Abstract
Objective
To determine the rate of new onset of widespread pain after a traumatic event (motor vehicle crash).
Methods
A prospective cohort study of persons registered with an insurance company who had or had not experienced a motor vehicle crash. All participants were sent a questionnaire to assess pre‐crash (or for the non‐crash group, prior) psychosocial factors and widespread pain. Participants reporting pre‐crash (prior) widespread pain were excluded. At six months, participants were sent a follow up questionnaire to ascertain new prevalent widespread pain.
Results
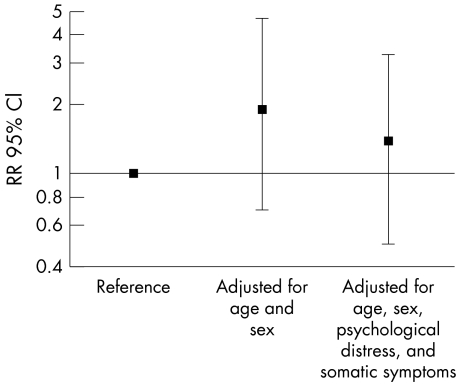
597 (51%) of participants returned a baseline questionnaire (465 crash and 132 non‐crash). Among the cohort who had experienced a crash, the new onset rate of widespread pain six months later was low (8%), though in comparison with the non‐crash group there was an increased risk (RR = 1.9 (95% CI, 0.8 to 4.8, adjusted for age and sex)); this was attenuated after adjustment for pre‐crash (prior) psychological distress and somatic symptoms (RR = 1.4 (95% CI, 0.5 to 3.2)).
Conclusions
The findings suggest that a motor vehicle crash (as an example of a physically traumatic event) is unlikely to have a major impact on the new onset of widespread pain. Any observed relation may, in part, be explained by psychological distress.
Keywords: fibromyalgia, pain, trauma
Widespread pain (WP) is a common condition affecting approximately 16% of the population.1 Almost 80% of those with WP experience chronic symptoms,2 representing a considerable burden to the individuals and their families, as well as to health care resources. Various adverse psychosocial factors may predict the onset of WP, in particular depression, somatic symptom reporting, and specific health behaviours.3,4,5 In addition, patients often attribute the onset of their symptoms to a precipitating physical trauma,6,7 although very few studies have been conducted to investigate this potential aetiological factor.
A few case–control and cross sectional studies have suggested there may be an association between trauma and WP.7,8 For example a case–control study comparing 136 hospital outpatients with fibromyalgia with 152 matched controls found that 39% of the fibromyalgia patients reported physical trauma in the previous six months, compared with 24% of controls.8 However, given that such studies measure exposure retrospectively and are potentially subject to recall bias, it is important to validate events wherever possible. One study involved a prospective assessment of the association between trauma and fibromyalgia syndrome,9 of which widespread pain is the primary symptom. The investigators concluded that fibromyalgia was 13 times more frequent following neck injury than following lower extremity injury. However, many of the tender point sites used to diagnose fibromyalgia are located in the neck area, so it may be expected that neck injured patients would report more pain and tenderness in these areas.
Our aim in the present study was to determine prospectively for the first time the rate of new onset widespread pain after a motor vehicle crash, and whether this is in excess of the new onset rate in the absence of such a physically traumatic event.
Methods
The design was a prospective cohort study. Subjects were recruited through a national UK motor insurance company. Individuals aged 17 to 70 years, who contacted the company to report a motor vehicle accident, were eligible for participation in the crash cohort. Those reporting other claims, for example theft or damage while the vehicle was unoccupied, were eligible for participation in the non‐crash cohort. Additionally all participants had to be making a claim less than seven days after their crash/non‐crash. The definition of crash was that provided by participants—that is, self report of a motor vehicle accident, with verification by the insurance company operative.
Subjects were asked to participate in the study at the time of telephoning the insurance company. Those who agreed to participate were then sent a questionnaire by post. General health and wellbeing in the month before the crash (or in the prior month for the non‐crash group) was assessed using the Health Status Short‐Form 8 (SF‐8)10 questionnaire. The Somatic Symptoms Checklist (SSC)11 measured the number of certain bodily symptoms experienced ever before the crash (or ever for the non‐crash group). General psychological distress was measured during the pre‐crash (or prior) month using the General Health Questionnaire (GHQ).12 Participants' pain status was determined using four full view body manikins on which they were asked to shade the location of any pain either in the past month (non‐crash group) or in the month before the crash (crash group). Individuals with widespread pain (using the American College of Rheumatology definition as part of the criteria for fibromyalgia13) were excluded.
Six months later, participants were re‐contacted by postal questionnaire and asked the same questions on pain. Subjects with widespread pain at follow up (using the body manikins) were labelled as “new prevalent widespread pain”.
