Abstract
Objective
To assess the immediate effects of tumour necrosis factor α (TNFα) blockade on endothelial function in systemic vasculitis.
Methods
Endothelial function was assessed by laser Doppler flowmetry in patients with active vasculitis after 10 infusions of infliximab. For comparison endothelial responses were assessed after five infusions of cyclophosphamide plus methylprednisolone.
Results
Endothelial dependent vasodilatation (EDV) improved significantly within 24 hours of infliximab infusion. The median change in red blood cell flux (interquartile range) was 5.7 (4.3–8.2) before infusion v 8.4 (7.5–10.9) at 24 hours; p = 0.027. This was not maintained at day 14. No improvement was seen in EDV after cyclophosphamide plus methylprednisolone infusion.
Conclusion
The rapid but transient improvement in EDV after TNFα inhibition suggests that TNFα may have a direct role in the impairment of endothelial function.
Keywords: vasculitis, endothelial function, endothelial dependent vasodilatation, tumour necrosis factor α, anti‐tumour necrosis factor α treatment
Endothelial dependent vasodilatation (EDV) is impaired in patients with primary systemic vasculitis (PSV). This impairment occurs in a range of vasculitides and is seen in both medium sized muscular arteries and in the cutaneous microvasculature as assessed by flow mediated dilatation at the brachial artery and by acetylcholine (ACh) induced vasodilatation in the small vessels of the skin.1,2 Although nitric oxide (NO) mediated vasodilatation is the readout used in these in vivo assays of endothelial function, in fact NO is central to the regulation of other endothelial and vascular functions, such as leucocyte adhesion, platelet aggregation, and thrombosis, and the growth and migration of vascular smooth muscle cells.3 An impaired release of NO by vascular endothelium in patients with PSV therefore reflects a generalised perturbation in endothelial function in patients with this group of diseases. Similar endothelial dysfunction is seen in rheumatoid arthritis (RA), and we have suggested that this is fundamental to the link between RA and atherosclerosis.4
The mechanisms for this diffuse impairment in endothelial function remain unclear but are likely to be related to the inflammatory response occurring at distant sites of active vasculitis. Thus, in patients with vasculitis, it has been shown that brachial artery endothelial function improves after the induction of disease remission with cyclophosphamide and steroid.1 Tumour necrosis factor α (TNFα) is likely to have a mechanistic role in the impairment of endothelial function.5 Levels of TNFα are raised in PSV, and TNFα impairs endothelium dependent vasodilatation both in vitro and in human arteries in vivo.6,7 Local infusion of TNFα into the brachial artery depressed endothelial dependent vasodilatation, while no such effect was seen with interleukin 6, emphasising the central role of TNFα in endothelial dysfunction.7 We aimed at examining the time course of the immediate effects of TNFα blockade, induced by infliximab, on endothelial function in patients with PSV.
Patients and methods
Patients
Endothelial dependent vasodilatation and endothelial independent vasodilatation (EIV) were assessed by laser Doppler flowmetry (LDF) immediately before and at days 1, 2, 5, and 14 after the infusion of infliximab (5 mg/kg) in patients with PSV. No additional treatment was given for the vasculitis during the treatment course. Assessments were performed after a total of 10 infusions of infliximab in three patients. For comparison, EDV and EIV were studied before and at days 1, 2, 5, and 14 after treatment with cyclophosphamide (15 mg/kg) plus methylprednisolone (10 mg/kg) after a total of five infusions in three patients. As many of the patients studied were ill it was not possible to subject them to the full experimental protocol in all instances. We were unable to capture data at eight of the 50 possible assessment points from the patients treated with infliximab and at five of the 25 possible assessment points from the patients treated with cyclophosphamide plus methylprednisolone. No patients were taking angiotensin converting enzyme inhibitors, angiotensin II receptor antagonists, calcium channel blockers, β blockers, non‐steroidal anti‐inflammatory drugs or statins during the course of the study. All patients were normotensive and had serum creatinine levels within the normal range.
Details of the three patients treated with infliximab are as follows: three male; ages 29, 71, and 39 years; one with polyarteritis nodosa, two with Wegener's granulomatosis; Birmingham Vasculitis Activity Score (BVAS)8 at baseline 12, 14, and 10. Details of the three patients treated with cyclophosphamide and methylprednisolone are as follows: one male, two female; ages 29, 59, and 54 years; one with polyarteritis nodosa, one with Henoch‐Schönlein purpura, one with systemic lupus erythematosus associated vasculitis; BVAS at baseline 12, 6, and 5. All patients had previously been treated with conventional immunosuppressive drugs, including prednisolone, except for one patient with Wegener's granulomatosis for whom infliximab was the initial treatment. Ethical approval was obtained for the study and all subjects gave written informed consent.
