Abstract
Two novel human immunodeficiency virus protease mutations, I84C and I84A, were identified in patient isolates. The mutants with I84C displayed high-level resistance (median, at least 56-fold) to nelfinavir and saquinavir, but the majority remained susceptible to lopinavir. In contrast, isolates with the I84A mutation exhibited ≥33-fold median increased levels of resistance to nelfinavir, indinavir, amprenavir, ritonavir, lopinavir, saquinavir, and atazanavir. Isolates with the I84A or I84C mutation tended to be more resistant than the isolates with the I84V mutation. Modeling of the structure of the mutant proteases indicated that the I84V, I84C, and I84A mutations all create unoccupied volume in the active site, with I84A introducing the greatest change in the accessible surface area from that of the wild-type structure.
The selection of human immunodeficiency virus (HIV) type 1 (HIV-1) variants that are resistant to protease (PR) inhibitors (PIs) and reverse transcriptase (RT) inhibitors is an ongoing problem in the treatment of HIV-1 infection (18). Novel mutations may emerge as a consequence of the wider use of antiretroviral regimens. The identification and characterization of new mutations associated with drug resistance are critical for both individual treatment decisions and new drug design. I84V is an important primary mutation associated with resistance to the PI class of agents (1, 7, 9, 10, 12, 15-17). A mutation that results in an alanine at position 84 (I84A) has also been observed in variants following in vitro passage with the experimental PI BILA 1906 BS (8). Although the I84A and I84C mutations are documented in patient isolates in the Stanford HIV Database, selection of these mutations has not been published to date. In the present study, we describe the identification and the biological and structural characterization of the I84A mutation and another novel substitution, I84C, in clinical isolates.
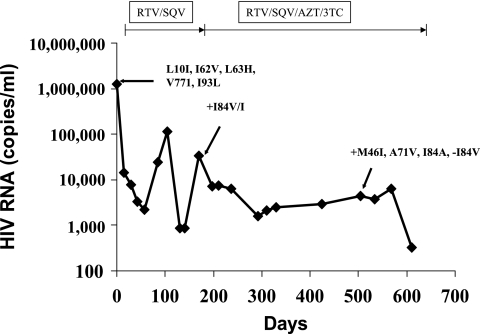
Subject A1 was PI treatment naïve before the initiation of ritonavir (RTV)-saquinavir (SQV) dual-PI therapy in 1998, with a baseline isolate containing no primary mutations but four secondary mutations (L10I, L63H, V77I, and I93L) associated with PI resistance and one polymorphism (Fig. 1), as determined by population sequencing. After an initial response, a viral rebound at day 168 was associated with the appearance of I84V. The viral load declined again following the intensification of treatment with zidovudine and lamivudine but remained at approximately 2,000 to 7,000 RNA copies/ml from day 224 to day 560. At day 505, three new PR mutations, M46I, A71V, and I84A, were observed, while I84V was no longer detected. Notably, a valine substitution (I84V) results from a single nucleotide change from the wild-type (WT) sequence, while the alanine substitution (I84A) requires two nucleotide changes but only a single change compared with the sequence of the mutant with the valine substitution. The initial appearance of I84V followed by replacement by I84A in this subject suggests that the I84V mutant underwent further evolution to I84A rather than I84A being selected from the original I84 population.
FIG. 1.
Viral load and genotypic changes in isolates from subject A1. RNA was extracted from plasma by use of a QIAamp viral RNA mini kit (QIAGEN), according to the manufacturer's protocol. Reverse transcription-PCR was performed by using a QIAGEN One-Step RT-PCR kit. Two independent PCRs were performed, and the PCR products were pooled for DNA sequence analysis with an automated ABI 3101X1 sequencer (Applied Biosystems).
