Abstract
Objective
To investigate the facioskeletal morphology in patients with juvenile idiopathic arthritis (JIA) with and without temporomandibular joint (TMJ) involvement.
Methods
Eighty five patients were included. TMJ involvement was defined by orthopantomogram alterations. Lateral cephalograms were used to determine linear and angular measurements and occlusion.
Results
Patients regardless of their TMJ status had a 67% chance for retrognathia and a 52% chance for posterior rotation of the mandible and, respectively, 82% and 58% if TMJ involvement were present. Changes were not uniformly distributed among the different subtypes.
Conclusion
Patients with JIA have an altered facial morphology, especially in the presence of TMJ involvement.
Keywords: juvenile idiopathic arthritis, temporomandibular joints
Juvenile idiopathic arthritis (JIA) is characterised by arthritis persisting for at least 6 weeks and onset before the 16th birthday and may affect several joints, including the temporomandibular joint (TMJ).1
The TMJ can be affected both unilaterally and bilaterally, early or late in the course of the disease, and it can even be the first joint affected. The reported prevalence of TMJ involvement varies from 17% to 87% depending on the population investigated, the subtypes of JIA represented and the radiological method by which involvement is diagnosed.2,3,4,5,6 In a survey representing all subtypes of JIA, the prevalence of TMJ involvement diagnosed with an orthopantomogram (OPT) was 45%.7 Arthritis of the TMJ results in reduced mandibular growth and subsequent alteration in dental occlusion and may even affect the total craniofacial growth.2,3,4,5
Alterations in the craniofacial structure of patients with JIA have been described in several studies.5,8,9,10,11,12 Patients with JIA demonstrated retrognathia and increased mandibular posterior rotation. Usually the characteristic facial morphology has been associated with condylar destruction.5,8,9,10,11,12
Most studies were performed in the oligo‐ and polyarticular subtype with more rethrognathia and posterior rotated mandibles in the polyarticular subtype.5,8,9 Only one study reported a mild downward and backward rotation of the mandible in the systemic subtype.11
The purpose of this study was to determine the influence of arthritis of the TMJ on facioskeletal morphology in a cohort representing all subtypes of JIA.
Patients and methods
Patients
In a 6 month period all children with JIA, according to the Durban criteria, who visited the paediatric rheumatology clinic of the Erasmus MC Sophia Children's Hospital, were routinely referred for orthodontic evaluation, even in the absence of complaints. The initial 97 consecutive children were reviewed to evaluate the prevalence of TMJ involvement. Patients with both OPT and lateral cephalogram available were included.
Methods
Radiographic examination
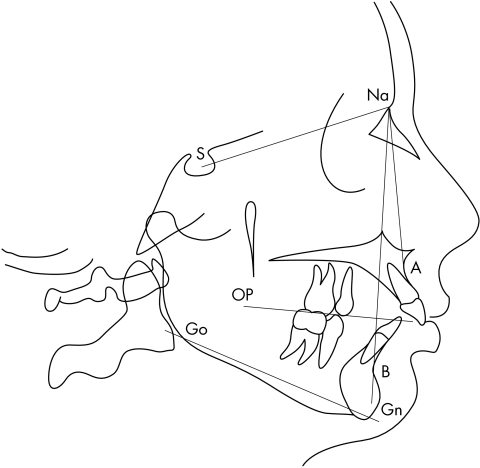
A standardised radiographic examination was carried out by means of lateral cephalograms and OPTs. All lateral cephalograms were digitised with an Epson 1680 Pro scanner (Epson, Long Beach, USA) and traced with QuickCeph 2000 software (QuickCeph, San Diego, USA). The following values were measured using the lateral cephalograms (see fig 1): ANB, indicating the discrepancy between maxilla and mandible, and Go‐Gn to S‐Na and OP to S‐Na, both evaluating the divergency of the maxilla and mandible.13
Figure 1 Tracing of a lateral cephalogram. Retrognathia is determined by the ANB angle (S‐Na‐A minus S‐Na‐B), and posterior rotation of the mandible is determined by the mandibular plane to cranial base angle (Go‐Gn to S‐Na) and the occlusal plane to cranial base angle (OP to S‐Na).
The OPTs were used to determine TMJ involvement and to measure mandibular ramus lengths.
