Abstract
Employment status is commonly used as a sign of stability in recovery and an outcome variable for substance abuse treatment and research. However, there has been little attention in the literature on the topic of work for the dually diagnosed (i.e., persons diagnosed with both substance use and mental health disorders). Data collected in 1999 are presented on expressed interest in and perceived barriers to pursuing work and on the utilization of vocational rehabilitation (voc-rehab) services among unemployed members of a dual recovery self-help fellowship (N = 130). While members generally expressed high interest in working, they also cited multiple obstacles to attaining and maintaining employment. A path model was specified and tested. Significant contributors to interest in working were substance use status and physical health rating. Consistent with our hypotheses, mental health symptoms and greater perceived obstacles (e.g., stigma, fear of failure, and insufficient skills) were significant contributors to perceived difficulty in pursuing work, whereas substance use, physical health, and recency of employment were not. Finally, those who perceived less difficulty in pursuing work were more likely to utilize voc-rehab services, and men were more likely than women to use these facilities; interest in work was not significantly associated with utilizing voc-rehab services. The roles of mental health disorders and substance use in relation to pursuit of employment are discussed, as well as that of perceived obstacles such as stigma. The paper addresses the setting of realistic vocational goals and possible strategies to mitigate barriers to increased employment of dually diagnosed individuals.
Keywords: Employment, Dual-diagnosis, Comorbidity, Recovery, Entitlement
INTRODUCTION
Work plays many important roles in our society. It is the primary source of income and, often, of health insurance; it largely defines social identity, social class, and opportunities for social and financial advancement [e.g., (1)]. Work also provides a frame of reference and various structures of functioning. However, for many, employment remains an elusive goal. This is true of individuals with substance dependency or mental health disorders, and even more so of those dually diagnosed with both disorders. In spite of the high prevalence of comorbidity among substance users and mental health clients (2), the topic of employment among the dually diagnosed has received little empirical attention. This paper presents data on self-reported utilization of vocational rehabilitation (vocrehab) services, interest in and obstacles to pursuit of employment among dually diagnosed persons, and it examines the association among these variables.
BACKGROUND
Employment has been identified as a positive treatment outcome and an indicator of recovery for substance-using clients as well as for those with a mental health disorder (1,3–6). Employment has both economic and non-economic benefits for recovering individuals and contributes to higher-level functioning [e.g., (7)]. It has been associated with reduced substance use (8), decreased psychiatric symptoms and hospitalization, increased self-esteem, and improved quality of life (9–13).
For dually diagnosed individuals, the process and the outcomes of work can be beneficial in several ways (14). Work occupies time and provides structure, two important issues for recovering individuals [(15); also see (16)]; it offers an opportunity for social connections and for socialization with non substance users who can function as role models (17). Being employed can enhance personal mastery, self-esteem, and self-efficacy (13,18), an important benefit for persons whose disorders are highly stigmatized. By providing something valued that can be lost to relapse to drug use or to hospitalization, work can strengthen one’s commitment to recovery (14,19). Finally, work provides legitimate income that can end or lessen dependence on disability benefits whose rules “enforce poverty” (20,21), and thus it contributes to increasing the quality of life. While employment can be beneficial in many ways, it can also be a source of stress that may lead to mental health problems and to relapse [e.g., (22)].
The many benefits of employment are not available to most dually diagnosed persons as employment rates for this group are considerably lower than those in the general population [e.g., (23–27)]. The aggregate employment rate for persons with mental illness is between 10% and 15% [(28–30); also see (31)] and chronic unemployment is common (32). Work status among the dually diagnosed has rarely been addressed empirically and there is little attention given to whether these individuals are candidates for work (14).
While employment rates are low among recovering individuals, there is evidence that such individuals express interest in being employed, although the literature on this topic is scarce. Among mental health clients, getting a job is the often cited as an important self-reported goal [(33); also see (34,35)] and substance users express interest in training and employment [e.g., (36–39)]. However, recovering individuals face many potential barriers to employment. At the societal level, the first and greatest barrier is stigma. Recently, the Surgeon General (40) cited the stigma of mental illness as the foremost barrier to services among nearly half of all Americans who have a severe mental illness and do not seek treatment. A national survey documented a bias among employers against hiring former substance users (41). For dually diagnosed individuals, the dual stigma may result in low self-expectations [e.g., see (42)] and low self-efficacy (43) so that challenges are avoided. Another societal obstacle to employment may be the entitlement system itself. Receiving entitlements affects one’s sense of self as well as the outcome of treatment and rehabilitation (44), and the rules may provide a strong disincentive to being employed [e.g., (11)]. Further, disability benefits provide much-needed health insurance that covers medications and psychiatric care, unlike many of the low-paying jobs filled by persons lacking the technical skills the workplace increasingly demands.
At the individual level, dually diagnosed persons may face multiple obstacles to gaining and retaining employment. First, the disorders themselves present a barrier to employment [e.g., (45)]; among the mentally ill, symptoms and medication side effects may cause cognitive impairments and physical distress that interfere with skills acquisition and job performance (46). Second, such persons face many interrelated problems, some job related, others not. Job-related obstacles to employment include lack of work experience (47), poor work history (48), low levels of marketable skills and pre-employment skills (e.g., resumé writing), inadequate work readiness (49), and poor social and work relations skills (47); recovering individuals may also lack skills other than those that are job related, such as personal habits, time management, impulse control, and self-presentation [for review, see (50–52)]. Overall, for recovering individuals, getting a job is a job in itself, especially for those who have lost or never gained the skills necessary for sustainable employment (52).
Vocational and rehabilitation services for recovering individuals aim to address some of the barriers to employment summarized above. While such services are insufficiently emphasized [e.g., see (1)] and tend to be offered only after the rehabilitation process—especially abstinence—has been achieved (14,15,53,54), empirical findings suggest that clients do benefit from such services [e.g., (55–57)]. There has been little effort to extend vocational services to dually diagnosed persons (14). In what follows, we present data on interest in working and obstacles to employment as experienced by dually diagnosed persons. This appears to be the first such investigation. The study tested three hypotheses:
Better mental and physical health, less substance use, and more recent work history will be associated with greater interest in current employment.
More recent substance use, poorer physical and mental health, less recent work history, greater fear of failure, greater perceived stigma and inability to “fit in,” greater perceived need for treatment and for education, disincentive from the entitlement system, and poorer impulse control will be associated with greater perceived difficulty in pursuing work.
