connolly, M. Kleiman, K. Supparatpinyo, K. Nelson, R. Bradsher, and A. Restrepo. 1997. Cross-reactivity in Histoplasma capsulatum variety capsulatum antigen assays of urine samples from patients with endemic mycoses. Clin. Infect. Dis. 24:1169-1171. [DOI] [PubMed] [Google Scholar]
- 134.Wheat, J., P. Marichal, H. Vanden Bossche, A. Le Monte, and P. Connolly. 1997. Hypothesis on the mechanism of resistance to fluconazole in Histoplasma capsulatum. Antimicrob. Agents Chemother. 41:410-414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wheat, J., G. Sarosi, D. McKinsey, R. Hamill, R. Bradsher, P. Johnson, J. Loyd, and C. A. Kauffman. 2000. Practice guidelines for the management of patients with histoplasmosis. Clin. Infect. Dis. 30:688-695. [DOI] [PubMed] [Google Scholar]
- 136.Wheat, L. J., T. G. Slama, H. E. Eitzen, R. B. Kohler, M. L. V. French, and J. L. Biesecker. 1981. A large urban outbreak of histoplasmosis: clinical features. Ann. Intern. Med. 94:331-337. [DOI] [PubMed] [Google Scholar]
- 137.Wheat, L. J., L. Stein, B. C. Corya, J. L. Wass, J. A. Norton, K. Grider, T. G. Slama, M. L. French, and R. B. Kohler. 1983. Pericarditis as a manifestation of histoplasmosis during two large urban outbreaks. Medicine (Baltimore) 62:110-119. [DOI] [PubMed] [Google Scholar]
- 138.Wheat, L. J., R. B. Kohler, M. L. V. French, M. Garten, M. Kleiman, S. E. Zimmerman, W. Schlech, J. Ho, A. C. White, and Z. Brahmi. 1983. Immunoglobulin M and G histoplasmal antibody response in histoplasmosis. Am. Rev. Respir. Dis. 128:65-70. [DOI] [PubMed] [Google Scholar]
- 139.Wheat, L. J., E. J. Sith, and B. Sathapatayavongs. 1983. Histoplasmosis in renal allograft recipients: two large urban outbreaks. Arch. Intern. Med. 143:703-707. [PubMed] [Google Scholar]
- 140.Wheat, L. J., J. Wass, J. Norton, R. B. Kohler, M. L. V. French, and J. L. Biesecker. 1984. Cavitary histoplasmosis occurring during two large urban outbreaks: analysis of clinical, epidemiologic, roentgenographic, and laboratory features. Medicine (Baltimore) 63:201-209. [DOI] [PubMed] [Google Scholar]
- 141.Wheat, L. J., M. L. V. French, S. Kamel, and R. P. Tewari. 1986. Evaluation of cross-reactions in Histoplasma capsulatum serologic tests. J. Clin. Microbiol. 23:493-499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Wheat, L. J., R. B. Kohler, and R. P. Tewari. 1986. Diagnosis of disseminated histoplasmosis by detection of Histoplasma capsulatum antigen in serum and urine specimens. N. Engl. J. Med. 314:83-88. [DOI] [PubMed] [Google Scholar]
- 143.Wheat, L. J., R. B. Kohler, R. P. Tewari, M. Garten, and M. L. V. French. 1989. Significance of Histoplasma antigen in the cerebrospinal fluid of patients with meningitis. Arch. Intern. Med. 149:302-304. [PubMed] [Google Scholar]
- 144.Wheat, L. J., M. L. V French, and J. L. Wass. 1989. Sarcoidlike manifestations of histoplasmosis. Arch. Intern. Med. 149:2421-2426. [PubMed] [Google Scholar]
- 145.Wheat, L. J., B. E. Batteiger, and B. Sathapatayavongs. 1990. Histoplasma capsulatum infections of the central nervous system: a clinical review. Medicine (Baltimore) 69:244-260. [DOI] [PubMed] [Google Scholar]
- 146.Wheat, L. J., P. A. Connolly-Stringfield, R. L. Baker, M. F. Curfman, M. E. Eads, K. S. Israel, S. A. Norris, D. H. Webb, and M. L. Zeckel. 1990. Disseminated histoplasmosis in the acquired immune deficiency syndrome: clinical findings, diagnosis and treatment, and review of the literature. Medicine (Baltimore) 69:361-374. [DOI] [PubMed] [Google Scholar]
- 147.Wheat, L. J., P. Connolly-Stringfield, R. Blair, K. Connolly, T. Garringer, and B. P. Katz. 1991. Histoplasmosis relapse in patients with AIDS: detection using Histoplasma capsulatum variety capsulatum antigen levels. Ann. Intern. Med. 115:936-941. [DOI] [PubMed] [Google Scholar]
- 148.Wheat, L. J., P. Connolly-Stringfield, R. Blair, K. Connolly, T. Garringer, B. P. Katz, and M. Gupta. 1992. Effect of successful treatment with amphotericin B on Histoplasma capsulatum variety capsulatum polysaccharide antigen levels in patients with AIDS and histoplasmosis. Am. J. Med. 92:153-160. [DOI] [PubMed] [Google Scholar]
- 149.Wheat, L. J., P. Connolly-Stringfield, B. Williams, K. Connolly, R. Blair, M. Bartlett, and M. Durkin. 1992. Diagnosis of histoplasmosis in patients with the acquired immunodeficiency syndrome by detection of Histoplasma capsulatum polysaccharide antigen in bronchoalveolar lavage fluid. Am. Rev. Respir. Dis. 145:1421-1424. [DOI] [PubMed] [Google Scholar]