Analysis
Poisson regression was employed to examine which factors measured at baseline predicted the presence of widespread pain at six months. Results are expressed as relative risks (RR) with 95% confidence intervals (CI).14
Results
We invited 1178 individuals to participate in the study, of whom 896 consented to receive a postal questionnaire. Questionnaires were returned by 597 (51%) of those invited to participate. They comprised 465 individuals in the crash cohort, mean age 42.0 years, 59% female; and 132 individuals in the non‐crash cohort, mean age 42.0 years, 60% female. The prevalence of WP in the month before the incident was 4% (n = 20) and 6% (n = 8) in the crash and non‐crash cohorts, respectively. These individuals were excluded from follow up, and thus 569 were eligible for follow up.
In all, 517 (87%) of these individuals completed the six month follow up questionnaire, of whom 490 provided complete pain data: 376 individuals in the crash cohort (81%) and 114 in the non‐crash cohort (86%). The prevalence of new WP was 8% (n = 31) in the crash cohort and 4% (n = 5) in the non‐crash cohort (RR = 1.9 (95% CI, 0.8 to 4.8, adjusted for age and sex)). Further adjustment for GHQ score (high v low distress) and somatic symptom reporting (0 v 1 or more symptoms) attenuated this risk (RR = 1.4 (95% CI, 0.5 to 3.2)) (fig 1). Adjustment for SF‐8 mental and physical scores did not further alter the risk of new WP.
Figure 1 Risk of new onset widespread pain at six months: accident v non‐accident cohort. CI, confidence interval; RR, relative risk.
Although this study was not designed to have sufficient power to examine risk separately in men and women, the data suggest that there may be differential effects by sex, with a slightly higher risk in women (RR = 1.5 (95% CI, 0.5 to 5.1)) compared with men (RR = 1.1 (95% CI, 0.3 to 4.3)) (table 1).
Table 1 Comparison of new onset WP between males and females.
| New onset widespread pain (n (%)) | Adjusted RR (95%CI)* | ||
|---|---|---|---|
| Crash group | Non‐crash group | ||
| All subjects | 31 (8.2) | 5 (4.4) | 1.4 (0.6 to 3.3) |
| Male | 12 (6.9) | 2 (4.7) | 1.1 (0.3 to 4.1) |
| Female | 19 (9.5) | 3 (4.2) | 1.5 (0.5 to 5.1) |
*Adjusted for age, psychological distress, and somatic symptom reporting.
CI, confidence interval; RR, relative risk.
Discussion
This is the first study to examine prospectively the rate of onset of widespread pain after physical trauma, namely a motor vehicle crash. It suggests that the rate of onset of WP after a motor vehicle crash is low and at most there is a modest increase in risk, particularly after adjusting for levels of psychological distress.
There are several caveats that need to be considered to put this study into context.
First, although the study was large, the number of new onset pain episodes was small. This is interesting as an observation in itself but does limit the power of the study.
Second, the initial response rate was low; of those invited to participate just over 50% returned a questionnaire, raising questions about the external validity of the study. The available data on those who did not return a questionnaire are limited; however, there were no significant differences in either age (Zm−w; p = 0.08) or sex (χ2; p = 0.08) between those who returned a completed questionnaire and those who were invited to participate but refused to or did not reply. It is also unlikely that those subjects who had experienced a crash but did not take part would be at a greater increased risk of developing WP, thus causing us to underestimate the risk.
Third, the precise role of psychological distress is difficult to determine in this study. It could be hypothesised that psychological distress is a pathway variable, that trauma leads to distress and then WP, and therefore should not be adjusted for. However, the measure of psychological distress used was before the trauma. Therefore psychological distress could lead to an increased likelihood of experiencing a motor vehicle crash, in addition to being associated with the onset of pain. In a recent study,15 Lagarde et al found that stressful life events were associated with a subsequent increase in serious motor vehicle accidents, lending support to this hypothesis. Adjusting for psychological distress does attenuate the relation between trauma and WP, but we do not know the extent to which the reporting of pre‐crash psychological distress was influenced by the post‐crash psychological distress experienced. Current work has suggested that prior distress, in particular depression, leads to a poor adjustment to stressful events16; additionally there are interactions between affective states, stressors, and pain.17 It will be important for future studies to explore not only the effect of trauma but modifiers of its effect.
This study does have several strengths. The design is prospective and therefore we have been able to determine the new onset of WP in persons who were initially WP‐free. An inherent problem of prospective studies is loss to follow up; however, loss in this study is minimal. Further, it may be expected that any such loss to follow up may result in an overestimation of the new onset of widespread pain. The setting was population based, thus overcoming the potential issue of selection bias associated with samples selected from clinic populations.
Our study suggests that the new onset of widespread pain after a motor vehicle crash is uncommon and only marginally above that experienced by a non‐crash group. The rate of new onset over a six month period in the non‐crash group (4%) was very similar to the rate reported (6%) over a 12 month period in a study of 1658 adults in the general population of one area of north west England.18 This provides additional support for the study's external validity.
Previous studies have reported that trauma is associated with WP7,8,9; however, methodological limitations, such as recall bias and the inability to measure the onset of pain, have restricted the interpretation of these findings. We have added to the literature by demonstrating a weak relation between trauma and the onset of WP. Studies have suggested that prior trauma is reported by 23%7 and 39%8 of fibromyalgia patients. These studies, however, have been conducted in specialist clinics among a selected population of fibromyalgia patients. Nevertheless the latter study,8 although showing an association between fibromyalgia and trauma, found that in both case and control subjects the report of a motor vehicle crash was uncommon. It is possible that an association does exist but with other and more severe forms of trauma.
