Abstract
A large percentage of individuals are dually-diagnosed with a psychiatric disorder and a substance use disorder. Such persons typically face more difficulties and have poorer outcomes than do single disorder substance users. Among noncomorbid substance users, treatment and participation in 12-Step groups have been shown to enhance the likelihood of abstinence from substance misuse. Specialized 12-Step based fellowships have recently emerged to address the recovery needs of dually-diagnosed persons. The present study is a longitudinal investigation of the effect of such 12-Step based groups on abstinence among dually-diagnosed persons. Participants were members of Double Trouble in Recovery (DTR) who were recruited at community-based meetings in New York City and reinterviewed twice at yearly intervals. Generalized estimating equation analysis indicated that, over the two-year study period, ongoing DTR attendance was significantly associated with a greater likelihood of abstinence after controlling for other pertinent variables, such as mental health symptoms. For clinicians, these findings underline the importance of fostering stable affiliation with specialized 12-Step based groups among their clients.
Keywords: comorbidity, dual diagnosis, recovery, self help, substance use, 12-Step
The rate of co-occurring substance misuse and psychiatric disorders is high (e.g., Kessler 1995). Persons with such a dual diagnosis typically have poorer outcomes (e.g., Gonzalez & Rosenheck 2002) and have increased vulnerability to difficulties in a broad array of life domains including physical health, social relations, and housing (Clark 1994; Bartels et al. 1993). For example, the McKinney Demonstration Projects for homeless mentally ill adults reported that substance use disorders were the single most important factor contributing to housing instability in this population (Center for Mental Health Services 1994). Dually-diagnosed persons also appear to face more challenges in recovery than do single disorder substance users (e.g., Laudet et al. 2000a). Overall, identifying interventions that promote abstinence among dually-diagnosed persons can enhance the likelihood of positive outcomes and decrease the risk of the negative consequences attendant to substance use.
Participation in treatment has been associated with reduction in substance use and improvements in other areas of functioning among dually-diagnosed persons (e.g., Gonzalez & Rosenheck 2002). It is generally believed that the duration of services for such clients should be extensive as “experience with dually diagnosed patients supports the need for a long-term perspective” (Drake et al. 1993).
With the advent of managed care and resulting decreases in both duration and intensity of formal treatment, researchers and service providers have been increasingly interested in community-based resources to augment support for recovery both during and after treatment. This is particularly important for dually-diagnosed persons who may need more support for a longer time than do single disorder substance users.
Twelve-Step fellowships such as Alcoholics and Narcotics Anonymous are a widely available, cost-free recovery resource. Participation in 12-Step groups has been found to be associated with greater likelihood of abstinence (Florentine & Hillhouse 2000; Laudet et al. 2000b; Timko et al. 2000; Humphreys et al. 1999; Moos et al. 1999; McCrady & Miller 1993). One of the major tenets of 12-Step programs is that addiction is a lifelong condition and that recovery requires ongoing participation in 12-Step meetings (e.g., Kingree 1995; Morgenstern & McCrady 1993). Empirical findings from a post-treatment follow-up study among illicit drug users speak to the importance of consistent 12-Step attendance in maintaining abstinence: The 40% of participants who attended 12-Step groups consistently over a two-year study period maintained a high rate of abstinence, whereas abstinence rates dropped significantly among the 26% of subjects who stopped attending (Fiorentine 1999).
The effectiveness of participation in 12-Step groups among dually-diagnosed persons has received little empirical attention. Available reports suggest that the benefits of 12-Step group participation may extend to clients with a comorbid psychiatric disorder (e.g., Gonzalez & Rosenheck 2002; Moos et al. 2001, 1999; Ouimette, Finney, and Moos 1997; Jerrell & Ridgely 1995). However, the American Psychiatric Association (1995) has recommended that dually-diagnosed persons who take psychoactive medications be referred to support groups where such therapy is recognized and encouraged as useful, rather than possibly questioned or criticized. (The authors note that this recommendation is somewhat inconsistent with the 12-Step program’s “singleness of purpose” whereby members who attend 12-Step meetings because they wish to stop drinking or using drugs are encouraged to limit their discussion to substance-related problems, so that psychiatric medication regimens would not necessarily be mentioned and thus not be subject to criticism.) Two 12-Step based fellowships have emerged specifically to address dual-diagnosis recovery needs: Dual Recovery Anonymous (DRA; see Hazelden 1993; http://draonline.org) and Double Trouble in Recovery (DTR; Vogel et al. 1998; www.doubletroubleinrecovery.org). The few studies examining participation in dual-focus 12-Step based groups have reported satisfactory participation rates (e.g., Powell et al. 1996; Kurtz et al. 1995). These groups provide members with an opportunity to discuss both substance use and mental health issues, including the use of medications, in an accepting and psychologically safe forum. The present study uses a repeated measures model to conduct a longitudinal investigation of the effectiveness of participation in 12-Step based dual-focus groups for achieving abstinence from alcohol and drugs. The primary hypothesis examined here is that length of attendance at 12-Step based dual-focus groups will be associated with a greater probability of abstinence, independent of other factors that may be associated with abstinence. The secondary hypotheses are that: (a) participation in formal treatment and (b) participation in traditional 12-Step groups will be associated with greater probability of abstinence, independent of other relevant factors.