To study the effect of the I84A mutation on drug susceptibility, a fragment the spanning the C-terminal end of gag, all of PR, and amino acids 1 to 305 of RT was amplified from the patient's viral RNA at the baseline and at day 505 by reverse transcription-PCR and transferred to a luciferase-based resistance test vector (Monogram Biosciences, Inc., South San Francisco, CA). The phenotype and replication capacity (RC) were determined by Monogram Biosciences, Inc., using the PhenoSense HIV assay, as described previously (3, 17a). Briefly, RC was assessed by use of a modification of the phenotypic drug susceptibility assay, whereby the luciferase activity in infected cells in the absence of drugs is compared to that of the NL4-3 reference virus, following normalization based on luciferase activity in the transfected cells. RC values are expressed as a percentage of the RC for the NL4-3 reference strain and adjusted so that the median value for WT viruses approximates 100%. The baseline isolate from this subject was sensitive to nelfinavir (NFV), SQV, indinavir (IDV), RTV, amprenavir (APV), lopinavir (LPV), and atazanavir (ATV) (data not shown). In contrast, the mutant identified at day 505 from this subject exhibited >30-fold increased resistance to all PIs tested except LPV (10-fold reduced susceptibility; isolate A1 in Table 1). The RCs of the baseline and mutant identified at day 505 were 114% and 41% (isolate A1 in Table 1), respectively.
TABLE 1.
Genotypes, phenotypes, and RCs of resistant isolates
| Isolatea | Mutation(s) in proteaseb
|
Mutation in the following cleavage sites:
|
FC in IC50 compared to that for WTc
|
RC (% of that for WT) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Amino acid at position 84 | Other mutations | p7/p1 | p1/p6 | NFV | SQV | IDV | RTV | APV | LPV | ATV | ||
| A1 | I84A | L10I, M46I, L63H, A71V, V77I | A431V | WT | 600 | 1,000 | 73 | 60 | 32 | 10 | 38 | 41 |
| A2 | I84A | L33F, M46I, L63P | NA | NA | 600 | 141 | 27 | 85 | 31 | NA | NA | NA |
| A3 | I84A | L10I, M46L, L63T, A71V | NA | NA | 600 | 365 | 78 | 76 | 43 | 11 | NA | 22 |
| A4 | I84A | L10F, M46I, L63P, A71V | WT | L449F | 600 | 241 | 58 | 42 | 32 | 14 | NA | 2.5 |
| A5 | I84A | L10V, M46I, L63A/P, A71V | A431V | L449Q | 600 | 256 | 53 | 54 | 28 | 9.0 | NA | 18 |
| A6 | I84A | L10I, M46I, L63P, A71V, L76V | A431V | WT | 64 | 24 | 38 | 34 | 21 | 14 | NA | 1.0 |
| A7 | I84A | L10F, L19I, M46I, I47V, I54V, L63P, A71V | A431V | S451I | 600 | 1,000 | 92 | 141 | 74 | 124 | NA | NA |
| A8 | I84A | L10V, K20I, M36I, M46I, A71V, G73S, L76V | A431V | WT | 600 | 265.5 | 400 | 86 | 252 | 94 | NA | 6.4 |
| A9 | I84A | L10I, M46I, L63P, A71V, V77I | WT | L449F | 600 | 1,000 | 138 | 167 | 33 | 16 | 52 | 64 |
| A10 | I84A | L10F, K20I, M46I, I54M, L63P, A71V, G73T, V77I | A431V | L449L/V, R452R/K | 600 | 1,000 | 400 | 400 | 400 | 59 | 700 | 27 |