Laser Doppler flowmetry
All LDF studies were performed in the morning in a vascular laboratory maintained at a constant temperature (25±1°C). Patients abstained from caffeine and smoking for 12 hours before each assessment. Subjects rested semirecumbent in light clothing for 20 minutes before assessment. Blood flow changes in the cutaneous microcirculation were assessed at clinically unaffected sites by LDF (DTR4, Moor Instruments, Axminster, Devon, UK) and recorded as red blood cell (RBC) flux. ACh (Miochol, CIBA Vision Ophthalmics, Southampton, UK), an endothelial dependent vasodilator, and sodium nitroprusside (SNP; David Bull Laboratories, Melbourne, Victoria, Australia), an endothelial independent vasodilator, were freshly prepared as 1% solutions in 0.5 molar saline (vehicle). The iontophoresis chamber was attached to the dorsum of a finger. The laser Doppler probe (MIC1, Moor Instruments) was incorporated in the centre of the chamber and RBC flux was recorded continuously from the area to which iontophoresis was applied. Vehicle alone, ACh, and SNP were administered by iontophoresis to different sites. Currents of increasing intensity and duration were delivered to give a charge of 1–16 mC and the peak response was recorded. RBC flux was recorded for 1 minute before iontophoresis and 2 minutes after iontophoresis. Baseline and maximum RBC flux were calculated for each period of iontophoresis. There were no significant changes in RBC flux after the iontophoresis of vehicle alone (data not shown). The change in RBC flux was calculated as the proportional change from baseline ((maximum flux−baseline flux)/baseline flux).
Statistical analysis
Results are presented as median and interquartile range (IQR). For patients treated with infliximab, results at days 1, 2, 5, and 14 were compared with results before treatment using Wilcoxon's signed rank test. Wilcoxon's signed rank test was not used to analyse the data for the patients treated with steroid and cyclophosphamide because with this sample size there was no possibility of achieving a significant result. The Friedman test was thus used instead. All results are presented as two tailed values and significance was inferred at p<0.05.
Results
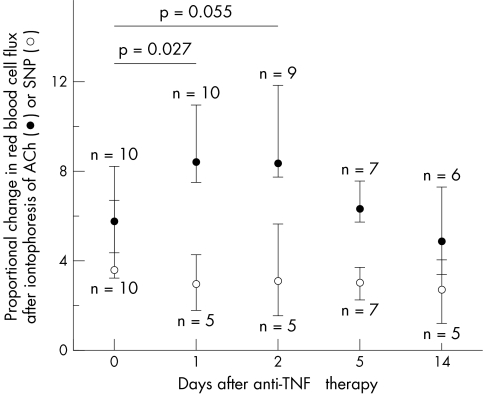
Rapid and statistically significant improvement in endothelial function occurred after treatment with infliximab. The improvement in EDV was apparent 24 hours after the infusion of infliximab (median change in RBC flux (IQR) 5.7 (4.3–8.2) before infusion v 8.4 (7.5–10.9) at 24 hours; p = 0.027) (fig 1). This improvement in EDV was maintained at 48 hours after the infusion of infliximab, though a comparison with preinfusion values just failed to reach significance at this time point (median change in flux (IQR): 5.7 (4.3–8.2) before infusion v 8.3 (7.7–11.8) at 48 hours; p = 0.055) (fig 1).
Figure 1 Proportional change in RBC flux after iontophoresis of ACh (closed circles) or SNP (open circles) in patients treated with infliximab.
Endothelial function subsequently declined and by days 5 and 14 was similar to that seen before infliximab infusion (fig 1). This pattern of transient improvement was essentially the same for the first and subsequent infusions. By contrast there was no change in EIV after infliximab treatment over this period (fig 1). In comparison, there was no significant change in EDV or EIV after treatment with cyclophosphamide plus methylprednisolone (Friedman test; although there were five missing data points, the 20 known values were such that the result could not be significant whatever the values of the missing data). EDV (median change in RBC flux) in this group was: before infusion, 8.8 (IQR 7.6–13.7); 24 hours, 6.9 (IQR 3.6–12.6); 48 hours, 12.8 (IQR 9.0–19.9); day 5, 7.2 (range 4.5–12.3); day 14, 6.6 (range 3.1–13.6).