METHODS
Setting
Study participants were recruited from persons attending Double Trouble in Recovery (DTR) meetings throughout New York City. DTR is a mutual aid fellowship adapted from the 12-Step program of recovery, specifically embracing those who are dually-diagnosed with a psychiatric illness and a substance use disorder (Vogel et al. 1998). DTR was started in New York State in 1989 and currently has approximately 200 groups meeting in the U.S., with the most groups currently in New York, Georgia, Colorado, New Mexico and Florida. New DTR groups continue to be started, some initiated by dually-diagnosed persons and others by professionals who believe that mutual help fellowships are a useful complement to formal treatment. DTR, Inc., a small nonprofit organization, supports this growth by training recovering persons to start and conduct groups and by providing ongoing support to existing groups. DTR developed as a grassroots initiative and functions today with minimal involvement from the professional community; it is not affiliated with AA or with any other 12-Step fellowship. Groups meet in community-based organizations, psychosocial clubs, outpatient treatment programs for mental health, substance abuse and dual-diagnosis, and inpatient psychiatric hospital units. All meetings are led by recovering individuals and follow the format of other 12-Step fellowship meetings—most often, round-robin or speaker meetings. At this writing, this relatively new fellowship is in the process of formalizing its own 12-Step dual-diagnosis recovery program including efforts to encourage sponsorship and step work among its members. The 12-Steps of DTR are those used by other 12-Step organizations, adapted to dual diagnosis in Step One (“We admitted we were powerless over our menial disorders and substance abuse and that our lives had become unmanageable.”) and Step Twelve (“Having had a spiritual awakening as a result of these steps, we tried to carry this message to other dually-diagnosed people and to practice these principles in all our affairs.”).
Participants
Prospective study participants were recruited at 24 DTR meetings (10 to 20 members at each) held in community-based organizations and day treatment programs throughout New York City. Study staff went to the various meetings, explained the study to members, and invited all members to participate in the study, with the only requirement being that they had to be attending DTR for at least one month. Of the total of 360 attendees counted at these meetings, 16 were ineligible due to less than one month of attendance, and 34 declined participation, either immediately or when they were subsequently contacted for an interview. Three hundred and ten DTR members agreed to participate. Thus, about six out of seven DTR attendees (310/360–86%) participated in the study. The main reasons for declining were a concern about confidentiality (especially for meetings held in treatment facilities), interview length, and scheduling conflicts among persons attending intensive day treatment programs. Participation was voluntary based on informed consent; the NDRI Institutional Review Board approved the study. The study employed as interviewers several trusted members of the DTR fellowship who received training in interview skills and were closely supervised in their research activities. Baseline interviews were conducted between January and December of 1998; 276 one-year follow-up interviews were conducted between January and December of 1999, representing a 90% recontact rate (four participants died). Reasons for no follow-up were: unable to locate or contact (19), refused (six), residential treatment out of state (four), and incarcerated (one). Two-hundred and thirty-three of the 276 participants were reinterviewed at the two-year follow-up between January and December 2000, representing a two-year recontact rate of 76% (233/306) of those remaining alive).1 The interviews took about two hours; participants received $35 at baseline and $40 for each of the follow-up interviews.
Study Measures
The interview was a semistructured instrument administered at study intake (“baseline”), one year later (“one year follow-up”) and two years later (“two year follow-up”). In addition to sociodemographics, background and self-reported psychiatric diagnoses, the study used the following measures:
DTR attendance. The number of months participants attended DTR in the year before each interview.
Substance use. At each interview, participants were asked about their use of each of 11 substances (e.g., alcohol, marijuana/grass, crack/rock) in the previous year, following the format of the Addiction Severity Index (McLellan et al. 1992). A summary variable was created to indicate abstinence from all drugs of abuse and alcohol (yes/no) at each time point
Formal treatment for mental illness and/or substance abuse. The authors initially intended to examine the influence of both outpatient and inpatient treatment on substance use. However, almost all participants were enrolled in outpatient services at both follow-up assessments (97% at one-year follow-up and 94% at two-year follow-up), resulting in too little variance to allow outpatient treatment to be included in the analysis. (Services included in outpatient services were: outpatient treatment for dual diagnosis, mental health only and substance use only, as well as individual counseling.) The treatment variable used in the analyses was any inpatient treatment in the prior year at the one- and two-year follow-ups (yes/no).
Attendance at traditional 12-Step meetings. Frequency of attendance at Alcoholics Anonymous (AA), Narcotics Anonymous (NA), and/or Cocaine Anonymous (CA) in the year preceding each interview was coded as 0 = none, 1 = once a month, 2 = every other week, 3 = about once a week, 4 = more than once a week.
Problem severity has been found to be associated with poorer outcomes among single disorder substance misusers (e.g., Simpson et al, 1999). Several historical measures of drug use and mental health problem severity were included:
Primary substance of abuse. At baseline, participants were asked which substance had been their major problem, coded as cocaine/crack, alcohol, heroin, marijuana, or “other” substance.
Age of onset of substance misuse. Number of years of substance use is sometimes used as a measure of addiction severity (e.g., McLellan et al. 1992); that measure is largely dependent on participants’ age at the time of the interview. Therefore, a less biased measure of severity was selected, namely age at substance use initiation. At the baseline interview, participants were asked the age at which they initiated regular substance misuse.