TMJ involvement was diagnosed using the six categories of Rohlin: grade 0, normal conditions; grade 1, slight abnormality; grade 2, definite early abnormality; grade 3, moderate destructive abnormality; grade 4, severe destructive abnormality; and grade 5, mutilating abnormality.14
Some films showed magnification owing to incorrect placement of patients during the x ray examination, therefore left/right ratios were used instead. Differences between left and right mandibular length were calculated using the formula: ((R‐L)/(R‐L)) × 100%. Differences >3% are due to asymmetries of the mandibular condyle or ramus height, while differences <3% are caused by technical failures.15 Therefore asymmetry of the mandible was defined as a ramus length difference of >3%.
Cephalometric standards
Control data for the cephalometric measurements of patients aged 6–16 years were obtained according to sex and age, based on Riolo et al.16 Normal values for patients older than 16 years were based on Steiner.17 Posterior rotation of the mandible was defined as the mean + 2 SD of Go‐Gn to S‐Na and OP to S‐Na. Retrognathia was defined as a mean ANB value of >4 degrees.
Statistical analysis
SPSS version 12.0 for Windows (SPSS‐PC, Chicago, USA) was used for data analysis. To compare differences in means between the group with and without TMJ involvement Student's t test was used for continuous variables and a χ2 test for ordinal values.
Results
Of the initial cohort, 12 patients were excluded owing to technical failures of the cephalogram (n = 10) and OPT (n = 2). All necessary information was available for 85 patients.
Table 1 summarises information on TMJ involvement, unilaterally or bilaterally, divided according to subtype. According to the grading system of Rohlin 38 of the 85 patients (45%) had TMJ involvement; 18 patients had unilateral involvement and 20 bilateral involvement.
Table 1 JIA subtype distribution and TMJ involvement.
| JIA subtype | No (%) | TMJ involvement (%) | ||
|---|---|---|---|---|
| Total | Unilateral | Bilateral | ||
| Systemic | 14 (16) | 10 (71) | 3 (30) | 7 (70) |
| Oligoarticular* | 38 (45) | 15 (39) | 8 (53) | 7 (47) |
| Polyarticular RF positive | 6 (7) | 3 (50) | 3 (100) | 0 (0) |
| Polyarticular RF negative | 14 (16) | 7 (50) | 2 (29) | 5 (71) |
| ERA | 8 (9) | 1 (13) | 1 (100) | 0 (0) |
| Psoriatic arthritis | 2 (2) | 1 (50) | 0 (0) | 1 (100) |
| Other | 3 (4) | 1 (33) | 1 (100) | 0 (0) |
| Total | 85 (100) | 38 (45) | 18 (47) | 20 (53) |
*Thirty four oligoarticular persistent and four oligoarticular extended.
The only difference found between the different subtypes was age at onset (mean 6.0 years); patients with the polyarticular subtype were 2.7 and 3.5 years older than the oligoarticular and systemic subtypes. The mean duration of the disease was 4.9 years, with minimal differences among the different subtypes. The subtype distribution found in this study is in agreement with the distribution found in a regular paediatric rheumatology department.
As in previous reports, more girls than boys were represented (respectively, 50 and 35). TMJ involvement was almost equally distributed between girls and boys (respectively, 48% and 40%).
Cephalometric analysis
Retrognathia was present in 57/85 (67%) patients with JIA. This percentage was higher in patients with TMJ involvement (31/38 (82%)) than in those without TMJ involvement (26/47 (55%)). On average, ANB was 1.8 (p = 0.001) degrees greater in patients with TMJ involvement than in patients without TMJ involvement.
Posterior rotation was present in 44/85 (52%) patients with JIA according to Go‐Gn to S‐Na and in 60/85 (71%) according to OP to S‐Na. Posterior rotation measured by OP to S‐Na was equal in patients with and without TMJ involvement (71% and 70%). Go‐Gn to S‐Na showed that the mandibles were more posteriorly rotated in patients with TMJ involvement than in those without (58% v 47%).
The three large subgroups—namely, systemic onset arthritis, oligoarticular arthritis, and polyarticular arthritis (including rheumatoid factor (RF) positive and negative), were used to study the influence of subtype. Comparison between patients within these subtypes showed that retrognathia was most often found in patients with polyarticular JIA (75%), followed by the patients with oligoarticular (68%) and systemic disease (64%).