Greater interest in working and lower levels of perceived difficulty in pursuing employment will be associated with greater utilization of voc-rehab services.
METHOD
Setting and Sample
Participants were members of Double Trouble in Recovery (DTR) who reported no employment in the preceding year (N = 130). The DTR group is a dual-focus self-help program adapted from the 12-step program [see (58)]. Members were recruited at 25 meeting sites throughout New York City. The study was described as an investigation of effectiveness of self-help participation among dually diagnosed persons. Participation in the study was voluntary, based on informed consent; 15% of DTR members declined to take part in the study, chiefly because of concerns about confidentiality, especially at meetings held in treatment facilities. The interviews were conducted at the participants’ residences between January and December 1999. Recruitment and interviewing were performed by three long-term DTR members (an African-American male and two Caucasian females; their ages ranged from 30 to 39 years) who received training in interviewing skills by senior research staff. Participants received $40 in reimbursement for their time (2.5 hr).
Measures
Data were obtained during the 1-year follow-up data collection of this longitudinal study, using a semistructured interview protocol covering sociodemographics and background, mental health status and history, mental health treatment history (including medications), substance use status and history, substance use treatment history, and history of participation in DTR and other 12-step fellowships. Primary substance and primary psychiatric diagnosis were obtained from self-report. The following measures were used—all reported Alphas were computed for the present study data.
Mental Health
We used the Colorado Symptom Index (CSI), a checklist of 13 items developed to determine the presence of symptoms among persons diagnosed with severe persistent mental illness (59); the authors report good psychometric properties, including construct validity and inter-rater reliability. Respondents were asked: “In the past year, have you [item]?” Sample items are: felt depressed? forgot important things? felt like seriously hurting someone? (Alpha = .88) A summed score was computed (score range of 1–13); a higher score represents higher mental health distress.
Substance Use
This assessed the use of alcohol and illicit drugs in the past year: “In the past year, did you use [name of substance]?” (Any use of each drug = 1, no use = 0.)
Physical Health
“Overall, how would you describe your health in the past month?” (4 = Poor, 3 = Fair, 2 = Good, and 1 = Excellent.)
Recency of Employment
The measure of interest for the analyses was “How long ago did you last work?” The answers were coded in number of months since last worked.
Interest in Employment
“To what extent are you currently interested in working?” (0 = ”Not at all” to 10 = ”Extremely.”) We also looked at participants’ answers to one of the open-ended questions in the final section of the questionnaire: “What do you hope to do, change, accomplish, in the next year?” (Codes for the open-ended questions were developed on the first 30 completed interviews; based on a subsample of 25 instruments coded by two independent researchers, inter-rater reliability was r = .92.)
Perceived Obstacles to Employment
This construct was assessed in two ways: (1) an open-ended item asked: “What may make it hard for you to be employed right now?” Answers were coded to allow up to four statements. (2) A structured list of items was developed in collaboration with DTR members consulting on this study and from members’ answers to open-ended questions in qualitative interviews reported elsewhere (58). The final list consisted of 12 items presented in the Results section (Chronbach Alpha = .88). Respondents were asked: “How strongly do you agree or disagree with each statement. Most dually diagnosed people find it hard to be employed because of [item].”
Perceived Difficulty in Pursuing Work
The Recovery Challenges Scale, developed for this study, consists of 35 items representing areas identified, in focus groups, as difficult for individuals in dual recovery [e.g., “dealing with being bored,” “regaining the trust of loved ones”—Chronbach Alpha = .97; (60)]. The items are written approximately at the 8th grade reading level. The instrument has shown good construct validity in ongoing analyses, with modest to moderate correlations with indices of ongoing stress. The instructions are: “Following are issues and situations that people may struggle with during their recovery from dual-diagnosis. Please rate each according to your own experience dealing with these issues in recovery.” Pretesting indicated that the instrument was feasible to use with this sample. For this study, we looked at the item: “Working, finding work, or keeping a job.” (1 = not at all difficult to do, 2 = a little, 3 = moderately, and 4 = very difficult.)
Vocational Services
Utilization. The service utilization inventory originally developed for mental health clients (61) contains two items assessing the use of training and employment-related services in the preceding 12 months: “job finding or placement services” and “support for education.” A summary score of these two items was created.
Need. Following the service utilization section, we asked “In the past 12 months, were there any services you wanted but were unable to get?” Those answering positively were asked to identify the service(s), followed by: the question “How come you were unable to get that service?” Answers were coded as described above.
Analytical Procedures
From the hypotheses presented earlier, a path model was specified and tested using a three-phase procedure:
The predictor and outcome variables, as well as sociodemographic and background variables (age, gender, ethnic background, education levels, primary substance, and primary diagnosis) were included in a bivariate correlation matrix.
Multiple regression analyses with simultaneous entry were conducted with interest in working and perceived difficulties in pursuing work as dependent variables to test the first two hypotheses. For the regression on perceived difficulty, an obstacle index was constructed consisting only of the individual obstacles significantly associated with perceived difficulty in bivariate analyses.
Interest in working, perceived difficulty and the sociodemographic variables identified as being significant were regressed on utilization of vocational rehabilitation services to test the third hypothesis. One-tailed tests of significance are used throughout because directional hypotheses are being tested.
RESULTS
Sociodemographics
Participants were predominantly male and ethnically diverse (Table 1); most relied on disability income as their primary source of income and resided in supported housing. Education levels were generally low. One-half of participants reported having a chronic medical condition; most prevalent were asthma and other respiratory problems (15%), hypertension (12%), diabetes (7%), HIV (6%), hepatitis C (6%), chronic pain (4%), and heart disease (3%). Forty-six percent were taking prescribed medication for a medical illness or condition. Participants rated their health in the previous month as “excellent” (23%), good (42%), fair (25%), and poor (10%).
Table 1.