Hospitalizations for substance misuse. This was self-reported at baseline among participants who reported hospitalization as more than five times or less than Five times. (In pre-testing of the instrument, participants had difficulty repotting the total number of hospitalizations; the authors arrived at the current item phrasing after discussing the issue with DTR members as well as with treatment professionals.)
Mental health symptoms. The Colorado Symptoms Index (CSI), a scale developed specifically for persons diagnosed with severe and persistent mental illness (Shern et al. 1994), was used to measure symptoms. For this study, the index is the number of the 13 symptoms (e.g., have you felt depressed? have you felt like seriously hurting someone?) experienced in the year before each interview (Alpha = .86 at both interviews).
Hospitalizations for mental health problems. This was reported at baseline among participants who reported mental health hospitalization, as more than five times and less than five times (see note above concerning hospitalizations for substance misuse).
Timing of Interviews
While interviews were scheduled at yearly intervals one and two years after baseline, a small number of participants were interviewed earlier (e.g., because they were about to move out of state) or were difficult to locate so that they were interviewed somewhat later than required by the study design. Advanced techniques for longitudinal analysis (described below) allow the exact interval between interviews to be taken into account. The mean number of days between the baseline and the one-year follow-up interviews was 380 (SD = 40 days, range = 321 to 622 days) and 745 days between the baseline and two year follow-up interviews (SD = 41 days, range = 618 to 1004 days).
Analysis Plan and Statistical Techniques
The first step in the analyses was to describe the associations of demographic variables, psychiatric diagnosis, past abstinence, traditional 12-Step, formal treatment, and DTR attendance with abstinence during each follow-up period. Zero-order (bivariate) correlations describe the relation between a single predictor and dependent variable when that single predictor is not required to compete with other predictors. Unique relations indicate whether a single variable can add to the prediction of the dependent variable when all other predictors have been controlled. Thus, a predictor may be significantly correlated with a dependent variable yet not be uniquely related to that variable, particularly if the information it provides is redundant with that provided by other predictors. For that reason, we examined both correlations and unique relations between hypothesized predictors and outcome variables.
In the next step, multivariate analyses were conducted to examine the unique effects of time, DTR attendance, and other variables on abstinence. Generalized estimating equations (GEE) are an appropriate analytic tool when a dichotomous outcome variable is observed longitudinally (Liang & Zeger 1986; Zeger & Liang 1986). In this study, GEE analysis allows for all of the available observations to be used, and it summarizes the unique effects of time, DTR attendance, and other variables on abstinence. Variables which were not related to abstinence during one or both follow-up periods were not included in the GEE analysis. All analyses were performed using PROC GENMOD, a module of the SAS (1999) data analysis package, which implements generalized estimating equations.
For some of the variables considered as potential predictors of abstinence, a small amount of the data was missing (up to but never exceeding 3%). In order to maintain a constant sample size in the regression modeling, missing values were imputed. For continuous and discrete predictors, missing values were replaced with a random sample from the nonmissing cases.
RESULTS
The sample was 73% male; 58% Black, 25% White, 14% Hispanic, and 3% other ethnicity. At the baseline interview, mean age was 40.8 years (SD = 8.5), ranging from 20 to 63 years. Sixty-one percent graduated from high school or received a GED. Self-reported primary psychiatric diagnoses were: schizophrenia (39%), major depression (20%), bipolar (20%), other (21%). The primary substance of abuse reported by participants was: cocaine/crack (39%); alcohpl (35%), heroin (12%), marijuana (11%), other (3%).
Participants followed-up and lost to follow-up were compared on age, gender, ethnicity, primary substance of abuse, primary psychiatric diagnosis, and on DTR attendance, number of mental health symptoms, mental health symptom severity, and substance use prior to baseline. When compared with those not followed-up, participants followed-up were less likely to have reported substance use in the year before baseline (r = −.15), had attended DTR for a longer time before baseline (r = .11), and were less likely to report cocaine/crack than other substances as a primary drug (r = .14).
Descriptive statistics, zero-order and unique relations of background and hypothesized predictor variables with abstinence at each follow-up are presented in Tables 1 and 2. For ease of presentation, age, DTR attendance, mental health symptoms, and age of onset of substance misuse are shown and analyzed as categorical variables with three or four levels in Tables 1 and 2. (Continuous variables are used in the analyses presented in Table 3.)
TABLE 1.