Posteriorly rotated mandibles were more common in the systemic subtype (93%) than in the polyarticular and oligoarticular subtypes (65% and 63%) when measured by OP to S‐Na.
Measured by Go‐Gn to S‐Na, posterior rotation was also most common in the systemic type (79%), followed by the oligoarticular type and polyarticular types (45% and 45%) of JIA.
The intraobserver agreement measured by κ statistics was 0.79 for ANB, 0.55 for Go‐Gn to S‐Na, and 0.53 for OP to S‐Na. The interobserver agreement was 0.85 for ANB, 0.59 for Go‐Gn to S‐Na, and 0.44 for OP to S‐Na.
Analysis of orthopantomograms
Mandibular asymmetry was seen in 23/85 (27%) patients. Asymmetry was more common in patients with TMJ involvement than in those without TMJ involvement (37% v 19%, p = 0.07). No difference in asymmetry was found between patients with unilateral and bilateral involvement (39% v 37%). Of the 20 patients with bilateral condylar involvement, seven had disproportionate TMJ involvement—that is, one condyle was more severe affected than the condyle on the other side. Of these seven patients with disproportionate involvement, five also showed asymmetry. In patients with proportional bilateral involvement two patients also showed asymmetry.
Discussion
In our survey, patients with JIA, regardless of their TMJ status, had retrognathia and more posteriorly rotated mandibles than age matched healthy subjects previously reported.16,17 In agreement with the published reports, we also found that retrognathia and posterior rotation is more common in patients with TMJ involvement.8,10,11,12 However, in these studies no patients with JIA without TMJ involvement were compared with age matched healthy subjects. Our study also found retrognathia and posterior rotation of the mandible in patients without TMJ involvement, which might be explained by TMJ alterations that were not yet detectable at OPT at the time of evaluation. On the other hand, these patients might have had TMJ alterations earlier, which were no longer detectable on radiographs.
Our study provides a unique possibility to compare the three major subtypes of JIA. Among these subtypes, retrognathia and posterior rotation of the mandible were not uniformly distributed. Retrognathia is most common in the polyarticular subtypes, closely followed by the oligoarticular and systemic subtype. Posterior rotation of the mandible is more common in the systemic subtype. The only study performed with patients with systemic JIA also describes more downwards and backwards rotated mandibles.11 No study has compared patients with systemic JIA with patients with oligo‐ and polyarticular disease. We found no difference in the prevalence of posteriorly rotated mandibles between the patients with oligo‐ and polyarticular JIA.
In agreement with published reports, we found more retrognathia in the polyarticular subtype than the oligoarticular subtype (75% v 68%).6,8,10 However, as no actual percentages of retrognathia were defined in the other studies, no comparison with our study was possible.
In our survey, posterior rotation is measured in two different ways, giving different results. This discrepancy might be explained because the angle OP to S‐Na takes the occlusion into account. Variation of the occlusal plane was believed to be too great because most of our patients had mixed dentitions, resulting in a temporarily altered occlusal plane owing to shedding of primary teeth.
Patients with TMJ involvement have more mandibular asymmetry than patients without TMJ involvement. Although this finding was not significant, this trend might help as a diagnostic tool for TMJ involvement. As the κ statistic for intra‐ and interobserver agreement is high for ANB, tracing is a useful tool for rethrognathia.
In contrast with our expectations, we found no difference in asymmetry between unilaterally and bilaterally affected patients. This is because the bilaterally disproportionate group (that is, one condyle was more severely affected than the condyle on the other side) also showed mandibular asymmetry.
Beside facioskeletal changes, arthritis of the TMJ also leads to difficulty with chewing, oral health problems (for example, caries), problems with intubations, and aesthetic problems.
In conclusion, patients with JIA are more likely to exhibit retrognathia and posterior rotation of the mandible in the presence of TMJ involvement. Hence retrognathia and posterior rotation might serve as a predictor for TMJ involvement in patients with JIA.
Abbreviations
JIA - juvenile idiopathic arthritis
OPT - orthopantomogram
RF - rheumatoid factor
TMJ - temporomandibular joint
Footnotes
Competing interest: None.