Selected Sample Characteristics
| Male | 69% |
| Age | 40 years (mean; SD = 8.8) |
| Ethnic background: | |
| African-American | 54% |
| Caucasian | 26% |
| Mixed or other | 3% |
| Hispanic (total) | 17% |
| Puerto-Rican | 15% |
| Other Hispanic | 2% |
| Born in the United States | 86% |
| Primary income | |
| Disability payments | 96% |
| Pension/vets’ benefits | 4% |
| Monthly income | $647 (mean; SD = 309) |
| Education | |
| Less than HS grad/GEDa | 46% |
| HS grad/GED | 31% |
| Some college or more | 23% |
| Living arrangements | |
| Supported housing | 72% |
| Own apt/house | 18% |
| w/ friends/relatives | 7% |
| Shelter | 3% |
| Chronic medical condition | 47% |
| Employment | |
| Ever worked | 89% |
| Last worked (among ever employed) | 6 years (mean; SD = 7.2) |
| Substance use | |
| Age at 1st use | 15 years (mean; SD = 5) |
| Primary substance (lifetime) | |
| Crack/cocaine | 41% |
| Alcohol | 35% |
| Heroin | 11% |
| Marijuana | 10% |
| Other | 3% |
| Any substance use past year | 30% |
| Any substance use past month | 9% |
| Mental health | |
| Age 1st emotional/mental health problems | 19 years (mean; SD = 11) |
| Age 1st diagnosed | 29 years (mean; SD = 11) |
| Primary diagnosis: | |
| Schizophrenia | 40% |
| Unipolar (major) depression | 21% |
| Bipolar disorder | 21% |
| Schizoaffective | 8% |
| Mood disorder | 4% |
| Other | 6% |
| Experienced symptoms past year | 60% |
| Colorado Symptom Index score | 6.3 (mean; SD = 4.0) |
| Emotional/mental health past month | |
| Very troubled | 6% |
| Moderately troubled | 22% |
| Somewhat troubled | 38% |
| Not at all troubled | 34% |
| Treatment—currently in outpatientb | 68% |
| Prescribed psychiatric medications | 91% |
| Age at 1st treatment—mental health | 25 years (mean; SD = 12) |
| Age at 1st treatment—substance use | 28 years (mean; SD = 5) |
| Ever hospitalized—mental health | 90% |
| Self-help attendance (once a month or more) | |
| Double Trouble in Recovery | 75% |
| Alcoholics or Narcotics Anonymous | 66% |
HS, high school; GED, general equivalency diploma.
Alcohol/”drug abuse,” mental health or dual-diagnosis.
Alcohol and Illicit Drugs Use
Participants reported extensive experience with substance use, beginning in adolescence. The primary substance (lifetime) was crack-cocaine. About one-third reported substance use in the year preceding the interview, 9% in the past month.
Mental Health
Participants also had a long history of mental health symptoms, beginning, on average, in late adolescence. Most prevalent diagnoses were schizophrenia, bipolar disorder, and major depression. Nearly two-thirds experienced symptoms in the past year; number of symptoms reported on the CSI ranged from zero to 13; mean = 6.3; SD = 4.0.
Formal Treatment
Subjects were found to have had extensive experience with treatment, both for mental health and “substance abuse,” beginning in their mid- and late 20s, respectively. At the time of the study, most were taking psychiatric medications and two-thirds were enrolled in outpatient treatment (60% in a dual-diagnosis program, 5% in drug abuse treatment, and 3% in a mental health treatment).
Self-Help Groups Participation
In addition to formal treatment, participants also attended traditional 12-step groups [e.g., Alcoholics Anonymous (AA) and Narcotics Anonymous (NA)] as well as DTR. Median length of DTR affiliation was 2.75 years (range = 13 months to 9 years); 61% had attended the group for the entire year preceding the interview.
Recency of Employment
Time since participants’ last job ranged from 1 to 31 years ago (median = 6 years); they had worked primarily as service workers (44%), in sales (13%), or in a technical field (7%), and had held their last job for a median of 1 year; 11% had never been employed.
Perceived Obstacles to Employment
The most common answers to the open-ended question fell into three categories: mental illness including symptoms and side effects from medications (29%); physical health and physical disability (22%); and scheduling conflicts with treatment program (17%). Also mentioned were: need for skills or education (7%), “nothing” (7%), financial disincentives from entitlement regulations or because of low-paying jobs (6%), addiction and substance use history (3%), stage of recovery (not far along—3%), fear of failure (3%), and difficulty handling stress or pressure (3%).
There was little variation in levels of agreement across items from the structured list (Table 2). “Strongly agree” ratings ranged from 16% (“difficulties interacting with people”) to 31% (“fear of failure”), while “strongly disagree” ratings were low across all items, and ranged from 1% to 3%. Overall, all items received a combined “strongly agree/agree” rating of about 70% or higher.
Table 2.
Obstacles to Working (Items Ranked in Descending Order of Strong Agreement)
| Strongly
|
Strongly
|
|||
|---|---|---|---|---|
| Disagree (%) | Disagree (%) | Agree (%) | Agree (%) | |
| Fear of failure | 3 | 13 | 53 | 31 |
| Need for education/skills | 2 | 18 | 54 | 26 |
| Need to stay totally focused on recovery | 2 | 18 | 56 | 24 |
| Impulse control | 1 | 23 | 53 | 23 |
| SSI, SSD, awelfare rules about working | — | 25 | 52 | 23 |
| Need to stay in day treatment/program | 2 | 19 | 57 | 22 |
| Anger management | 2 | 28 | 50 | 20 |
| Therapist says I should wait | 2 | 23 | 58 | 17 |
| Stigma | 2 | 26 | 55 | 17 |
| Not “clean” long enough | 1 | 30 | 52 | 17 |
| Concerns about not fitting in | 3 | 19 | 62 | 16 |
| Difficulties interacting with people | 2 | 24 | 60 | 16 |
SSI = Supplemental Security Income.
SSD = Social Security Disability Insurance (typically abbreviated in the US as “SSD”).
Perceived Difficulty in Pursuing Work
Participants were equally divided in their experiences. About one-third (35%) rated “working, finding work, or keeping a job” as “very difficult to do”, 19% as “moderately difficult,” 13% “a little difficult,” 33%, “not at all difficult.”
Correlates of Perceived Difficulties in Pursuing Work
Mental health symptoms in the past year and the following six obstacles were significant covariates of perceived difficulty in pursuing work (Table 3): fear of failure, need for education and skills, impulse control, need to stay in treatment, stigma, and concerns about fitting in.
Table 3.
