Abstract
Salicylate has previously been shown to reduce the susceptibility of Mycobacterium tuberculosis to several drugs in vitro. In this study, aspirin, a salicylate anti-inflammatory, antagonized isoniazid treatment of murine pulmonary tuberculosis, whereas the nonsalicylate ibuprofen did not. These results may have implications on concurrent administration of anti-inflammatory and antituberculosis drugs.
Aspirin (acetylsalicylic acid) is in widespread use for the treatment and prevention of numerous medical conditions. Salicylate, the active metabolite of aspirin, has also been shown to induce multiple drug resistance in various bacterial species (5, 6). Previously reported in vitro data demonstrated that exposure of Mycobacterium tuberculosis to salicylate increased resistance to isoniazid, streptomycin, rifampin, and ethambutol in an originally susceptible strain of H37Ra (7). However, the mechanism underlying this effect in M. tuberculosis is not known. Transcriptional analysis of M. tuberculosis revealed that incubation with salicylate led to the upregulation of genes, including a 27-kDa methyltransferase and a flavin adenine dinucleotide-associated acyl-coenzyme A dehydrogenase involved in fatty acid oxidation (2). Salicylate exposure downregulated a range of genes involved in transcription and translation, including 30S and 50S ribosomal subunits and rpoB (2), the β-subunit of RNA polymerase and target of rifampin. The antibiotic isoniazid acts, after conversion by KatG (8), through inhibition of InhA, which is involved in mycolic acid synthesis (1). From the transcriptional profile, salicylate appears to trigger a general decrease in metabolism in M. tuberculosis, causing phenotypic resistance to antibiotics such as isoniazid.
Although salicylate was shown in vitro to decrease susceptibility to several antituberculosis (anti-TB) drugs (7), the implications of this finding on the treatment of tuberculosis in vivo had yet to be examined. In this study, we investigated the effect of aspirin on isoniazid treatment of TB in a murine model. Ibuprofen, a nonsteroidal anti-inflammatory drug (NSAID) that is not a salicylate, was also included in the comparison.
A nonestablished aerosol infection mouse model was employed to evaluate daily administration of these anti-inflammatory drugs in TB therapy. Four-week-old BALB/c mice were infected by aerosol with M. tuberculosis H37Rv as previously described (4) and randomized to five mice per group. Treatments were initiated the day after aerosol exposure and were administered five times per week. The following dosages were dissolved in 0.2 ml sterile water and administered by oral gavage: aspirin (10, 20, and 40 mg/kg of body weight), ibuprofen (10, 20, and 40 mg/kg), and isoniazid (25 mg/kg) (compounds obtained from Sigma). Dosages of aspirin and ibuprofen were chosen for similarity to amounts used for treatment of humans for pain and rheumatoid arthritis and, in the case of aspirin, prevention of heart disease (3). Since isoniazid alone can clear a nonestablished aerosol infection in mice after a short course of therapy, the study was concluded after a month of treatment to detect antagonism by either NSAID. Mice were euthanized the day following the treatment completion. Enumerations of live bacteria from lungs and spleens of animals in each group were made by plating organ homogenates on 7H11 agar with ADC and PANTA supplementation (DIFCO) following incubation for 3 weeks at 37°C. After 1 month of infection, nontreated controls had 6.91 ± 0.09 log10 CFU in the lung and 4.54 ± 0.22 log10 CFU in the spleen.
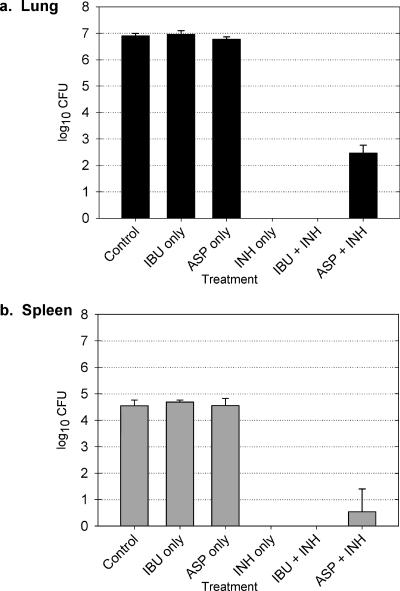
First, the impact of aspirin or ibuprofen alone on the development of tuberculosis was evaluated. Aspirin or ibuprofen treatment had no effect on the number of viable bacilli in the lungs of these animals (Fig. 1). At doses of 10 to 40 mg/kg, ibuprofen had no significant effect on spleen bacterial counts after 1 month of treatment (data not shown). Animals that received aspirin in low doses (10 mg/kg) exhibited a small but significant decrease in spleen infection compared to controls (3.48 ± 0.52 log10 CFU; P = 0.04), while no difference was detected with higher aspirin doses of 20 and 40 mg/kg (4.55 ± 0.27 log10 CFU and 4.38 ± 0.15 log10 CFU, respectively).
FIG. 1.
Effect of aspirin or ibuprofen administered in combination with isoniazid on lung (a) and spleen (b) log10 CFU in murine tuberculosis. ASP only, aspirin (20 mg/kg of body weight); IBU only, ibuprofen (20 mg/kg); INH only, isoniazid (25 mg/kg); ASP + INH, aspirin and isoniazid (20 and 25 mg/kg, respectively); IBU + INH, ibuprofen and isoniazid (20 and 25 mg/kg, respectively).