Longitudinal Relation of Background Characteristics, Formal Treatment, Traditional 12-Step, and DTR to Abstinence at One-Year Follow-Up: Zero-Order and Unique Effects (N=276)
| % Abstinent | χ2 (Zero-Order) | χ2 (Unique) | |
|---|---|---|---|
| Gender | |||
| Female (27%) | 72 | 0.15 | 2.23 |
| Male (73%) | 70 | ||
| Age | |||
| 20–36(35%) | 66 | 2.11 | 0.13 |
| 37–43(28%) | 69 | ||
| 44–64(37%) | 75 | ||
| High school graduate/GED | |||
| Yes (61%) | 72 | 0.94 | 1.16 |
| No (39%) | 67 | ||
| Race/ethnicity | |||
| African-American (58%) | 71 | 3.09 | 6.27 |
| White (24%) | 64 | ||
| Hispanic (14%) | 72 | ||
| Other (3%) | 89 | ||
| Primary MH diagnosis | |||
| Schizophrenia (39%) | 67 | 2.33 | 8.14* |
| Unipolar depression (20%) | 70 | ||
| Bipolar depression (20%) | 78 | ||
| Other (21%) | 70 | ||
| Mental health hospitalizations | |||
| Less than five (51%) | 71 | 0.06 | 0.08 |
| Five or more (49%) | 70 | ||
| Primary substance of abuse | |||
| Cocaine/crack (39%) | 64 | 10.02* | 14.69** |
| Alcohol (35%) | 69 | ||
| Heroin (12%) | 78 | ||
| Marijuana (11%) | 80 | ||
| Other (3%) | 100 | ||
| Age of onset of substance misuse | |||
| Less than 14 (29%) | 74 | 4.02 | 10.20* |
| 14–15(29%) | 65 | ||
| 16–19(30%) | 68 | ||
| 20 or greater (12%) | 81 | ||
| Substance use hospitalizations | |||
| Less than five (74%) | 69 | 1.06 | 1.03 |
| Five or more (26%) | 75 | ||
| 12-Step attendance (base - F1) | |||
| None (28%) | 68 | 1.29 | 5.31 |
| About once a month (3%) | 67 | ||
| Every other week (6%) | 75 | ||
| About once a week (21%) | 67 | ||
| More than once a week (42%) | 73 | ||
| Any inpatient treatment (base - F1) | |||
| Yes (21%) | 59 | 4.59* | 1.23 |
| No (79%) | 73 | ||
| MH symptoms (base - F1) | |||
| 0–3(34%) | 84 | 14.53** | 16.80** |
| 4–7(29%) | 68 | ||
| 8–13 (37%) | 60 | ||
| DTR attendance (base - F1) | |||
| 0–5 Months (17%) | 52 | 11.69** | 8.72* |
| 6–11 Months (21%) | 64 | ||
| 12 Months (62%) | 77 | ||
| Abstinence in the year before baseline | |||
| Yes (54%) | 85 | 33.13** | 27.41** |
| No (46%) | 53 | ||
P<.05.
P<.01.
TABLE 2.
Longitudinal Relation of Background Characteristics, Formal Treatment, Traditional 12-Step, and DTR to Abstinence at Two-Year Follow-Up: Zero-Order and Unique Effects (N=233)
| % Abstinent | χ2 (Zero-Order) | χ2 (Unique) | |
|---|---|---|---|
| Gender | |||
| Female (27%) | 78 | 0.72 | 1.10 |
| Male (73%) | 72 | ||
| Age | |||
| 20–36 (34%) | 76 | 1.08 | 2.61 |
| 37–43 (29%) | 69 | ||
| 44–64 (37%) | 76 | ||
| High school graduate/GED | |||
| Yes (64%) | 76 | 0.72 | 0.29 |
| No (36%) | 71 | ||
| Race/ethnicity | |||
| African-American (58%) | 78 | 5.66 | 5.50 |
| White (25%) | 69 | ||
| Hispanic (13%) | 60 | ||
| Other (4%) | 89 | ||
| Primary MH diagnosis | |||
| Schizophrenia (40%) | 73 | 0.67 | 1.92 |
| Unipolar depression (19%) | 73 | ||
| Bipolar depression (20%) | 78 | ||
| Other (21%) | 71 | ||
| Mental health hospitalizations | |||
| Less than five (51%) | 71 | 0.72 | 1.39 |
| Five or more (49%) | 76 | ||
| Primary substance of abuse | |||
| Cocaine/crack (38%) | 73 | 5.57 | 8.56 |
| Alcohol (36%) | 73 | ||
| Heroin (11%) | 72 | ||
| Marijuana (11%) | 88 | ||
| Other (4%) | 50 | ||
| Age of onset of substance misuse | |||
| Less than 14 (28%) | 76 | 1.04 | 0.25 |
| 14–15(28%) | 74 | ||
| 16–19(33%) | 70 | ||
| 20 or greater (10%) | 79 | ||
| Substance use hospitalizations | |||
| Less than five (73%) | 73 | 0.06 | 0.09 |
| Five or more (27%) | 75 | ||
| 12-Step attendance (F1 – F2) | |||
| None (26%) | 64 | 6.19 | 7.39 |
| About once a month (5%) | 75 | ||
| Every other week (2%) | 100 | ||
| About once a week (18%) | 79 | ||
| More than once a week (49%) | 76 | ||
| Any inpatient treatment (F1 – F2) | |||
| Yes (19%) | 50 | 14.49** | 10.80** |
| No (81%) | 79 | ||
| MH symptoms (F1 – F2) | |||
| 0–3 (33%) | 78 | 1.36 | 0.66 |
| 4–7(35%) | 74 | ||
| 8–13(32%) | 69 | ||
| Concurrent DTR attendance (F1 – F2) | |||
| 0–5 months (33%) | 58 | 19.86** | 8.55** |
| 6–11 months (17%) | 68 | ||
| 12 months (50%) | 86 | ||
| Past DTR attendance (base – F1) | |||
| 0–5 months (15%) | 53 | 9.22** | 1.23 |
| 6–11 months (21%) | 72 | ||
| 12 months (64%) | 79 | ||
| Abstinence (base – F1) | |||
| Yes (72%) | 85 | 35.96** | 26.29** |
| No (28%) | 45 | ||
P<.05.
P<.01.
TABLE 3.