Correlations Among Key Variables (N = 130)
| Interest in Working Perceived | Difficulty in Pursuing Work | |
|---|---|---|
| Substance use past year | −.21** | .03 |
| Mental health symptoms past year | .07 | .34** |
| Health past month | −.19* | .15 |
| When last worked | −.19* | .04 |
| Interest in working | — | −.08 |
| Perceived difficulty in pursuing work | −.08 | — |
| Obstacles to employment | ||
| Fear of failurea | .07 | .28** |
| Need for education/skillsa | .07 | .25** |
| Need to stay totally focused on recovery | .08 | .13 |
| Impulse controla | .09 | .21* |
| SSI, SSD, welfare rules about working | .02 | .04 |
| Need to stay in day treatment/programa | .07 | .17* |
| Anger management | −.02 | .05 |
| Therapist says/suggests I should wait | .11 | .16 |
| Stigmaa | .01 | .19* |
| Not clean long enough | .09 | .15 |
| Concerns about not fitting ina | .17* | .28** |
| Difficulty interacting with people | .11 | .14 |
| Index of perceived obstacles to employment | .10 | .32** |
p<.05;
p<.01.
Item included in index of perceived obstacles to employment.
SSI = Supplemental Security Income.
SSD = Social Security Disability Insurance (typically abbreviated in the US as “SSD”).
Interest in Working
Interest in work was generally high (mean = 6.7, SD = 3.6); 36% reported being “extremely” interested while 16% expressed no interest. Interest in working was also evident in participants’ stated goals for the next year, where employment and education were mentioned most often; nearly one-half (48%) mentioned getting a job, or training or gaining skills to get a job, as a goal, and one-third (31%) reported education (including obtaining a GED) as a goal.
Correlates of Interest in Working
Bivariate analyses revealed three significant correlates of interest in working: substance use in the previous year, physical health in the previous month, and recency of employment (Table 3). Participants who reported no substance use in the past year also expressed a higher level of interest in working than did those who had used drugs and/or alcohol (r = −.21, p<.05). Better physical health was associated with greater expressed interest in working (r = .19, p<.05), and the more time since participants were last employed, the lower was their interest in being employed (r = −.19, p<.05).
Utilization of Vocational Rehabilitation Services
Twenty percent of participants reported use of such services in the previous year; 5% has used job-placement or job-finding services, 17%, support for education, and 2% had used both. Few(4%) participants reported being unable to obtain needed education or vocational services; among those who did, with the exception of two individuals, the reasons why the services were not obtained were unrelated to mental health or to “substance abuse.”
Correlates of Utilization of Vocational Rehabilitative Services
Bivariate correlations between utilization of services and sociodemographic variables revealed a significant association with gender: men were more likely than women to have used educational support services in the preceding year (26% vs. 8%, p = .02).
Path Analysis
Consistent with our hypotheses, physical health and substance use were associated with expressed interest in working (Beta = −.23, p = .009 and Beta = −.25, p = .005, respectively). Results did not support the hypothesized paths between interest in working and recency of employment (Beta = −.11) or mental health symptoms (Beta = .11). Turning to the second set of hypotheses, mental health symptoms were significantly associated with perceived difficulty in pursuing work (Beta = .28, p = .003), as was the summary index of the six obstacles identified as significant in bivariate analyses (Beta = .26, p = .009). The other three hypothesized paths to perceived difficulty were not supported: recency of employment (Beta = .06), physical health (Beta = .12), and substance use (Beta = −.01). Turning to interest in working, finally, the hypothesized association between perceived difficulty in pursuing work and utilization of vocational rehabilitation services was supported (Beta = −.31, p = .000); gender (male) was also a significant contributor to the utilization of such services (Beta = .21, p = .02). Results did not support the hypothesized path between interest in working and utilization of voc-rehab services (Beta = .07). (The full path model including causal paths representing our hypotheses, as well as paths consistent with the results of correlational analyses, is depicted in Figure 1.)
Figure 1.
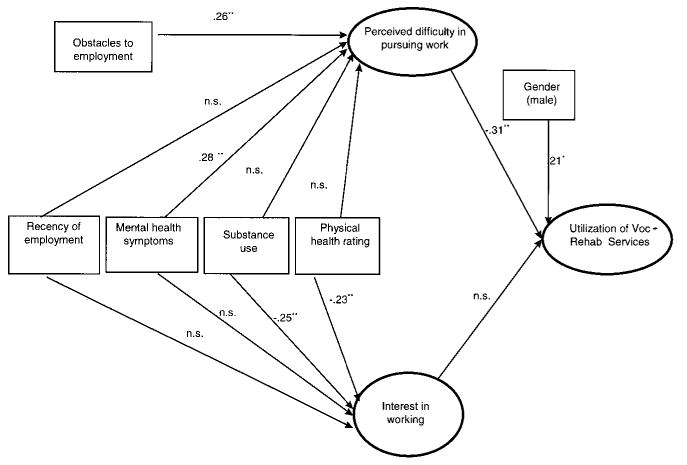
Path analysis model. *p<.05; **p<.01; n.s., not significant.
DISCUSSION
Our hypotheses received partial support only. With respect to the first group of hypotheses, substance use and physical health were significantly associated with interest in working, whereas mental health symptoms and recency of employment were not. That mental health was not significantly associated with interest in working is unexpected; the finding may be due in part to the instrument used to assess symptomatology or to the juxtaposition of time frames—symptoms in the past year vs. current interest in work. For persons with a long history of mental health symptoms, having experienced symptoms in the previous year is likely to be the norm and, as current findings suggest, may not affect the interest in pursuing employment as part of an effort to progress. The absence of a significant association between recency of employment and interest in working may be due to the distribution of the work history variable.
Of the hypothesized paths to perceived difficulty in pursing work, mental health, fear of failure, need for education and skills, impulse control, stigma, concerns about fitting in, and the need to stay in treatment all contributed to levels of perceived difficulty, whereas physical health, work history, and substance use did not. The use of a categorical variable for substance use in the analyses may have contributed to the finding reported here. The absence of a significant association between physical health and perceived difficulty is unexpected, especially since physical health was the second most frequently mentioned obstacle to the open-ended question and a strong contributor to interest in working. It may be that the rating of physical health status in the past month was not a stable enough measure to yield a significant association; for instance, if participants’ health fluctuates.
Finally, only one of our two hypothesized paths was supported with respect to the utilization of voc-rehab services. Perceived difficulty in pursuing work was associated with the utilization of services, whereas interest in working was not. One possible explanation for the latter finding may be that expressed interest in working in fact represents a desire to progress, a commitment to striving for the outcome society seems to value most: to become productive members of society. After abstinence has been achieved, individuals often report that “things aren’t happening fast enough” (60). The finding that interest in working was significantly higher among those who had maintained abstinence in the past year supports this conclusion.