In summary, the results of this preliminary study do not provide strong support for physical trauma (at least as exemplified by a motor vehicle crash) having a large impact on the new onset of widespread pain. It suggests a more modest estimate of the effect of trauma than those previously reported.
Acknowledgements
The study received ethical approval from the University of Manchester committee for the ethics of research on human beings.
GW‐J was funded by an MRC PhD studentship. The study was funded by the Arthritis Research Campaign, Chesterfield. The authors would like to thank the staff at Direct Line Insurers, Manchester, for their help in recruiting subjects.
Abbreviations
GHQ - General Health Questionnaire
SF‐8 - Health Status Short‐Form 8
SSC - Somatic Symptoms Checklist
WP - widespread pain
References
- 1.Croft P R, Rigby A S, Boswell R, Schollum J, Silman A J. The prevalence of chronic widespread pain in the general population. J Rheumatol 199320710–713. [PubMed] [Google Scholar]
- 2.Macfarlane G J, McBeth J, Silman A J. Widespread body pain and mortality: prospective population based study. BMJ 2001323662–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hunt I M, Silman A J, Benjamin S, McBeth J, Macfarlane G J. The prevalence and associated features of chronic widespread pain in the community using the “Manchester” definition of chronic widespread pain. Rheumatology (Oxford) 199938275–279. [DOI] [PubMed] [Google Scholar]
- 4.McBeth J, Macfarlane G J, Hunt I M, Silman A J. Risk factors for persistent chronic widespread pain: a community‐based study. Rheumatology (Oxford) 20014095–101. [DOI] [PubMed] [Google Scholar]
- 5.Benjamin S, Morris S, McBeth J, Macfarlane G J, Silman A J. The association between chronic widespread pain and mental disorder: a population‐based study. Arthritis Rheum 200043561–567. [DOI] [PubMed] [Google Scholar]
- 6.Wolfe F. Post‐traumatic fibromyalgia: a case report narrated by the patient. Arthritis Care Res 19947161–165. [DOI] [PubMed] [Google Scholar]
- 7.Greenfield S, Fitzcharles M A, Esdaile J M. Reactive fibromyalgia syndrome. Arthritis Rheum 199235678–681. [DOI] [PubMed] [Google Scholar]
- 8.Al‐Allaf A W, Dunbar K L, Hallum N S, Nosratzadeh B, Templeton K D, Pullar T. A case‐control study examining the role of physical trauma in the onset of fibromyalgia syndrome. Rheumatology (Oxford) 200241450–453. [DOI] [PubMed] [Google Scholar]
- 9.Buskila D, Neumann L, Vaisberg G, Alkalay D, Wolfe F. Increased rates of fibromyalgia following cervical spine injury. A controlled study of 161 cases of traumatic injury. Arthritis Rheum 199740446–452. [DOI] [PubMed] [Google Scholar]
- 10.Ware J E, Kosinski M A, Dewey J E, Gandeck B.How to score and interpret single‐item health status measures: a manual for users of the SF8 Health Survey. Boston: Quality Metric Inc and Health Assessment Lab, 2001
- 11.Othmer E, DeSouza C. A screening test for somatization disorder (hysteria). Am J Psychiatry 19851421146–1149. [DOI] [PubMed] [Google Scholar]
- 12.Goldberg D P, Williams P.A user's guide to the General Health Questionnaire. Windsor: Nfer‐Nelson, 1988
- 13.Wolfe F, Smythe H A, Yunus M B, Bennett R, Bombardier C, Goldenberg D L.et al The American College of Rheumatology 1990 Criteria for the Classification of fibromyalgia. Arthritis Rheum 199033160–172. [DOI] [PubMed] [Google Scholar]
- 14.Greenland S. Model‐based estimation of relative risks and other epidemiologic measures in studies of common outcomes and in case‐control studies. Am J Epidemiol 2004160301–305. [DOI] [PubMed] [Google Scholar]
- 15.Lagarde E, Chastang J F, Gueguen A, Coeuret‐Pellicer M, Chiron M, Lafont S. Emotional stress and traffic accidents: the impact of separation and divorce. Epidemiology 200415762–766. [DOI] [PubMed] [Google Scholar]
- 16.Southwick S M, Vythilingam M, Charney D S. The psychobiology of depression. Annu Rev Clin Psychol 20051255–291. [DOI] [PubMed] [Google Scholar]
- 17.Zautra A J, Johnson L M, Davis M C. Positive affect as a source of resilience for women in chronic pain. J Consult Clin Psychol 200573212–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McBeth J, Macfarlane G J, Benjamin S, Silman A J. Features of somatization predict the onset of chronic widespread pain: results of a large population‐based study. Arthritis Rheum 200144940–946. [DOI] [PubMed] [Google Scholar]