Longitudinal Relation of DTR, Traditional 12-Step, and Formal Treatment to Abstinence During Two Year Follow-Up: Estimated Regression Coefficients and z-Statistics
| Effect | df | χ2 | B | Robust SE | Robust z | Odds Ratio |
|---|---|---|---|---|---|---|
| DTR attendance | 1 | 11.44** | 1.1848 | .3158 | 3.75** | 3.27 |
| Traditional 12-Step attendance | 4 | 4.71 | — | — | — | — |
| About once a month versus none | 1 | — | 0.1389 | .5279 | 0.26 | 0.87 |
| Every other week versus none | 1 | — | 0.4422 | .5728 | 0.77 | 1.56 |
| About once a week versus none | 1 | — | 0.5704 | .3331 | 1.71 | 1.77 |
| More than once a week versus none | 1 | — | 0.6063 | .2951 | 2.05* | 1.83 |
| Abstinence before baseline | 1 | 30.47** | 1.4811 | .2573 | 5.76** | 4.40 |
| Age of onset of substance misuse | 1 | 1.26 | 0.0321 | .0295 | 1.09 | 1.03 |
| Primary substance of abuse | 4 | 7.48 | — | — | — | — |
| Cocaine/crack versus other | 1 | — | 0.0280 | .5834 | 0.05 | 0.97 |
| Alcohol versus other | 1 | — | 0.1580 | .5926 | 0.27 | 1.17 |
| Heroin versus other | 1 | — | 0.3982 | .6749 | 0.59 | 1.49 |
| Marijuana versus other | 1 | — | 1.1956 | .7204 | 1.66 | 3.31 |
| Inpatient treatment | 1 | 6.92** | 0.8505 | .3074 | 2.77** | 0.43 |
| Primary psychiatric diagnosis | 3 | 7.60 | — | — | — | — |
| Schizophrenia versus unipolar | 1 | — | 0.4677 | .3416 | 1.37 | 0.63 |
| Bipolar versus unipolar | 1 | — | 0.4480 | .4290 | 1.04 | 1.57 |
| Other versus unipolar | 1 | — | 0.5469 | .3906 | 1.40 | 0.58 |
| Mental health symptoms | 1 | 7.00** | 0.0936 | .0343 | 2.73** | 0.91 |
| Time period | 1 | 2.09 | 0.2872 | .1985 | 1.45 | 1.33 |
P<.05.
P<.01.
Table 1 presents the data for the one-year follow-up. Longer DTR attendance in the concurrent year (i.e., the year before the follow-up interview), fewer concurrent mental health symptoms, age of onset of substance misuse, primary psychiatric diagnosis, primary substance of abuse, and abstinence in the preceding year (i.e., the year before the baseline interview) had significant unique associations with greater likelihood of abstinence at the one year follow-up. Receiving inpatient treatment in the year before follow-up had a significant zero-order association indicating less abstinence at one-year, but did not have a significant unique effect.
Table 2 presents the data for the two-year follow-up. Similar to the one-year results, longer DTR attendance in the concurrent year and abstinence in the preceding year had significant unique associations with greater likelihood of abstinence at the two-year follow-up. Longer DTR attendance in the preceding year had a significant zero order association with abstinence at two years, but not a significant unique effect. Receiving inpatient treatment in the concurrent year had a significant unique effect indicating less abstinence at the two year follow-up. Finally, frequency of participation in traditional 12-Step fellowships was not uniquely related to abstinence at either follow-up.
Of the background variables, since only age of onset of substance misuse, primary psychiatric diagnosis, and primary substance of abuse were uniquely associated with abstinence in one of the time periods, only these variable were included in the longitudinal GEE analysis testing the study hypotheses. Abstinence in the preceding year also was included in the analyses since it was found to have a unique effect on current abstinence.
Repeated Measures Analysis of Abstinence with GEE
The estimated regression coefficients, associated robust standard errors and z-statistics for the GEE model are presented in Table 3. In this analysis, abstinence is treated as a repeated measures dependent variable. Other than “Time Period,” the effects represent the “averaged” effects on abstinence of each of these constructs over the two time periods. The “Time Period” effect represents possible differences in abstinence rates between the two follow-up periods. “Abstinence Before Baseline” is a control for substance use in the year prior to the baseline interview. Table 3 shows that after controlling for traditional 12-Step group attendance, formal (inpatient) treatment, age of onset of substance misuse, mental health symptoms, primary psychiatric diagnosis, primary substance of abuse, and abstinence before baseline, longer DTR attendance was significantly associated with a greater likelihood of abstinence during the two year follow-up period. Continuous variables are used in the analyses presented in Table 3, As in logistic regression (Hosmer & Lemeshow 2000), the regression coefficient for a main effect can be exponentiated to obtain an odds ratio associated with a unit increase in the predictor. A single month of DTR attendance was associated with a small increase in the odds of abstinence (B = 0.10, OR = 1.11). The effect of a full year of DTR attendance on abstinence can be estimated by receding attendance in terms of years instead of months. Doing so, a full year of DTR attendance was associated with a relatively large increase in the odds of abstinence relative to no DTR attendance (OR = 3.27).