Overall, study participants, most of whom had not worked in several years, were highly interested in pursuing employment but perceived multiple obstacles to doing so. In spite of their interest in employment, few have received voc-rehab services during the preceding year; this may be due to the high rate of involvement in outpatient services (scheduling conflicts with treatment were cited as an obstacle to employment). Exploratory analyses revealed a strong association between utilization of voc-rehab services at baseline and employment status 1 year later (r = .27, p = .00), suggesting that those who use voc-rehab services are actively preparing to pursue employment. While we cannot infer causation from cross-sectional data, the overall pattern of findings suggests that those who perceive more difficulty in employment and more obstacles in pursuit of employment may be less likely to utilize voc-rehab services and to become employed in the future. Fear of failure was often cited as an obstacle to pursuing employment. Bandura (43) has suggested that self-confidence develops through positive environmental interactions or personal experiences. In the area of work, dually diagnosed persons may have had few such experiences. Exposure to successful peers who can act as role models may partially compensate for this; attendance at dual-focus self-help groups, such as DTR, provides such contacts (in the overall sample, 20% of DTR members were employed).
The issue of employment among the dually diagnosed has not been adequately addressed in the literature and crucial questions remain. One issue is the low priority currently placed on the rehabilitative process for dually diagnosed persons. Perhaps this is due to the multitude of problems such clients may present, including high rates of hospitalization, HIV infection, homelessness, and violent behavior; such individuals are often difficult to treat, may appear noncompliant and unmotivated, and need specialized programs and assertive outreach (14,15). While there are a few programs that stress vocational outcomes for this target population, few program evaluations have been published and even fewer are methodologically sound (37). Thus, a second issue is the lack of well-designed evaluation studies of vocational programs for the dually diagnosed. One such study conducted in an assertive community treatment team for mental illness revealed no relationship between employment status and dual diagnosis (45). In recent years, most successful vocational rehabilitation innovations, developed in the mental health field, have been models that emphasize supported employment (i.e., permanent jobs in competitive and integrated work settings, with ongoing support). This model is now used by the federal and state vocational rehabilitation (VR) system across disabilities [e.g., (62,63)], and it appears to have considerable applicability to substance-using populations (14). Investigation of this model for the dually diagnosed needs to be undertaken. A third issue is that of assessment. The process must be ongoing and must go beyond determining clients’ skills, competencies, and needs; it also involves helping clients to examine their successes and decide on their next steps (and any possible changes in their vocational goals), as well as continuous practice in spotting potential problems [for discussion, see (14,50)].
The lack of emphasis in either service delivery or research on employment for dually diagnosed persons poses a challenge to the service providers. The current trend in treatment is increasingly toward integrated services where both mental health and “substance abuse” are addressed simultaneously (64), but the bulk of investigations about and the provision of voc-rehab services and employment have come from the mental health perspective. Clinicians may lack necessary information to address this topic; training is needed where staff are provided with empirically derived guidelines and strategies on whether, how, and at what time in the recovery process to encourage clients to consider employment. Clearly, these crucial clinical determinations must be made on an individual client basis [according to severity of disorders, recovery status, current skills and training, and past work history, among other criteria; for discussion, see (14)] but treatment providers need information to enhance the effectiveness of their decision. Areas where training is needed include how the two disorders interact over time, the course of recovery from dual-diagnosis, and where employment and work-readiness services fit in that process. Further, policy changes may be called for in the entitlement system. Although becoming more flexible (65), the disability benefits system still provides many disincentives to being employed [e.g., (11)]. Work is becoming a federally mandated right and norm for all citizens, whether or not they have disabilities or are economically deprived (i.e., American’s Disability Act (ADA) and welfare reform), and the system must strive to adapt. Increased flexibility is needed to allow a gradual transition to employment while preserving a safety net in terms of income and health insurance. Also, the system must not penalize those who may struggle in the work place and subsequently need to obtain benefits again. As a society, we must foster a climate where recovering persons feel supported in their employment goals, whatever they may be. We must also examine the assumptions underlying our assessment of employment outcomes and our widely held beliefs that “all work is good” and “more work is better.” Full-time employment should not be viewed as the ultimate goal and only measure of success for every recovering person. For example, there is evidence that part-time work may afford many of the recognized benefits of employment while minimizing stress [e.g., (66,67)].
Ultimately, the role of employment in recovery may be as much therapeutic as it is economic. The process and rate of recovery varies across individuals, as do level of skills, abilities, and goals; these differences must be considered. While work should be viewed as a normal part of clients’ lives and can be built upon as a strength in the rehabilitation process (14), individuals who are not ready should not feel pressured to become employed. Similarly, job termination (whether initiated by the employer or the employee) should not be viewed as failure, but instead used as a source of information about the individual’s readiness to work, and their existing and needed skills. When addressing employment with dually diagnosed persons, one must attempt to strike a balance between the potential risks and benefits of working to the recovering person. Dually diagnosed persons should be encouraged to seek employment if and when it can enhance recovery and overall functioning and quality of life. The authors hope that this study will stimulate other investigations on the important topic of employment among the dually diagnosed.
The present study has several strengths, including the investigation of an important yet largely neglected topic in the literature, and the use of an ethnically diverse sample of community-based individuals who represent different stages of dual-recovery as evidenced by their substance use and mental health status. Our study also has several limitations, including a large number of participants receiving treatment services, perhaps accounting for the low rate of utilization of voc-rehab services and limiting the generalizability of our findings. Further, self-reported substance use and mental health have limitations. However, empirical evidence suggests that self-reports of substance use among the dually diagnosed are reliable and valid as verified by collaterals [e.g., (68)]; the use of senior DTR members as interviewers is presumed to have enhanced the validity of reports. With respect to psychiatric diagnosis, cross-referencing of the reported prescribed medications was consistent with the diagnoses provided. Some of our measures are limited, including the use of a dichotomous variable to assess substance use and a single instrument to assess symptoms. Finally, the absence of a comparison group of individuals with a single disorder (either mental or substance use) did not allow us to obtain information on the specificity of the findings for the dually diagnosed.
Acknowledgments
The authors gratefully acknowledge the cooperation of the DTR members whose experiences contributed to this paper, as well as that of the agencies where the study participants were recruited.