- 150.Wheat, L. J., G. Cloud, P. C. Johnson, P. Connolly, M. Goldman, A. Le Monte, D. E. Fuller, T. E. Davis, R. Hafner, the AIDS Clinical Trials Group, and the Mycoses Study Group of NIAID. 2001. Clearance of fungal burden during treatment of disseminated histoplasmosis with liposomal amphotericin B versus itraconazole. Antimicrob. Agents Chemother. 45:2354-2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Wheat, L. J. 2001. Laboratory diagnosis of histoplasmosis: update 2000. Semin. Respir. Infect. 16:131-140. [DOI] [PubMed] [Google Scholar]
- 152.Wheat, L. J., P. Connolly, N. Haddad, A. Le Monte, E. Brizendine, and R. Hafner. 2002. Antigen clearance during treatment of disseminated histoplasmosis with itraconazole versus fluconazole in patients with AIDS. Antimicrob. Agents Chemother. 46:248-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Wheat, L. J., T. Garringer, E. Brizendine, and P. Connolly. 2002. Diagnosis of histoplasmosis by antigen detection based upon experience at the histoplasmosis reference laboratory. Diagn. Microbiol. Infect. Dis. 43:29-37. [DOI] [PubMed] [Google Scholar]
- 154.Wheat, L. J., and C. A. Kauffman. 2003. Histoplasmosis. Infect. Dis. Clin. N. Am. 17:1-19. [DOI] [PubMed] [Google Scholar]
- 155.Wheat, L. J., P. Connolly, M. Durkin, B. K. Book, A. J. Tector, J. Fridell, and M. D. Pescovitz. 2004. False-positive Histoplasma antigenemia caused by antithymocyte globulin antibodies. Transpl. Infect. Dis. 6:23-27. [DOI] [PubMed] [Google Scholar]
- 156.Wheat, L. J., D. Conces, S. D. Allen, D. Blue-Hnidy, and J. Loyd. 2004. Pulmonary histoplasmosis syndromes: recognition, diagnosis, and management. Semin. Respir. Crit. Care Med. 25:129-144. [DOI] [PubMed] [Google Scholar]
- 157.Wheat, L. J., C. E. Musial, and E. Jenny-Avital. 2005. Diagnosis and management of central nervous system histoplasmosis. Clin. Infect. Dis. 40:844-852. [DOI] [PubMed] [Google Scholar]
- 158.Whitt, S. P., G. A. Koch, B. Fender, N. Ratnasamy, and D. Everett. 2004. Histoplasmosis in pregnancy. Case series and report of transplacental transmission. Arch. Intern. Med. 164:454-458. [DOI] [PubMed] [Google Scholar]
- 159.Williams, B. M., P. Fojtasek, P. Connolly-Stringfield, and L. J. Wheat. 1994. Diagnosis of histoplasmosis by antigen detection during an outbreak in Indianapolis, Ind. Arch. Pathol. Lab. Med. 118:1205-1208. [PubMed] [Google Scholar]
- 160.Wilson, D. A., H. G. Muchmore, R. G. Tisda, A. Fahmy, and J. V. Pitha. 1984. Histoplasmosis of the adrenal glands studied by CT. Radiology 150:779-783. [DOI] [PubMed] [Google Scholar]
- 161.Wilson, M. L., T. E. Davis, S. Mirrett, J. Reynolds, D. Fuller, S. D. Allen, K. K. Flint, F. Koontz, and L. B. Reller. 1993. Controlled comparison of the BACTEC high-blood-volume fungal medium, BACTEC Plus 26 aerobic blood culture bottle, and 10-milliliter isolator blood culture system for detection of fungemia and bacteremia. J. Clin. Microbiol. 31:865-871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Wood, K. L., C. A. Hage, K. S. Knox, M. B. Kleiman, A. Sannuti, R. B. Day, L. J. Wheat, and H. L. Twigg III. 2003. Histoplasmosis after treatment with anti-tumor necrosis factor-alpha therapy. Am. J. Respir. Crit. Care Med. 167:1279-1282. [DOI] [PubMed] [Google Scholar]
- 163.Woods, J. P., E. L. Heinecke, J. W. Luecke, E. Malsonado, J. Z. Ng, D. M. Retallack, and M. M. Timmerman. 2001. Pathogenesis of Histoplasma capsulatum. Semin. Respir. Infect. 16:91-101. [DOI] [PubMed] [Google Scholar]
- 164.Wynne, J. W., and G. N. Olsen. 1974. Acute histoplasmosis presenting as the adult respiratory distress syndrome. Chest 66:158-161. [DOI] [PubMed] [Google Scholar]
- 165.Yan, T. D., M. S. Kavuru, B. Yen-Lieberman, A. Brzezinski, and S. M. Gordon. 2005. Immune function evaluation (ImmunoKnow assay) in a patient treated with infliximab who developed miliary histoplasmosis. Infect. Dis. Clin. Pract. 13:315-317. [Google Scholar]
- 166.Yaseen, Z., D. Havlichek, B. Mathes, and M.-H. Hahn. 1997. Disseminated histoplasmosis in a patient with sarcoidosis: a controversial relationship and a diagnostic dilemma. Am. J. Med. Sci. 313:187-190. [DOI] [PubMed] [Google Scholar]
- 167.Young, E. J., B. Vainrub, and D. M. Musher. 1978. Pericarditis due to histoplasmosis. JAMA 240:1750-1751. [PubMed] [Google Scholar]
- 168.Zerbe, C. S., and S. M. Holland. 2005. Disseminated histoplasmosis in persons with interferon-gamma receptor 1 deficiency. Clin. Infect. Dis. 41:e38-e41. [DOI] [PubMed] [Google Scholar]