In addition to the main effect of DTR attendance, there was a main effect of inpatient treatment after controlling for the other variables in the model whereby over time, receiving inpatient treatment was significantly associated with lower rates of abstinence: the likelihood of abstinence among participants who had received inpatient treatment was less than half that of participants who did not (OR = 0.43). There was also a main effect for mental health symptoms whereby, over time, those with more symptoms were less likely to be abstinent (OR = 0.91), Finally, prebaseline abstinence was significantly associated with abstinence during the subsequent two-year study period. Participants who were abstinent in the year before baseline were more than four times as likely to be abstinent during the two year study period (OR = 4.40).
The two-way interactions between time and the other main effects were also examined. None of these interactions was significant, suggesting the unique effects of variables other than time were similar in both periods.
Figure 1 summarizes the primary effect of interest— DTR attendance.2 The open circles in this figure represent the proportion of subjects reporting abstinence at each level of DTR attendance. The solid line within each panel represents the model predicted values of abstinence on the probability scale. As can be seen in this figure, in both follow-up periods, longer DTR attendance was associated with a greater likelihood of abstinence.
FIGURE 1.
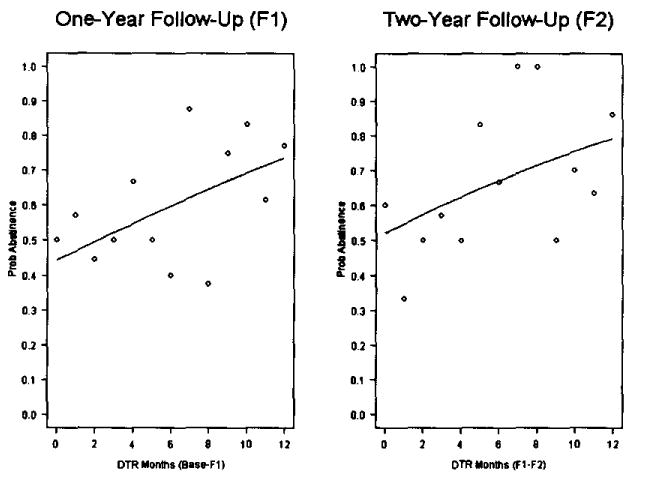
Predicted Probability of Abstinence as a Function of Time Period and DTR Attendance
DISCUSSION
The primary hypothesis that attendance at 12-Step based dual focus groups would be associated with a greater probability of abstinence independent of other factors that may be associated with abstinence was supported. As mentioned earlier, available evidence strongly supports 12-Step participation for dually-diagnosed clients (e.g. Ouimette, Finney & Moos 1997; Jerrell & Ridgely 1995). However, this appears to be the first report in the literature using a longitudinal study design to investigate the effectiveness of adapting the 12-Step model of recovery for dual diagnosis. Note that past DTR attendance without substantial concurrent attendance provided no unique contribution to abstinence. These findings suggest that DTR attendance is most beneficial when it is ongoing. Addiction is generally viewed as a chronic, relapse-prone disorder and ongoing support is believed to be crucial to promoting and sustaining recovery (e.g., McLellan et al. 2000). Substance use is an impulsive behavior that is likely to occur in close temporal proximity to triggering events, be they emotional (e.g., loneliness, anger) or environmental (e.g., being offered drugs). This is likely to be especially true among dually-diagnosed persons who may not have well-developed and practiced coping strategies that can provide an adaptive alternative to substance use to deal with stress and negative emotional states. The peer support and acceptance dual-focus groups provide may help overcome the loneliness and isolation that often trigger substance use in this population (Laudet et al. 2002). Further, exposure to other dually-diagnosed peers who have more time in recovery can provide role models for a drug-free life as well as adaptive strategies to cope with stress, another trigger to substance use. The finding that ongoing DTR attendance is associated with abstinence is consistent with 12-Step fellowship beliefs that addiction is a lifelong disorder and that recovery requires consistent 12-Step attendance over time—“one day at a time” and “keep coming back, it works if you work it” are popular 12-Step slogans. McKay and colleagues (2001) have reported that continued 12-Step participation was associated with positive outcome among cocaine users (also see Fiorentine 1999 ). We note that the majority of participants were enrolled in outpatient services at the time of the interviews. Because many of the DTR meetings are held in treatment programs, ongoing involvement with treatment is likely to have enhanced the likelihood of DTR participation. At the same time, participation in DTR, where members are exposed to recovering peers, may also reinforce and enhance the effectiveness of formal treatment.
With respect to the secondary hypotheses, attending traditional 12-Step groups was not significantly associated with abstinence in this dually-diagnosed sample. The findings were in the expected direction—abstinence was higher for those attending traditional 12-Step groups in addition to DTR—but did not reach statistical significance. We note, however, the significant contrast between no attendance and more than weekly attendance (Table 3), as well as the finding that attendance at traditional 12-Step groups was high, replicating prior reports (e.g., Bogenschutz & Akin 2000; Pristach & Smith 1999; Kurtz et al. 1995).
Findings did not support the hypothesized association between formal treatment and greater probability of abstinence. Instead, the association was significant in the opposite direction: the likelihood of abstinence was lower among persons who had received inpatient treatment during the study period. Although this dataset did not lend itself to an extensive investigation of this question, available data suggest that in about one-half of instances where participants reported substance use and inpatient treatment, and where chronology could be determined, substance use preceded hospitalization. The most plausible interpretation of the finding about the association between inpatient hospitalization and substance use appears to be one where greater psychiatric severity may have made inpatient hospitalization necessary during the course of the study and also explained greater rates of substance use (lower abstinence rates).