The work reported here was supported by National Institute on Drug Abuse (NIDA) Grant R01 DA11240-01 (PI: S. Magura).
Biographies
Alexandre B. Laudet, Ph.D., a social psychologist, joined NDRI in 1994. Her research interests include the process of recovery from addiction over time—particularly after treatment—and factors contributing to the maintenance of lifelong recovery, such as affiliation with 12-step groups. She is also interested in cross-cultural perspectives on addiction and recovery.
Stephen Magura, Ph.D., C.S.W., is Director of the Institute for Treatment and Services Research at NDRI. He has designed and directed clinical trials of substance use interventions, treatment outcome studies, health services research, social epidemiology studies, HIV prevention research, and policy analysis. He has published more than 100 articles and authored/edited several books and special journal issues, including Experimental Therapeutics in Addiction Medicine and Program Quality in Substance Dependency Treatment.
Howard S. Vogel, C.S.W., C.A.S.A.C., is the Executive Director of Double Trouble in Recovery. Mr. Vogel has recently been appointed Deputy Director of Dual-Diagnosed Affairs at the Mental Health Empowerment Project, Inc., in NewYork State. He is a graduate of Hunter Graduate School of Social Work, holds a C.A.S.A.C. from the Office of Alcoholism and Substance Abuse in NewYork State, and is currently a consultant for NDRI.
Edward L. Knight, Ph.D., received his Ph.D. in Sociology in 1979 from the Graduate Faculty of the New School for Social Research in NewYork. He is a researcher with several National Institutes of Mental Health (NIMH)-funded research centres. He trains mental health professionals in recovery in serious mental illness, rehabilitation, and mutual support, run by peers, not professionals. He consults with managed care companies and mental health state authorities. He is diagnosed with schizophrenia and has been homeless.
References
- 1.Room JA. Work and Identity in Substance Abuse Recovery. J Subst Abuse Treat. 1998;15(1):65–74. doi: 10.1016/s0740-5472(97)00250-x. [DOI] [PubMed] [Google Scholar]
- 2.Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of Mental Disorders with Alcohol and Other Drug Abuse. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- 3.Hubbard RL, Marsden ME, Rachal JV, Harwood HJ, Cavanaugh ER, Ginzburgh HM. Drug Abuse Treatment: A National Study of Effectiveness. University of North Carolina Press; Chapel Hill, NC: 1989. [Google Scholar]
- 4.Platt JJ. Vocational Rehabilitation of Drug Abusers. Psychol Bull. 1995;117(3):416–423. doi: 10.1037/0033-2909.117.3.416. [DOI] [PubMed] [Google Scholar]
- 5.Platt JJ, Widman M, Lidz V, Rubenstein D, Thompson R. The Case for Support Services in Substance Abuse Treatment. Am Behav Sci. 1998;41(8):1050–1062. [Google Scholar]
- 6.Jenner M. Harm Minimization Outcomes for Methadone Recipients: Role of Employment. J Subst Misuse . 1998;3(2):114–118. [Google Scholar]
- 7.Cook A, Razzano L. Vocational Rehabilitation for Persons with Schizophrenia: Recent Research and Implications for Practice. Schizophr Bull. 2000;26:87–103. doi: 10.1093/oxfordjournals.schbul.a033448. [DOI] [PubMed] [Google Scholar]
- 8.Hammer T, Ravndal E, Vaglum P. Work is Not Enough: A Quasi-experimental Study of a Vocational Training Program for Young Drug Abusers. J Drug Issues. 1985;15:393–403. [Google Scholar]
- 9.Drake RE, McHugo GJ, Becker DR, Anthony WA, Clark RE. The New Hampsh ire Study of Supported Employment for People with Severe Mental Illness. J Consult Clin Psychol. 1996;64(2):391–399. doi: 10.1037//0022-006x.64.2.391. [DOI] [PubMed] [Google Scholar]
- 10.Fellin P. Reformulation of the Context of Community Based Care. J Sociol Soc Welf. 1993;20:57–67. [Google Scholar]
- 11.Harding CM. Some Things We’ve Learned About Vocational Rehabilitation of the Seriously and Persistently Mentally Ill. Presented at the Boston University Colloquium; Brookline, MA. April 17, 1996. [Google Scholar]
- 12.Haynes R, Gantt A. Patient Psychoeducation: The Therapeutic Use of Knowledge for the Mentally Ill. Soc Work Health Care. 1992;17:53–67. doi: 10.1300/J010v17n01_04. [DOI] [PubMed] [Google Scholar]
- 13.Mueser K, Becker D, Torrey W. Work and Nonvocational Domains of Functioning in Persons with Severe Mental Illness: A Longitudinal Analysis. Journal of Nervous and Mental Disorders. 1997;18(5):419–426. doi: 10.1097/00005053-199707000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Blankertz L, McKay C, Robinson S. Work as a Rehabilitative Tool for Individuals with Dual Diagnosis. J Vocat Rehabil. 1998;11:113–123. [Google Scholar]
- 15.Drake RE, Osher FC. Treating Substance Abuse in Patients with Severe Mental Illness. In: Henggeler SW, Santos AB, editors. Innovative Approaches for Difficult-to-Treat Populations. American Psychiatric Press; Washington, DC: 1997. [Google Scholar]
- 16.McGurrin MC. An Overview of the Effectiveness of Traditional Vocational Rehabilitation Services in the Treatment of Long Term Mental Illness. Psychosoc Rehabil J. 1994;17:37–54. [Google Scholar]
- 17.Noble JH, Honberg RS, Hall LL, et al. A Legacy of Failure: The Inability of the Federal-State Vocational Rehabilitation System to Serve People with Severe Mental Illnesses. National Alliance for the Mentally Ill; Arlington, VA: 1997. [Google Scholar]