| A11 | I84A | L10F, M46I, L63P, A71A/V, V77V/I | A431A/V | L449F | 600 | 1,000 | 73 | 73 | 47 | 14 | 63 | 31 |
| A12 | I84A | L10I, L33F, M46I, I54V, L63P, A71V, L76V | A431V | L449L/Q, S451T | 600 | 1,000 | 400 | 400 | 400 | 210 | 25 | 16 |
| A13 | I84A | L10F, K20I, M36M/I, M46I, I54V, L63P, A71V, G73S | WT | R452S | 196 | 1,000 | 178 | 400 | 43 | 50 | 700 | 5.7 |
| A14 | I84A | L10I, M46I, I47V, L63P, A71V, L76V | A431V | WT | 210 | 69 | 152 | 105 | 141 | 104 | 21 | 0.7 |
| A15 | I84A | L10I, K20R, M36I, M46I, I54V, Q58E, L63A/T, A71V, V82V/I | A431V | WT | 600 | 1,000 | 118 | 400 | 30 | 75 | 253 | 22 |
| Median | 600 | 1,000 | 92 | 86 | 43 | 33 | 57 | 18 | ||||
| C1 | I84C | WT | WT | 15 | 6.1 | 1.2 | 1.6 | 1.7 | 0.4 | NA | 12.0 | |
| C2 | I84C | K20I, M36I, V82I | WT | S451N | 59 | 14 | 1.3 | 8.6 | 5.4 | NA | NA | 11.0 |
| C3 | I84C | L10I, L19L/I, L24I, L63H | WT | L449L/F | 74 | 56 | 4.1 | 10 | 8.6 | 1.6 | NA | 8.9 |
| C4 | I84C | L10F, L19L/V, L24I, M46L, L63P | A431V | L449F | 395 | 92 | 11 | 9.1 | 10 | 3.1 | NA | 0.6 |
| C5 | I84C | L10L/I, K20R, M36I, M46L, L63P, V82IV/I | WT | WT | 51 | 41 | 3.8 | 15 | 20 | 3.1 | NA | 15.0 |
| C6 | I84C | L10I, G16A, M46I, L63P, L76V | A431V | WT | 144 | 24 | 63 | 22 | 64 | 47 | NA | 13.0 |
| C7 | I84C | L10I, L24I, M46L, L63P, A71T, G73S, V771 | A431A/V | L449F | 600 | 1,000 | 42 | 60 | 23 | 7.2 | NA | 1.2 |
| C8 | I84C | L10I, L19I, K20K/R, L24L/I, M46I, K55K/R, L63P | WT | WT | 86 | 68 | 6.4 | 14 | 12 | 2.9 | NA | 38 |
| C9 | I84C | L10V, L24L/I, M46L, I54L, L63P | WT | WT | 70 | 115 | 5.5 | 20 | 30 | 2.3 | 9.1 | NA |
| C10 | I84C | L10I, K20T, Q58E, V82I | WT | WT | 286 | 242 | 5.5 | 29 | 53 | 5.1 | 19 | 64 |
| C11 | I84C | L10I, L24I, L63H | WT | WT | 91 | 121 | 5.7 | 15 | 18 | 2.8 | 5.0 | 25 |
| Median | 86 | 68 | 5.5 | 15 | 18 | 3.0 | 9.1 | 13 | ||||
Except for the patient from whom isolate A1 was obtained, the treatment histories of the patients from which the isolates were obtained are unknown.
Reference sequences were compared with baseline sequences. Polymorphisms at the following positions are not listed: 12, 13, 14, 15, 18, 33 (other than L33F), 35, 37, 39, 41, 43, 45, 57, 60, 61, 62, 64, 65, 66, 67, 69, 70, 72, 74, 83, 89, 91, 93, and 95. Samples with a mixture of sequences at a particular codon were excluded from the analysis.
The current reduced susceptibility cutoffs are 2.5 for RTV, 3.6 for NFV, 2.3 for SQV, 10 for IDV, 4.0 for APV, and 9 for LPV-RTV. For calculation purposes FC values representing 50% inhibitory concentrations (IC50s) higher than the maximum measurable level were assigned an arbitrary value, based on the ratio between the highest drug concentration tested and the reference virus 50% inhibitory concentration: 600 for NFV, 1,000 for SQV, 400 for IDV and APV, 700 for ATV. NA, not available.