Based on current findings, we conclude that continued participation in dual-focus groups appears to be an important factor in the maintenance of good outcomes over extended periods among dually-diagnosed persons. This suggests that an important task for treatment providers is to facilitate clients’ engagement in recovery support groups, as previous noted by Mankowski and colleagues (2001). Where specialized dual focus groups are available, clinicians treating dually-diagnosed persons should emphasize the need for consistent participation over time; where such groups are not available, clinicians should educate clients about this resource, and support the initiation of such groups at their facilities (technical assistance for this is available from the DTR fellowship). Participation in traditional 12-Step groups should be encouraged as well.
This study has several limitations that must be considered in interpreting findings. First, the non-experimental design requires caution in making causal inferences; the authors are in the process of implementing a controlled longitudinal study to attempt to replicate and extend these promising results. Second, the sample was restricted to persons who had been attending DTR for a minimum of one month at recruitment and may differ in clinical or background characteristics from the general population of dually-diagnosed persons who have never attended DTR or who dropped out after attending one or two meetings (limiting the generalizability of findings). Finally, the use of self-report dictates caution in interpreting present results. With respect to self-reported substance use, the premium placed by 12-Step fellowships on honesty in recovery is presumed to have benefited the validity of the interview responses; further, most participants were enrolled in formal outpatient services and/or resided in supported living where substance use is monitored continuously. Self-reported psychiatric diagnoses were consistent with psychiatric medication regimens reported at the time of the interviews. However, the use of self-reported measures may have yielded an incomplete assessment of current severity (especially of psychiatric severity) that made the interpretation of some findings difficult—e.g., the association between inpatient hospitalization and substance use. The authors are currently conducting an effectiveness study of DTR where chart reviews will be used.
Footnotes
The authors gratefully acknowledge the cooperation of the DTR members whose experiences contributed to this article, as well as the help of the agencies where the study participants were recruited. The work reported here was supported by a grant from the Peter McManus Charitable Trust to A. Laudet and by NIDA Grant R01 DA11240 to S. Magura.
Information about final disposition of participants at two-year follow-up was lost in the authors’ World Trade Center offices. What information remains suggests that reasons for no follow-up at two years were similar to those at the one-year follow-up.
To simplify the presentation of predicted values, nonsignificant variables in the GEE model were trimmed, so the predictions in Figure 1 are based on a model with Time Period, Mental Health Symptoms, Inpatient Treatment, Abstinence Before Baseline, and DTR Attendance.
References
- American Psychiatric Association. Practice guidelines for the treatment of patients with substance abuse disorders: Alcohol, cocaine, opioids. American Journal of Psychiatry. 1995;152 (November supplement):1–59. doi: 10.1176/ajp.152.11.1. [DOI] [PubMed] [Google Scholar]
- Bartels SJ, Teague GB, Drake RE, Clark RE, Bush P, Noordsy DL. Substance abuse in schizophrenia: Service utilization and costs. Journal of Nervous and Mental Disorders. 1993;181:227–32. doi: 10.1097/00005053-199304000-00003. [DOI] [PubMed] [Google Scholar]
- Center for Mental Health Services. Making a Difference: Interim Status Report of the Mckinney Research Demonstration Program for Homeless Mentally Ill Adults. Rockville, Maryland: Substance Abuse; 1994. [Google Scholar]
- Clark R. Family costs associated with severe mental illness and substance use: A comparison of families with and without dual disorders. Hospital and Community Psychiatry. 1994;45:808–13. doi: 10.1176/ps.45.8.808. [DOI] [PubMed] [Google Scholar]
- Drake RE, Bartels SJ, Teague GB, Noordsy DL, Clark RE. Treatment of substance abuse in severely mentally ill patients. Journal of Nervous & Mental Disorders. 1993;181:606–11. doi: 10.1097/00005053-199310000-00006. [DOI] [PubMed] [Google Scholar]
- Florentine R, Hillhouse M. Drug treatment and 12-Step program participation: The additive effects of integrated recovery activities. Journal of Substance Abuse Treatment. 2000;18:65–74. doi: 10.1016/s0740-5472(99)00020-3. [DOI] [PubMed] [Google Scholar]
- Florentine R. After drug treatment: Are 12-Step programs effective in maintaining abstinence? American Journal of Drug and Alcohol Abuse. 1999;25:93–116. doi: 10.1081/ada-100101848. [DOI] [PubMed] [Google Scholar]
- Gonzalez G, Rosenheck R. Outcomes and service use among homeless persons with serious mental illness and substance abuse. Psychiatric Services. 2002;53:437–46. doi: 10.1176/appi.ps.53.4.437. [DOI] [PubMed] [Google Scholar]
- Hazelden Foundation. The Dual Diagnosis Recovery Book. Minneapolis, Minnesota: Hazelden; 1993. [Google Scholar]