- 18.Knoedler W. How Training in Community Living Helps its Patient. New Dir Ment Health Serv. 1979;50:43–56. [Google Scholar]
- 19.Sciacca K. An Integrated Treatment Approach for Severely Mentally Ill Individuals with Substance Disorders. New Dir Ment Health Serv. 1991;50:69–84. doi: 10.1002/yd.23319915008. [DOI] [PubMed] [Google Scholar]
- 20.Solomon P, Draine J. Subjective Burden of Family Members of Mentally Ill Adults: Relation to Stress, Coping, and Adaptation. Am J Orthopsychiatry. 1995;65:419–427. doi: 10.1037/h0079695. [DOI] [PubMed] [Google Scholar]
- 21.Bell M, Lysaker P, Milstien R. Clinical Benefits of Paid Work in Schizophrenia. Schizophr Bull. 1996;22:51–67. doi: 10.1093/schbul/22.1.51. [DOI] [PubMed] [Google Scholar]
- 22.Minko K. Program Components of Comprehensive Integrated Care System for Serious Mentally Ill Patients with Substance Disorders. New Dir Ment Health Serv. 1991;50:13–28. doi: 10.1002/yd.23319915004. [DOI] [PubMed] [Google Scholar]
- 23.Friedman AS, Granick S, Bransfield S, Kreisher C, Schwartz A. The Consequences of Drug Use/Abuse for Vocational Career: A Longitudinal Study of a Male Urban African-American Sample. Am J Drug Alcohol Abuse . 1996;22(1):57–73. doi: 10.3109/00952999609001645. [DOI] [PubMed] [Google Scholar]
- 24.Gardiner JC. Vocational Characteristics of Substance Abusers Admitted to a Therapeutic Community. In: Schecter AJ, editor. Drug Dependence and Alcoholism, Vol 2 Social and Behavioral Issues. NewYork: Plenum Press; 1978. pp. 497–510. [Google Scholar]
- 25.Harley DA, Maxwell CH. Improving Employment Outcomes for Chronic Alcoholics: Applying the Supported Employment Model. Int J Addict. 1994;29(5):667–673. doi: 10.3109/10826089409047407. [DOI] [PubMed] [Google Scholar]
- 26.Lamb R, Kirby J, Kimberly C, Platt JJ. Treatment Retention, Occupational Role, and Cocaine Use in Methadone Maintenance. Am J Addict. 1996;5(1):12–17. [Google Scholar]
- 27.Schottenfeld RS, Pascale R, Sokolowski S. Matching Services to Needs: Vocational Services for Substance Abusers. J Subst Abuse Treat. 1992;9:3–8. doi: 10.1016/0740-5472(92)90003-7. [DOI] [PubMed] [Google Scholar]
- 28.National Institute on Disability and Rehabilitation Research. NIDRR Consensus Validation Conference: Strategies to Secure and Maintain Employment for Persons with Long-Term Mental Illness. Department of Education; Washington, DC: 1992. [Google Scholar]
- 29.Lehman A. Vocational Rehabilitation in Schizophrenia. Schizophr Bull. 1995;21:645–656. doi: 10.1093/schbul/21.4.645. [DOI] [PubMed] [Google Scholar]
- 30.Ridgeway P, Rapp C. The Active Ingredients in Achieving Competitive Employment for People with Psychiatric Disabilities: A Research Synthesis. In: Lawrence KS, editor. Commission on Mental Health and Developmental Disabilities (Critical Ingredients Series) 1998. [Google Scholar]
- 31.Swartz J, Lurigio A, Goldstein P. Severe Mental Illness and Substance Use Disorders Among Former Supplemental Security Income Beneficiaries for Drug Addiction and Alcoholism. Arch Gen Psychiatry . 2000;57(7):701–707. doi: 10.1001/archpsyc.57.7.701. [DOI] [PubMed] [Google Scholar]
- 32.Goldberg R, Lucksted A, Mcnary S, Gold J, Dixon L, Lehman A. Correlates of Long-Term Employment Among Inner-City Adults with Serious and Persistent Mental Illness. Psychiatr Serv. 2001;52(1):101–103. doi: 10.1176/appi.ps.52.1.101. [DOI] [PubMed] [Google Scholar]
- 33.Sainfort F, Becker M, Diamond R. Judgements of Quality of Life of Individuals with Severe Mental Disorders: Patients’ Self-Report vs. Providers’ Perspectives. Am J Psychiatry. 1996;4:497–502. doi: 10.1176/ajp.153.4.497. [DOI] [PubMed] [Google Scholar]
- 34.Boykin Q. Parting Words. NYC Office of Consumer Affairs. From the Edge . 1998;2(1):16. [Google Scholar]
- 35.Harding CM, Brooks GW, Ashikaga T, Strauss JS, Landerl PD. Aging and Social Functioning in Once-Chronic Schizophrenic Patients 22–62 Years After First Admission: The Vermont Story. In: Miller N, Cohen GD, editors. Schizophrenia and Aging. Guildford Press; NewYork: 1987. pp. 160–166. [Google Scholar]
- 36.Arella LR, Deren S, Randell J, Brewington V. Structural Factors that Affect Provisions of Vocational/Education Services in Methadone Maintenance Treatment Programs. J Appl Rehabil Couns. 1990;21:19–26. [Google Scholar]
- 37.Dennis ML, Karuntzos GT, McDougal GL, French MT, Hubbard RL. Developing Training and Employment Programs to Meet the Needs of Methadone Treatment Clients. Eval Program Plann. 1993;16:73–86. [Google Scholar]
- 38.French MT, Dennis MI, McDougal GL, Karuntzos GT, Hubbard RL. Training and Employment Programs in Methadone Treatment: Client Needs and Desires. J Subst Abuse Treat. 1992;9(4):293–303. doi: 10.1016/0740-5472(92)90022-g. [DOI] [PubMed] [Google Scholar]
- 39.Hubbard R, Harwood H. Employment Related Services in Drug Treatment Programs. Research Triangle Institute; Research Triangle Park, NC: 1981. [Google Scholar]
- 40.Surgeon General. Mental Health: A Report of the Surgeon General. U.S. Public Health Office; Rockville, MD: 2000. [Google Scholar]
- 41.Hazelden . National Survey on Attitudes About Addiction. Hazelden Foundation; Center City, MN: 1999. [Google Scholar]
- 42.Leete E. HowI Perceive and Manage my Illness. Schizophr Bull. 1989;15(2):197–200. doi: 10.1093/schbul/15.2.197. [DOI] [PubMed] [Google Scholar]