We identified the I84A mutation in an additional 25 clinical samples, 14 of which did not contain recognized primary PI mutations other than M46I or I54V or I54M (isolates A2 to A15 in Table 1). In addition, another novel mutation, I84C, was identified in 21 separate clinical isolates, 11 of which did not contain recognized primary PI mutations other than L24I, M46I or M46L, or I54V or I54M (isolates C1 to C11 in Table 1). As shown in Table 1, the M46I and A71V mutations were observed in close association with the I84A mutation (15 of 15 and 14 of 15 I84A isolates, respectively). Similarly, L24I was seen in 5 of 11 I84C isolates but was rare in I84V isolates (∼2%) and absent in I84A isolates. Previous studies have demonstrated that M46I and A71V help to restore the replication capacity and increase the resistance level when they are present in addition to primary mutations (4-6, 11), while the L24I mutation alone displayed substantially reduced catalytic activity and dimer stability (13). It is possible that the M46I and A71V mutations and the L24I mutation also play similar roles in these isolates with the I84A and I84C mutations, respectively. In addition, 85% of samples with I84A or -C also contained mutations at positions 10 (L10F/I/V) and 63 (L63A/H/P).
In order to understand the specific effects of various substitutions at position 84, the RCs and the susceptibilities to PIs of these isolates were compared to those of a large number of analogous isolates containing the I84V mutation with matched backgrounds and with all other primary PI mutations excluded (Table 2). Multiple sequences were determined from the same individual in some cases but at different time points; however, the redundancy was only about 10% with more than one result. The I84C-containing isolates, with or without M46I, displayed high-level resistance to NFV and SQV (median fold change [FC], at least 56) and low- to intermediate-level resistance to IDV, RTV, and APV (median FCs, 4 to 10), but nearly all remained susceptible to LPV (Tables 1 and 2). In contrast, the I84A isolates, with or without I54M/V, displayed high-level resistance to all PIs (median FCs, >31), with the exception of a modest level of resistance to LPV (median FC, 14) in isolates with the mutation I84A lacking I54M/V. In general, isolates containing I84A or I84C tended to be more resistant than isolates containing I84V.
TABLE 2.
Comparison between groups of samples containing I84C, I84A, and I84V with similar backgroundsa
| Genotype at position:
|
Nb | Median (range) FC in resistance
|
RC (Nc) | Median RC (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 46 | 54 | 84 | APV | IDV | LPV | NFV | RTV | SQV | |||
| M | I | V | 100 | 4.0 (1-400) | 2.4 (1-30) | 2.8 (1-174) | 4.0 (0.3-228) | 6.7 (2-400) | 4.3 (1-1,000) | 70 | 53 |
| M | I | C | 5 | 8.6 (2-53) | 4.1 (1-6) | 2.2 (0.4-5) | 74 (15-286) | 10 (2-29) | 56 (6-242) | 5 | 12 |
| I | I | V | 81 | 9.0 (1-91) | 9.1 (1-78) | 8.9 (1-162) | 9.0 (1-119) | 11 (2-82) | 4.3 (1-110) | 56 | 33 |
| I | I | A | 10 | 33 (21-252) | 73 (27-400) | 14 (9-94) | >600d (64-600) | 74 (34-167) | 261 (24-1,000) | 9 | 18 |
| IL | I | C | 6 | 21 (10-64) | 8.6 (4-63) | 3.1 (2-47) | 115 (51-600) | 18 (9-60) | 80 (24-1,000) | 5 | 13 |
| I | V | V | 51 | 36 (1-400) | 19 (1-400) | 80 (8-500) | 16 (2-129) | 49 (18-400) | 20 (1-1,000) | 38 | 27 |
| I | MV | A | 5 | 74 (30-400) | 178 (92-400) | 75 (50-211) | >600d (64-600) | >400d (141-400) | >1,000d | 4 | 19 |
Samples containing I84A, I84C, or I84V and the indicated changes at position 46 or 54 but no mutation at positions 30, 32, 48, 50, 82 (except 82I), and 90.
N, number of samples defined by mutation listed.
N, number of RC data.
The median FC for these groups was over the maximum measurable level of resistance; N, number of samples.
