We report the case of a 47 year old woman with a 19 year history of mixed connective tissue disease (MCTD) diagnosed according to Alarcón‐Segovia classification criteria.1 She had Raynaud's phenomenon, arthritis, swollen hands, and anti‐ribonucleoprotein antibodies (anti‐RNP 1/1280). She received low doses of prednisone and her clinical course was uneventful, except for sporadic Raynaud's phenomenon. Her drug treatment was stopped 10 years ago, but medical supervision continued without evidence of pulmonary, gastrointestinal or renal disease during her follow up.
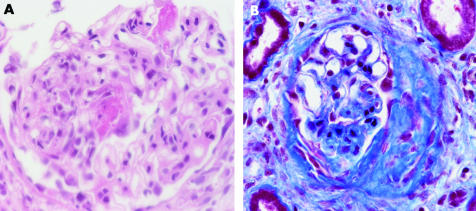
In 2003, she sought medical attention complaining of malaise during the past 3 months. Physical examination disclosed paleness, facial telangiectases, and hypertension (160/100). Laboratory findings were high—erythrocyte sedimentation rate (102 mm/1st h), normocytic/normochromic anaemia (haemoglobin 90 g/l), severely decreased renal function (creatinine had tripled to 250 μmol/l), and heavy proteinuria (6.5 g/day). Creatinine clearance was 20 ml/min. Urinary sediment exhibited dysmorphic red blood cells. Complement was normal and ANCA were positive with a perinuclear staining pattern (1/320). Previously, ANCA had not been determined. Anti‐myeloperoxidase (MPO) specificity was detected (9.3 U; normal <9.0). Two days later her serum creatinine increased to 360 μmol/l. A renal biopsy was performed, yielding a necrotising glomerulonephritis with fibrocellular crescents (fig 1). Immunofluorescence was negative for immunoglobulins and complement. No other clinical or laboratory feature reminiscent of microscopic polyangiitis was found.
Figure 1 (A) Necrotising glomerulonephritis in a patient with MCTD and (B) extracapillary proliferation and crescent formation.
Methylprednisolone pulse therapy was started, followed by intravenous cyclophosphamide. The patient continued with prednisone and monthly cyclophosphamide (nine doses) and achieved complete remission after 6 months. Serum creatinine decreased to 100 μmol/l, proteinuria to 255 mg/day, creatinine clearance reached 55 ml/min, and the microhaematuria disappeared. Azathioprine was started as maintenance treatment. She has remained in complete clinical remission during the past 14 months.
This is an unusual clinical association, reported only once.2 In both cases, patients with a clinically benign, longlasting MCTD developed a rapidly progressive glomerulonephritis with anti‐MPO antibodies, and responded favourably to treatment.
Clustering of systemic and organ‐specific autoimmune disease can occur in the same person or among several family members.3 This finding led to the proposal of the concept named shared autoimmunity.4 Accordingly, McDonagh and Isenberg reported at least one additional autoimmune disease in nearly 30% of a retrospective cohort of patients with systemic lupus erythematosus.5 Thus, a person who has an autoimmune disease may be more susceptible to developing a second one. These associations are likely to be triggered by unknown factors in genetically predisposed subjects.
The coexistence of necrotising glomerulonephritis (NGN) with organ‐specific or systemic autoimmune diseases has been reported.6 Endo et al found anti‐MPO antibodies in 6% of patients with systemic sclerosis (SSc) during the development of rapidly progressive renal failure.7 Further, this entity has also been reported in about 10% of 112 renal biopsies from patients with rheumatoid arthritis (RA) and renal disease.8 In this setting, is noteworthy the relationship between SSc and RA with NGN because findings similar to both conditions (SSc and RA) form part of the clinical manifestations grouped under the term MCTD.
The diagnostic and therapeutic procedure in a patient with MCTD who presents with rapidly progressive renal failure deserves some comments. Glomerulonephritis can be present in up to 20% of patients with MCTD. These glomerular diseases occasionally produce a rapid progressive renal failure.9 In such a case, the presence of a scleroderma‐like renal crisis must be strongly considered.10 Finally, when rapidly progressive renal dysfunction develops in a patient with a collagen disease, ANCA associated NGN is another diagnostic consideration. A renal biopsy must be performed to rule out vasculitis because the treatment depends highly on the histological findings.
Footnotes
Acting editor A D Woolf.
References
- 1.Alarcón‐Segovia D. Classification and diagnostic criteria for mixed connective tissue disease. J Rheumatol 19763191. [PubMed] [Google Scholar]
- 2.Makita N, Katori H, Takemoto F, Yokota M, Kitamura Y, Ubara Y.et al A case of mixed connective tissue disease complicated with MPO‐ANCA‐related necrotizing glomerulonephritis. Clin Nephrol 200054164–168. [PubMed] [Google Scholar]
- 3.Alarcón‐Segovia D, Alarcón‐Riquelme M E, Cardiel M H, Caeiro F, Massardo L, Villa A R.et al Familial aggregation of systemic lupus erythematosus, rheumatoid arthritis, and other autoimmune diseases in 1,177 lupus patients from the GLADEL cohort. Arthritis Rheum 2005521138–1147. [DOI] [PubMed] [Google Scholar]
- 4.Alarcón‐Segovia D. Shared autoimmunity: the time has come. Curr Rheumatol Rep 200461771–1774. [DOI] [PubMed] [Google Scholar]
- 5.McDonagh J E, Isenberg D A. Development of additional autoimmune disease in a population of patients with systemic lupus erythematosus. Ann Rheum Dis 200059230–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tanemoto M, Miyakawa H, Hanai J, Yago M, Kitaoka M, Uchida S. Myeloperoxidase‐antineutrophil cytoplasmic antibody positive crescentic glomerulonephritis complicating the course of Graves' disease: report of three adult cases. Am J Kid Dis 199526774–780. [DOI] [PubMed] [Google Scholar]
- 7.Endo H, Hosono T, Kondo H. Antineutrophil cytoplasmic autoantibodies in 6 patients with renal failure and systemic sclerosis. J Rheumatol 199421864–870. [PubMed] [Google Scholar]
- 8.Harper I, Cockwell P, Howie A, Richards M, Savage C, Wheeler D.et al Focal segmental necrotizing glomerulonephritis in rheumatoid arthritis. Q J Med 199090125–132. [DOI] [PubMed] [Google Scholar]
- 9.Bennet R, Spargo B. Immune complex nephropathy in mixed connective tissue disease. Am J Med 197763534–541. [DOI] [PubMed] [Google Scholar]
- 10.Satoh K, Imai H, Yasuda T, Wakui H, Mirua A, Nakamoto Y. Sclerodermatous renal crisis in a patient with mixed connective tissue disease. Am J Kidney Dis 199424215–218. [DOI] [PubMed] [Google Scholar]