- 43.Bandura A. Self-efficacy: Toward a Unifying Theory of Behavioural Change. Psychol Rev. 1997;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 44.Estro S. No Other Way to Go: Application for Disability Income Among Persons with Severe Mental Illness. In: Bonnie R, Monahan J, editors. Mental Disorder, Work Disability and the Law. University of Chicago Press; Chicago, IL: 1997. [Google Scholar]
- 45.Meisler N, Blackertz L, McKay C, Santos A. Impact of Assertive Community Treatment on Homeless Persons with Co-occurring Severe Psychiatric and Substance Use Disorders. Community Ment Health J. 1997;33:113–122. doi: 10.1023/a:1022419316396. [DOI] [PubMed] [Google Scholar]
- 46.Fabian ES. Longitudinal Outcomes in Supported Employment: A Survival Analysis. Rehabil Psychol. 1992;37:23–36. [Google Scholar]
- 47.Anthony WA, Jansen MA. Predicting the Vocational Capacity of the Chronically Mentally Ill: Research and Implications. Am Psychol. 1984;39:537–544. doi: 10.1037//0003-066x.39.5.537. [DOI] [PubMed] [Google Scholar]
- 48.Ferdinandi A, Yootanasumpun V, Pollack S, Bermanzohn P. Rehab Rounds: Predicting Rehabilitation Outcome Among Patients with Schizophrenia. Psychiatr Serv. 1998;49:907–909. doi: 10.1176/ps.49.7.907. [DOI] [PubMed] [Google Scholar]
- 49.Bond GR, Dietzen L. Predictive Validity and Vocational Assessment: Reframing the Question. In: Glueckauf RL, Sechrest LB, Bond GR, McDonel EC, editors. Improving Assessment in Rehabilitation and Health. Sage; Newbury Park, CA: 1993. pp. 61–86. [Google Scholar]
- 50.Becker D, Drake R, Bond G, Xie H, Dain B, Harrisson K. Job Terminations Among Persons with Severe Mental Illness Participating in Supported Employment. Community Ment Health J. 1998;34(1):71–82. doi: 10.1023/a:1018716313218. [DOI] [PubMed] [Google Scholar]
- 51.Brewington V, Deren S, Arella I, Randell J. Obstacles to Vocational Rehabilitation: The Clients’ Perspectives. J Appl Rehabil Couns. 1990;21:27–37. [Google Scholar]
- 52.Platt JJ, Metzger D. The Role of Employment in the Rehabilitation of Heroin Addicts. In: Ashery RS, editor. Progress in the Development of Cost Effective Treatment for Drug Abusers. National Institute on Drug Abuse; Rockville, MD: 1985. pp. 111–121. [Google Scholar]
- 53.McCory D. The Human Dimension of the Vocational Rehabilitation Process. In: Ciardiello JA, Bell MD, editors. Vocational Rehabilitation of Persons with Prolonged Psychiatric Disorders. Johns Hopkins University Press; Baltimore, MD: 1988. pp. 59–80. [Google Scholar]
- 54.Minko K. An Integrated Treatment Model for Dual Diagnosis of Psychosis with Addiction. Hosp Community Psychiatry. 1989;40:1031–1036. doi: 10.1176/ps.40.10.1031. [DOI] [PubMed] [Google Scholar]
- 55.Anthony W, Rogers E, Davies R. Relationships Between Psychiatric Symptomatology, Work Skills and Future Vocational Performance. Psychiatr Serv. 1995;46:353–358. doi: 10.1176/ps.46.4.353. [DOI] [PubMed] [Google Scholar]
- 56.Bond GR, Becker DR, Drake RE, Vogler KM. A Fidelity Scale for the Individual Placement and Support Model of Supported Employment. Rehabil Couns Bull. 1997;40(4):265–284. [Google Scholar]
- 57.Drake RE, Becker DR, Biesanz JC, Torrey WC, McHugo GJ, Wyzik PR. Rehabilitative Day Treatment Versus Supported Employment: I. Vocational Outcomes. Community Ment Health J. 1994;30:519–532. doi: 10.1007/BF02189068. [DOI] [PubMed] [Google Scholar]
- 58.Vogel HS, Knight E, Laudet AB, Magura S. Double Trouble in Recovery: Self-Help for the Dually-Diagnosed. Psychiatr Rehabil J. 1998;21(4):356–364. doi: 10.1037/h0095288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shern DL, Wilson NZ, Coen AS. Client outcomes II: Longitudinal Client data from the Colorado Treatment Outcome Study. The Milbank Quarterly. 1994;72:123–148. [PubMed] [Google Scholar]
- 60.Laudet A, Magura S, Vogel H, Knight E. Recovery Challenges Among Dually-Diagnosed Individuals. J Subst Abuse Treat. 2000;18(4):321–329. doi: 10.1016/s0740-5472(99)00077-x. [DOI] [PubMed] [Google Scholar]
- 61.Carpinello SE, Knight EL. A Qualitative Study of the Perceptions of the Meaning of Self-Help by Self-Help Group Leaders, Members, and Significant Others. NewYork State Office of Mental Health Bureau of Evaluation and Services Research; 1991. [Google Scholar]
- 62.Keel J, Mesibov G, Woods A. TEACCH—supported employment programs. J Autism Dev Disord. 1997;27(1):3–9. doi: 10.1023/a:1025813020229. [DOI] [PubMed] [Google Scholar]
- 63.Unger D. Workplace Supports: A View from Employers Who Have Hired Supported Employees. Focus on Autism and Other Developmental Disabilities . 1999;14(3):167–179. [Google Scholar]
- 64.Rosenthal RN, Hellerstein DJ, Miner CR. A Model of Integrated Services for Outpatient Treatment of Patients with Comorbid Schizophrenia and Addictive Disorders. Am J Addict. 1992;1(4):339–348. [Google Scholar]
- 65.Noble J. Policy Reform Dilemmas in Promoting Employment of Persons with Severe Mental Illness. Psychiatr Serv. 1998;49:775–781. doi: 10.1176/ps.49.6.775. [DOI] [PubMed] [Google Scholar]
- 66.Arnold R. Employment and Disability. Psychiatr Serv. 1999;49:1361. doi: 10.1176/ps.49.10.1361. [DOI] [PubMed] [Google Scholar]
- 67.Fodora Elliott E. Employment Disability. Psychiatr Serv. 1999;50:1640. doi: 10.1176/ps.50.12.1640-a. [DOI] [PubMed] [Google Scholar]
- 68.Stasiewicz P, Bradizza C, Connors G. Subject Collateral Reports of Drinking in Inpatient Alcoholics with Comorbid Mental Disorders. Alcohol Clin Exp Res. 1997;21(3):530–536. [PubMed] [Google Scholar]