References
- 1.Petty R E, Southwood T R, Manners P, Baum J, Glass D N, Goldenberg J.et al International League of Associations for Rheumatology Classification of Juvenile Idiopathic Arthritis: second revision, Edmonton, 2001. J Rheumatol 200431390–392. [PubMed] [Google Scholar]
- 2.Kjellberg H. Craniofacial growth in juvenile chronic arthritis. Acta Odontol Scand 199856360–365. [DOI] [PubMed] [Google Scholar]
- 3.Küseler A, Pederson T K, Herlin T, Gelineck J. Contrast enhanced magnetic resonance imaging as a method to diagnose early inflammatory changes in the temporomandibular joint in children with juvenile chronic arthritis. J Rheumatol 1998251406–1412. [PubMed] [Google Scholar]
- 4.Mayne J G, Hatch G S. Arthritis of the temporomandibular joint. J Am Dent Assoc 196979125–130. [DOI] [PubMed] [Google Scholar]
- 5.Mericle P M, Wilson V K, Moore T L, Hanna V E, Osborn T G, Rotskoff K S.et al Effects of polyarticular and pauciarticular onset juvenile rheumatoid arthritis on facial and mandibular growth. J Rheumatol 199623159–165. [PubMed] [Google Scholar]
- 6.Ronchezel M V, Hilário M O E, Goldenberg J, Lederman H M, Faltin K, Jr, de Azevedo M F.et al Temporomandibular joint and mandibular growth alterations in patients with juvenile rheumatoid arthritis.J Rheumatol 1995221956–1961. [PubMed] [Google Scholar]
- 7.Twilt M, Mobers S M L M, Arends L R, tan Cate R, Van Suijlekom‐Smit L W A. Temporomandibular involvement in juvenile idiopathic arthritis. J Rheumatol 2004311418–1422. [PubMed] [Google Scholar]
- 8.Sidiropoulou‐Chatzigianni S, Papadopoulos M, Kolokithas G. Dentoskeletal morphology in children with juvenile idiopathic arthritis compared with healthy children. J Orthod 20012853–58. [DOI] [PubMed] [Google Scholar]
- 9.Kjellberg H, Kiliaridis S, Thilander B. Dentofacial growth in orthodontically treated children with juvenile chronic arthritis (JCA). A comparison with angle class II division 1 subjects. Eur J Orthod 199517357–373. [DOI] [PubMed] [Google Scholar]
- 10.Larheim T A, Haanes H R. Micrognathia, temporomandibular joint changes and dental occlusion in juvenile rheumatoid arthritis of adolescents and adults. Scand J Dent Res 198189329–338. [DOI] [PubMed] [Google Scholar]
- 11.Hanna V E, Rider S F, Moore T L, Wilson V K, Osborn T G, Totskoff K S.et al Effects of systemic onset juvenile rheumatoid arthritis on facial morphology and temporomandibular joint form and function. J Rheumatol 199623155–158. [PubMed] [Google Scholar]
- 12.Kjellberg H, Fasth A, Kiliaridis S, Wenneberg B, Thilander B. Craniofacial structure in children with juvenile chronic arthritis (JCA) compared with healthy children with ideal or postnormal occlusion. Am J Orthod Dentofac Orthoped 199510767–78. [DOI] [PubMed] [Google Scholar]
- 13.Jacobson A.Radiographic cephalometry. 1st ed. Illinois: Quintessence Publishing Co, 1995
- 14.Rohlin M, Petersson A. Rheumatoid arthritis of the temporomandibular joint: radiologic evaluation based on standard reference films. Oral Surg Oral Med Oral Pathol 198967594–599. [DOI] [PubMed] [Google Scholar]
- 15.Habets L L M H, Bezuur J N, Naeiji M, Hansson T L. The orthopantomogram, an aid in diagnosis of temporomandibular joint problems.II. The vertical symmetry. J Oral Rehabil 198815465–471. [DOI] [PubMed] [Google Scholar]
- 16.Riolo M L, Moyers R E, Mcnamara J A, Hunter J S.An atlas of craniofacial growth: cephalometric standards from the University school growth study. Ann harbor: Center for Human Growth and Development, University of Michigan, 1974, (Monograph No 2, Craniofacial growth series. )
- 17.Steiner C C. Cephalometrics for you and me. Am J Orthod 195339729–755. [Google Scholar]