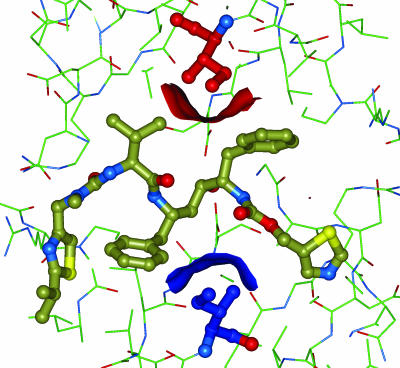
To further evaluate the mechanism by which the I84V/C/A mutations appear to contribute to resistance, a computational analysis was carried out by using the protein crystal structures of the inhibitor-HIV protease complexes (2). The central location of the two occurrences of residue 84 within the active site of the homodimeric enzyme is shown in Fig. 2. The calculated differences in total surface area (Connolly surface area, 30 surface points per Å2; 1.1-Å probe; InsightII software; Accelrys, San Diego, CA) between the WT and the modeled mutant enzymes are listed in Table 3. For all six inhibitors, the trend in the increase of the protein surface area of the mutant relative to that of the WT was the same: I84V, I84C, and I84A led to increases that ranged from 20 to 65, 30 to 112, and 150 to 193 Å2, respectively. This trend of increasing accessible surface area matches the order of loss in inhibitory potency against the mutant isolates observed and described above. Since the binding enthalpy of protein-ligand interactions is proportional to the degree of surface area buried upon complexation (14), our results suggest that one factor in the loss of inhibitor activity against the mutants is the increase in the unliganded surface area. A more extensive study, including experimental measures of binding thermodynamics, would be required to fully dissect all the factors underlying the variations in inhibition reported here.
FIG. 2.
Crystal structure of RTV bound to HIV protease showing the two symmetry-related isoleucines at positions 84 and 184 in red and blue, respectively. The surfaces of these two residues that contact the inhibitor are shown with corresponding red and blue solid surfaces.
TABLE 3.
Increases in surface area created by residue 84 mutations in HIV proteasea
| Mutation | Surface area change (Å2) for the following inhibitor:
|
|||||
|---|---|---|---|---|---|---|
| RTV | SQV | NFV | LPV | APV | IDV | |
| I84V | 65.5 | 36.7 | 36.0 | 20.6 | 33.2 | 42.5 |
| I84C | 108.8 | 62.3 | 112.8 | 30.0 | 56.3 | 96.1 |
| I84A | 193.0 | 147.5 | 150.8 | 174.2 | 158.5 | 171.1 |
The structures of each PI complex were obtained from the Protein Data Bank (accession numbers are given in parentheses): LPV (1MUI), SQV (1HXB), NFV (1OHR), RTV (1HXW), IDV (1HSG), and APV (1HPV) (2). Surface area changes were calculated as the difference in total surface area between the inhibited complexes of the WT enzymes and those of the modeled mutant enzymes.
It is notable that I84V and I84C isolates also containing M46I exhibited median of 2.3- and 1.8-fold incremental increases in resistance to all PIs, respectively, compared to those of the I84V and I84C isolates lacking M46I (Table 2). Similarly, the FC values increased by three to nine for I84V or I84A isolates containing I54M/V compared to those for isolates lacking I54M/V. Isolates with I84V plus I54V/M and I84A plus I54V/M were especially resistant to LPV (median, 75- and 80-fold increased resistance, respectively). These findings suggest that M46I and I54M/V are important mutations contributing to resistance to the PI class, particularly to LPV.
As shown in Tables 1 and 2, the RCs of both I84C and I84A mutants were impaired (median RC, <20%). It is of note that isolates with I84A (13/14) and isolates with I84C (5/11) also commonly contained mutations at the p7/p1 and/or p1/p6 cleavage sites (A431V and/or L449F/Q, respectively). It has previously been demonstrated that these cleavage site mutations may play a role in restoring the impaired fitness of I84A mutants (8). It is possible that because the mutants with the I84A and I84C mutations are defective, these mutants are unlikely to be selected when alternate pathways exist. In addition, both I84A and I84C require two nucleic acid changes from the WT sequence, imposing a higher genetic barrier for their emergence. Taken together, the high genetic barriers and the poor RCs of the mutants with the I84A and I84C mutations may account for the very low prevalence of these mutations in clinical samples.
