Osteonecrosis of the femoral head (ON) has been recognised as a relatively common complication in patients with systemic lupus erythematosus (SLE) who have received corticosteroids, with a reported prevalence of around 30%.1 Recently, subchondral insufficiency fracture of the femoral head (SIF) has been reported as a differential diagnosis in patients suspected of having osteonecrosis.2,3,4 We describe the clinicopathological features of a patient with SLE with a history of corticosteroid treatment, who developed SIF.
A 55 year old woman had a 32 year history of SLE, which had been treated with corticosteroids (8 mg/day). She had a history of hypothyroidism, arthritis in both shoulders, skin rash, pericarditis, and pleuritis, but had no history of smoking or drinking. The body mass index indicated she was overweight (27.4 kg/m2).
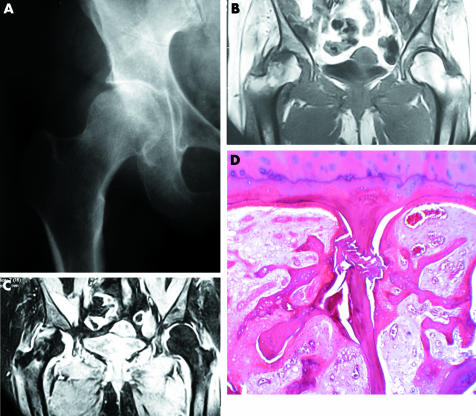
Over the past 5 years she had developed stiffness and discomfort in the right hip, and over the past 2 months the hip pain had got worse. Radiographs obtained at the first visit demonstrated slight joint space narrowing with a sclerotic change in the superolateral portion of the acetabulum. A sclerotic rim formation was not seen. The patient was treated with anti‐inflammatory drugs and use of a cane. However, the hip pain got worse. Radiographs obtained 1 month after the first visit showed progressive joint space narrowing with associated flattening of the lateral portion of the femoral head (fig 1A). Magnetic resonance imaging (MRI) obtained at the same time disclosed bone marrow oedema, mainly at the lateral part of the femoral head (figs 1B, C). An irregular serpiginous low intensity band was present at the superolateral margin of the femoral head on T1 weighted image. On T2 weighted image, both the band and area between the band and the articular surface showed high signal intensity. Owing to progressive severe hip pain, the patient underwent total hip arthroplasty.
Figure 1 (A) Radiograph obtained 1 month after the first visit shows progressive joint space narrowing with associated flattening of the lateral portion of the femoral head. (B, C) MRI shows a bone marrow oedema pattern, mainly at the lateral part of the femoral head extending to the intertrochanteric area. On T1 weighted image (repetition time (TR)/echo time (TE) = 380/20 ms), in addition to the diffuse low intensity, an irregular serpiginous low intensity band is present at the superolateral margin of the femoral head (B). On T2 weighted image (TR/TE = 1246/16 ms), both the band and the area between the band and the articular surface show high signal intensity. (D) Microscopically the whitish regions consist of fractured original lamellar bone with associated fracture callus, reactive cartilage, and granulation tissue. There is no evidence of antecedent osteonecrosis. (Haematoxylin and eosin; original magnification ×40.)
On a mid‐coronal cut section of the resected femoral head, a notched linear shaped whitish tissue was seen under the cartilage flap. Microscopically the whitish regions consisted of fracture callus, reactive cartilage, and granulation tissue (fig 1D).5 There was no evidence of antecedent osteonecrosis. In addition, there were several round to oval shaped granulomatous lesions in the marrow space. Thin disconnected bone trabeculae indicative of osteopenia were seen.
One of the important complications of patients with systemic lupus erythematosus treated with corticosteroids is ON. Before the development of MRI and the concept of SIF were introduced, this case most likely would have been interpreted as ON.
One of the characteristic findings on MRI in SIF has been reported as the shape of the low intensity band on T1 weighted images, which is generally irregular, serpiginous, paralleling the articular surface, and often discontinuous.2,3,4,5,6 On the other hand, in osteonecrosis, the low intensity band represents the repair tissue in response to osteonecrosis.7,8 As a consequence, the band is generally smooth and is seen in a different location circumscribing the necrotic segment.7,8,9 On T2 weighted images, in SIF, both the low intensity band and the proximal portion tend to show a high intensity, especially in the early phase of the fracture. In osteonecrosis, because the tissue between the band and the articular surface is an osteonecrotic area, T2 weighted images will not show high signal intensity.6,9 In addition, the location of the bone marrow oedema is useful for the differentiation. The oedema in ON is known to be found in living bone outside the low intensity band.10 In this case with SIF, the oedema pattern was seen both outside and within the low intensity band.
Acknowledgments
This work was supported in part by a grant from Japan Orthopaedics and Traumatology Foundation Inc, and a grant from the Clinical Research Foundation (2004).
Footnotes
Investigation performed at Departments of Orthopaedic Pathology and Radiology, Hospital for Special Surgery, 535 East 70th Street, New York, NY 10021, USA
References
- 1.Nagasawa K, Ishii Y, Mayumi T, Tada Y, Ueda A, Yamauchi Y.et al Avascular necrosis of bone in systemic lupus erythematosus: possible role of haemostatic abnormalities. Ann Rheum Dis 198948672–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yamamoto T, Bullough P G. Subchondral insufficiency fracture of the femoral head: a differential diagnosis in acute onset of coxarthrosis in the elderly. Arthritis Rheum 1999422719–2723. [DOI] [PubMed] [Google Scholar]
- 3.Vande Berg B C, Malghem J, Goffin E J, Duprez T P, Maldague B E. Transient epiphyseal lesions in renal transplant recipients: presumed insufficiency stress fractures. Radiology 1994191403–407. [DOI] [PubMed] [Google Scholar]
- 4.Rafii M, Mitnick H, Klug J, Firooznia H. Insufficiency fracture of the femoral head: MR imaging in three patients. AJR Am J Roentgenol 1997168159–163. [DOI] [PubMed] [Google Scholar]
- 5.Yamamoto T, Schneider R, Bullough P G. Insufficiency subchondral fracture of the femoral head. Am J Surg Pathol 200024464–468. [DOI] [PubMed] [Google Scholar]
- 6.Yamamoto T, Schneider R, Bullough P G. Subchondral insufficiency fracture of the femoral head: histopathologic correlation with MRI. Skeletal Radiol 200130247–254. [DOI] [PubMed] [Google Scholar]
- 7.Bullough P G, DiCarlo E F. Subchondral avascular necrosis: a common cause of arthritis. Ann Rheum Dis 199049412–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yamamoto T, DiCarlo E F, Bullough P G. The prevalence and clinicopathological appearance of extension of osteonecrosis in the femoral head. J Bone Joint Surg Br 199981328–332. [PubMed] [Google Scholar]
- 9.Kubo T, Yamazoe S, Sugano N, Fujioka M, Naruse S, Yoshimura N.et al Initial MRI findings of non‐traumatic osteonecrosis of the femoral head in renal allograft recipients. Magn Reson Imaging 1997151017–1023. [DOI] [PubMed] [Google Scholar]
- 10.Iida S, Harada Y, Shimizu K, Sakamoto M, Ikenoue S, Akita T.et al Correlation between bone marrow edema and collapse of the femoral head in steroid‐induced osteonecrosis. AJR Am J Roentgenol 2000174735–743. [DOI] [PubMed] [Google Scholar]