- Hosmer DW, Lemeshow S. Applied Logistic Regression. Second Edition. New York: John Wiley & Sons; 2000. [Google Scholar]
- Humphreys K, Huebsch PD, Finney JW, Moos RH. A comparative evaluation of substance abuse treatment: V. Substance abuse treatment can enhance the effectiveness of self-help groups. Alcoholism, Clinical & Experimental Research. 1999;23:558–63. [PubMed] [Google Scholar]
- Jerrell JM, Ridgely MS. Comparative effectiveness of three approaches to serving people with severe mental illness and substance use disorders. Journal of Nervous and Mental Disorders. 1995;183:566–76. doi: 10.1097/00005053-199509000-00002. [DOI] [PubMed] [Google Scholar]
- Kessler RC. The national comorbidity survey: Preliminary results and future directions. International Journal of Methods in Psychiatric Research. 1995;5:139–51. [Google Scholar]
- Kingree JB. Understanding gender differences in psychosocial functioning and treatment retention. American Journal of Drug and Alcohol Abuse. 1995;11:77–92. doi: 10.3109/00952999509002694. [DOI] [PubMed] [Google Scholar]
- Kurtz LF, Garvin CD, Hill EM, Pollio D, McPherson S, Powell TJ. Involvement in Alcoholics Anonymous by persons with dual disorders. Alcoholism Treatment Quarterly. 1995;12:1–18. [Google Scholar]
- Laudet AB, Magura S, Vogel HS, Knight EL. Perceived reasons for substance abuse among dually-diagnosed persons. Paper presented at the 130th Annual Meeting of the American Public Health Association; Philadelphia. 2002. Nov, [Google Scholar]
- Laudet AB, Magura S, Vogel HS, Knight EL. Recovery challenges among dually diagnosed individuals. Journal of Substance Abuse Treatment. 2000a;18:321–29. doi: 10.1016/s0740-5472(99)00077-x. [DOI] [PubMed] [Google Scholar]
- Laudet AB, Magura S, Vogel HS, Knight EL. Support, mutual aid and recovery from dual diagnosis. Community Mental Health Journal. 2000b;36:457–76. doi: 10.1023/a:1001982829359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- Mankowski E, Humphreys K, Moos R. Individual and contextual predictors of involvement in 12-Step self-help groups after substance abuse treatment. American Journal of Community Psychology. 2001;29(4):537–63. doi: 10.1023/A:1010469900892. [DOI] [PubMed] [Google Scholar]
- McCrady BS, Miller WR. Research on Alcoholics Anonymous: Opportunities and Alternatives. New Brunswick, New Jersey: Alcohol Research Documentation, Rutgers—the State University of New Jersey; 1993. [Google Scholar]
- McKay J, Merikle E, Mulvaney F, Weiss R, Kopenhaver J. Factors accounting for cocaine use 2 years following initiation of continuing care. Addiction. 2001;96:213–25. doi: 10.1046/j.1360-0443.2001.9622134.x. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grisson G, Pettinati H, Angerion M. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Lewis D, O’Brien C, Kleber H. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. Journal of the American Medical Association. 2000;284:1689–95. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- Moos R, Schaefer J, Andrassy J, Moos B. Outpatient mental health care, self-help groups and patients’ 1-year treatment outcomes. Journal of Clinical Psychology. 2001;57:273–87. doi: 10.1002/jclp.1011. [DOI] [PubMed] [Google Scholar]
- Moos RH, Finney J, Ouimette PC, Suchinsky R. A comparative evaluation of substance abuse treatment: I. Treatment orientation, amount of care, and 1-year outcomes. Alcoholism Clinical and Experimental Research. 1999;23:529–36. [PubMed] [Google Scholar]
- Morgenstern J, McCrady BS. Cognitive processes and change in disease-model treatment. In: McCrady BS, Miller WR, editors. Research on Alcoholics Anonymous: Opportunities and Alternatives. New Brunswick, New Jersey: Alcohol Research Documentation, Rutgers—the State University of New Jersey; 1993. [Google Scholar]
- Ouimette P, Finney J, Moos RH. Twelve-step and cognitive behavioral treatment for substance abuse: A comparison of treatment effectiveness. Journal of Clinical and Consulting Psychology. 1997;65:230–40. doi: 10.1037//0022-006x.65.2.230. [DOI] [PubMed] [Google Scholar]
- Powell T, Kurtz L, Garvin C, Hill E. A model of A.A. utilization by persons with a dual diagnosis. Contemporary Drug Problems. 1996;23:139–57. [Google Scholar]
- Pristach C, Smith C. Attitudes towards Alcoholics Anonymous by dually-diagnosed patients. Journal of Addictive Diseases. 1999;18:69–76. doi: 10.1300/J069v18n03_07. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS/STAT User’s Guide, Version 8. Cary, North Carolina: SAS Institute, Inc.; 1999. [Google Scholar]
- Shern DL, Wilson NZ, Coen AS, Patrick DC, Foster MA, Bartsch DA, Demmler J. Client outcomes II: Longitudinal client data from the Colorado treatment outcome study. Milbank Quarterly. 1994;72:123–48. [PubMed] [Google Scholar]
- Timko C, Moos RH, Finney JW, Lesar MD. Long-term outcomes of alcohol use disorders: Comparing untreated individuals with those in Alcoholics Anonymous and formal treatment. Journal of Studies on Alcohol. 2000;61:529–40. doi: 10.15288/jsa.2000.61.529. [DOI] [PubMed] [Google Scholar]
- Vogel HS, Knight EL, Laudet AB, Magura S. Double trouble in recovery: Self-help for the dually-diagnosed. Psychiatric Rehabilitation Journal. 1998;21:356–64. doi: 10.1037/h0095288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–30. [PubMed] [Google Scholar]