The present study is limited by the fact that the antiretroviral treatment history was available only for a single subject, who experienced virologic failure during RTV-SQV therapy. Consequently, the PIs most likely to select either I84C or I84A in vivo are unknown. However, the substantial changes in the susceptibilities of these isolates to multiple PIs suggest that these mutations can theoretically emerge during a variety of PI-based regimens. This study is also limited by the fact that the contribution of I84C or I84A to PI resistance has not been unequivocally established by site-directed mutagenesis or phenotypic analysis of molecular clones.
In summary, we have identified two novel PR mutations, I84C and I84A, that appear at a low prevalence in isolates from patients failing antiretroviral therapy and that are associated with high-level resistance to the PI class. The RCs of the majority of these mutants were impaired, despite the coemergence of cleavage site mutations that likely increased viral fitness. Computational analysis suggests that changes in the accessible surface area for the mutant enzymes relative to that for the WT enzyme contribute to the mechanism by which the mutations appear to contribute to resistance.
Acknowledgments
The assistance of the team members from Monogram Biosciences, Inc., in obtaining the phenotypes and genotypes of the isolates described in this study is gratefully acknowledged. In addition, we thank the investigators and the study site coordinators for Studies M96-462 as well as the subjects for participating in this study.
Footnotes
Published ahead of print on 13 November 2006.
REFERENCES
- 1.Arvieux, C., and O. Tribut. 2005. Amprenavir or fosamprenavir plus ritonavir in HIV infection: pharmacology, efficacy and tolerability profile. Drugs 65:633-659. [DOI] [PubMed] [Google Scholar]
- 2.Berman, H. M., J. Westbrook, Z. Feng, G. Gilliland, T. N. Bhat, H. Weissig, I. N. Shindyalov, and P. E. Bourne. 2000. The Protein Data Bank. Nucleic Acids Res. 28:235-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Campbell, T. B., K. Schneider, T. Wrin, C. Petropoulos, and E. Connick. Relationship between in vitro human immunodeficiency virus type 1 replication rate and virus load in plasma. J. Virol. 77:12105-12112. [DOI] [PMC free article] [PubMed]
- 4.Clemente, J. C., R. Hemrajani, L. E. Blum, M. M. Goodenow, and B. M. Dunn. 2003. Secondary mutations M36I and A71V in the human immunodeficiency virus type 1 protease can provide an advantage for the emergence of the primary mutation D30N. Biochemistry 42:15029-15035. [DOI] [PubMed] [Google Scholar]
- 5.Clemente, J. C., R. E. Moose, R. Hemrajani, L. R. Whitford, L. Govindasamy, R. Reutzel, R. McKenna, M. Agbandje-McKenna, M. M. Goodenow, and B. M. Dunn. 2004. Comparing the accumulation of active- and nonactive-site mutations in the HIV-1 protease. Biochemistry 43:12141-12151. [DOI] [PubMed] [Google Scholar]
- 6.Colonno, R., R. Rose, C. McLaren, A. Thiry, N. Parkin, and J. Friborg. 2004. Identification of I50L as the signature atazanavir (ATV)-resistance mutation in treatment-naive HIV-1-infected patients receiving ATV-containing regimens. J. Infect. Dis. 189:1802-1810. [DOI] [PubMed] [Google Scholar]
- 7.Condra, J. H., W. A. Schleif, O. M. Blahy, L. J. Gabryelski, D. J. Graham, J. C. Quintero, A. Rhodes, H. L. Robbins, E. Roth, M. Shivaprakash, et al. 1995. In vivo emergence of HIV-1 variants resistant to multiple protease inhibitors. Nature 374:569-571. [DOI] [PubMed] [Google Scholar]