Coadministration of ibuprofen with isoniazid had no significant effect on CFU counts of bacteria in either organ (Fig. 1). However, the combination of 20 mg/kg aspirin and 25 mg/kg isoniazid, compared to isoniazid alone, was associated with increased numbers of bacteria in the spleen and lungs (Fig. 1). Isoniazid-only treatment resulted in complete clearance of M. tuberculosis from the lungs and spleen (with a lower limit of detection of 0.90 log10 CFU). One mouse in the group coadministered aspirin and isoniazid had a spleen positive for infection (2.16 log10 CFU), while the other mice in this group had no culturable bacteria in the spleen (Table 1). Aspirin appeared to antagonize the action of isoniazid, since complete clearance of the infection was not seen in the groups receiving the aspirin and isoniazid in combination (Table 1). While mice in the isoniazid-only group had culture-negative lungs, all mice in the aspirin-isoniazid group had lungs positive for M. tuberculosis (2.46 ± 0.30 log10 CFU). In addition, all mice in the ibuprofen-isoniazid group were negative for lung or spleen infection.
TABLE 1.
Impact of aspirin or ibuprofen on organ culture conversion in isoniazid treatment of tuberculosis in mice
| Treatment groupa | No. of mice with culture-positive organ/total no. of mice in groupb
|
|
|---|---|---|
| Lung | Spleen | |
| Control | 5/5 | 5/5 |
| Isoniazid (25 mg/kg) | 0/5 | 0/5 |
| Ibuprofen (20 mg/kg) | 5/5 | 5/5 |
| Aspirin (20 mg/kg) | 5/5 | 5/5 |
| IBU + INH | 0/5 | 0/5 |
| ASP + INH | 5/5 | 1/5 |
IBU + INH, 20 mg/kg ibuprofen and 25 mg/kg isoniazid in combination; ASP + INH, 20 mg/kg aspirin and 25 mg/kg isoniazid in combination.
The lower limit of detection is 0.90 log10 CFU per total organ.
Our hypothesis, based on in vitro data regarding salicylate's effect on the transcriptional profile and drug susceptibility of the bacilli, was that aspirin would inhibit the bactericidal activity of isoniazid. Alternatively, aspirin or ibuprofen may impact the course of infection in vivo through their immunomodulatory effects on the host.
This study is the first to show the effect of salicylate on reducing the effect of antibiotic treatment of tuberculosis despite the observation of a similar phenomenon 20 years ago in Escherichia coli (6). In this study, aspirin appeared to antagonize isoniazid in vivo, whereas ibuprofen has no detrimental interaction with isoniazid during the therapy. To avoid antagonism with antibiotic therapy, ibuprofen may replace aspirin for the TB patient in instances in which the use of an NSAID is indicated. But before a conclusion can be made about the scenario in humans, further investigation is necessary. The effect of salicylate or aspirin on treatment with other TB drugs, in long-term therapy of established infection, and on the immune response to TB infection should be examined to elucidate the clinical significance of these findings.
Acknowledgments
We thank Sandeep Tyagi, Eric Nuermberger, and Jacques Grosset for assistance with the mouse model of TB infection.
Y.Z. was supported by National Institutes of Health grants AI44063 and AI49485 and the Natural Science Foundation of China (grant 30328031).
Footnotes
Published ahead of print on 4 December 2006.
REFERENCES
- 1.Banerjee, A., E. Dubnau, A. Quemard, V. Balasubramanian, K. S. Um, T. Wilson, D. Collins, G. de Lisle, and W. R. Jacobs, Jr. 1994. InhA, a gene encoding a target for isoniazid and ethionamide in Mycobacterium tuberculosis. Science 263:227-230. [DOI] [PubMed] [Google Scholar]
- 2.Denkin, S., S. Byrne, C. Jie, and Y. Zhang. 2005. Gene expression profiling analysis of Mycobacterium tuberculosis genes in response to salicylate. Arch. Microbiol. 184:152-157. [DOI] [PubMed] [Google Scholar]
- 3.Eidelman, R. S., P. R. Hebert, S. M. Weisman, and C. H. Hennekens. 2003. An update on aspirin in the primary prevention of cardiovascular disease, Arch. Intern. Med. 163:2006-2010. [DOI] [PubMed] [Google Scholar]
- 4.Nuermberger, E. L., T. Yoshimatsu, S. Tyagi, R. J. O'Brien, A. N. Vernon, R. E. Chaisson, W. R. Bishai, and J. H. Grosset. 2004. Moxifloxacin-containing regimen greatly reduces time to culture conversion in murine tuberculosis. Am. J. Respir. Crit. Care Med. 169:421-426. [DOI] [PubMed] [Google Scholar]
- 5.Price, C. T., I. R. Lee, and J. E. Gustafson. 2002. The effects of salicylate on bacteria. Int. J. Biochem. Cell Biol. 32:1029-1043. [DOI] [PubMed] [Google Scholar]
- 6.Rosner, J. L. 1985. Nonheritable resistance to chloramphenicol and other antibiotics induced by salicylates and other chemotactic repellents in Escherichia coli K-12. Proc. Natl. Acad. Sci. USA 82:8771-8774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schaller, A., Z. Sun, Y. Yang, A. Somoskovi, and Y. Zhang. 2002. Salicylate reduces susceptibility of Mycobacterium tuberculosis to multiple antituberculosis drugs. Antimicrob. Agents Chemother. 46:2636-2639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang, Y., B. Heym, B. Allen, D. Young, and S. Cole. 1992. The catalase-peroxidase gene and isoniazid resistance of Mycobacterium tuberculosis. Nature 358:591-593. [DOI] [PubMed] [Google Scholar]