- 8.Croteau, G., L. Doyon, D. Thibeault, G. McKercher, L. Pilote, and D. Lamarre. 1997. Impaired fitness of human immunodeficiency virus type 1 variants with high-level resistance to protease inhibitors. J. Virol. 71:1089-1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Doyon, L., S. Tremblay, L. Bourgon, E. Wardrop, and M. G. Cordingley. 2005. Selection and characterization of HIV-1 showing reduced susceptibility to the non-peptidic protease inhibitor tipranavir. Antivir. Res. 68:27-35. [DOI] [PubMed] [Google Scholar]
- 10.Gianotti, N., E. Seminari, M. Guffanti, E. Boeri, P. Villani, M. Regazzi, A. Bigoloni, G. Schira, S. Tiberi, G. Fusetti, A. Lazzarin, and A. Castagna. 2005. Evaluation of atazanavir Ctrough, atazanavir genotypic inhibitory quotient, and baseline HIV genotype as predictors of a 24-week virological response in highly drug-experienced, HIV-infected patients treated with unboosted atazanavir. New Microbiol. 28:119-125. [PubMed] [Google Scholar]
- 11.Ho, D. D., T. Toyoshima, H. Mo, D. J. Kempf, D. Norbeck, C. M. Chen, N. E. Wideburg, S. K. Burt, J. W. Erickson, and M. K. Singh. 1994. Characterization of human immunodeficiency virus type 1 variants with increased resistance to a C2-symmetric protease inhibitor. J. Virol. 68:2016-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kempf, D. J., J. D. Isaacson, M. S. King, S. C. Brun, Y. Xu, K. Real, B. M. Bernstein, A. J. Japour, E. Sun, and R. A. Rode. 2001. Identification of genotypic changes in human immunodeficiency virus protease that correlate with reduced susceptibility to the protease inhibitor lopinavir among viral isolates from protease inhibitor-experienced patients. J. Virol. 75:7462-7469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu, F., P. I. Boross, Y. F. Wang, J. Tozser, J. M. Louis, R. W. Harrison, and I. T. Weber. 2005. Kinetic, stability, and structural changes in high-resolution crystal structures of HIV-1 protease with drug-resistant mutations L24I, I50V, and G73S. J. Mol. Biol. 354:789-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Luque, I., and E. Freire. 2002. Structural parameterization of the binding enthalpy of small ligands. Proteins 49:181-190. [DOI] [PubMed] [Google Scholar]
- 15.Marcelin, A. G., D. Affolabi, C. Lamotte, H. A. Mohand, C. Delaugerre, M. Wirden, D. Voujon, P. Bossi, N. Ktorza, F. Bricaire, D. Costagliola, C. Katlama, G. Peytavin, and V. Calvez. 2004. Resistance profiles observed in virological failures after 24 weeks of amprenavir/ritonavir containing regimen in protease inhibitor experienced patients. J. Med. Virol. 74:16-20. [DOI] [PubMed] [Google Scholar]
- 16.Molla, A., M. Korneyeva, Q. Gao, S. Vasavanonda, P. J. Schipper, H. M. Mo, M. Markowitz, T. Chernyavskiy, P. Niu, N. Lyons, A. Hsu, G. R. Granneman, D. D. Ho, C. A. Boucher, J. M. Leonard, D. W. Norbeck, and D. J. Kempf. 1996. Ordered accumulation of mutations in HIV protease confers resistance to ritonavir. Nat. Med. 2:760-766. [DOI] [PubMed] [Google Scholar]
- 17.Patick, A. K., H. Mo, M. Markowitz, K. Appelt, B. Wu, L. Musick, V. Kalish, S. Kaldor, S. Reich, D. Ho, and S. Webber. 1996. Antiviral and resistance studies of AG1343, an orally bioavailable inhibitor of human immunodeficiency virus protease. Antimicrob. Agents Chemother. 40:292-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17a.Petropoulos, C. J., N. T. Parkin, K. L. Limoli, Y. S. Lie, T. Wrin, W. Huang, H. Tian, D. Smith, G. A. Winslow, D. J. Capon, and J. M. Whitcomb. 2000. A novel phenotypic drug susceptibility assay for human immunodeficiency virus type 1. Antimicrob. Agents Chemother. 44:920-928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sethi, A. K., D. D. Celentano, S. J. Gange, J. E. Gallant, D. Vlahov, and H. Farzadegan. 2004. High-risk behavior and potential transmission of drug-resistant HIV among injection drug users. J. Acquir. Immune Defic. Syndr. 35:503-510. [DOI] [PubMed] [Google Scholar]