Discussion
This pilot study shows that anti‐TNFα treatment leads to a rapid improvement in endothelial function in the cutaneous microvasculature in patients with PSV. This benefit is transient and not maintained at 2 weeks after treatment. Importantly, this improvement is not seen over an equivalent period of time after treatment with traditional intravenously administered immunosuppressive drugs used in PSV (cyclophosphamide plus methylprednisolone). This observation, that steroid and cyclophosphamide fail to improve endothelial function acutely in systemic vasculitis is consistent with studies which show that cortisol impairs endothelial function in healthy subjects.9,10 Previous reports of improvement in endothelial function with immunosuppressive regimens, whether they included TNFα blockade or not, have documented the change at a later time point, when clinical improvement had already occurred.1,11 Here we show a very rapid improvement in endothelial function within 24 hours of infliximab infusion, suggesting that TNFα may have a direct role in the impairment of endothelial function. The mechanisms underlying this effect deserve further investigation.
The principal limitation of this study is the relatively small number of patients in whom we were able to study the effects of infliximab treatment, though, importantly, the responses were consistent across infusions in individual patients. In addition, data were not available at all time points in all patients, and the patients and controls were not matched for sex or disease. However we note that the results are very similar to those reported in patients with RA treated with infliximab.12 In that study seven patients were assessed before infusion and at days 2, 7, and 28 after infusion and a significant improvement in endothelial function was seen at day 2, which had returned to baseline levels by day 28.
Endothelial dysfunction is an early event in atherosclerosis. Two studies have highlighted the increased incidence of subclinical atherosclerosis in PSV as shown by carotid artery intima media thickness.13,14 In addition, preliminary data suggest that the incidence of clinical atherosclerotic cardiovascular events is increased in PSV.13 Impaired endothelial function in patients with PSV may explain why an increased risk of atherosclerosis is associated with these conditions. The effect of tight control of disease activity and of anti‐TNFα treatment on cardiovascular outcomes in patients with PSV now deserves attention.
Acknowledgements
This study was supported by the Birmingham Arthritis Appeals Trust (BAAT).
Abbreviations
ACh - acetylcholine
BVAS - Birmingham Vasculitis Activity Score
EDV - endothelial dependent vasodilatation
EIV - endothelial independent vasodilatation
IQR - interquartile range
LDF - laser Doppler flowmetry
NO - nitric oxide
PSV - primary systemic vasculitis
RA - rheumatoid arthritis
RBC - red blood cell
SNP - sodium nitroprusside
TNFα - tumour necrosis factor α
Footnotes
Competing interests: Robert Stevens has been supported by Schering‐Plough to attend a conference.
References
- 1.Raza K, Thambyrajah J, Townend J N, Exley A R, Hortas C, Filer A.et al Suppression of inflammation in primary systemic vasculitis restores vascular endothelial function: lessons for atherosclerotic disease? Circulation 20001021470–1472. [DOI] [PubMed] [Google Scholar]
- 2.Filer A D, Gardner‐Medwin J M, Thambyrajah J, Raza K, Carruthers D M, Stevens R J.et al Diffuse endothelial dysfunction is common to ANCA associated systemic vasculitis and polyarteritis nodosa. Ann Rheum Dis 200362162–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Landmesser U, Hornig B, Drexler H. Endothelial function: a critical determinant in atherosclerosis? Circulation 2004109II27–II33. [DOI] [PubMed] [Google Scholar]
- 4.Bacon P A, Raza K, Banks M J, Townend J, Kitas G D. The role of endothelial cell dysfunction in the cardiovascular mortality of RA. Int Rev Immunol 2002211–17. [DOI] [PubMed] [Google Scholar]
- 5.Buckley C D, Ed Rainger G, Nash G B, Raza K. Endothelial cells, fibroblasts and vasculitis. Rheumatology (Oxford) 200544860–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wimalasundera R, Fexby S, Regan L, Thom S A, Hughes A D. Effect of tumour necrosis factor‐alpha and interleukin 1beta on endothelium‐dependent relaxation in rat mesenteric resistance arteries in vitro. Br J Pharmacol 20031381285–1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chia S, Qadan M, Newton R, Ludlam C A, Fox K A, Newby D E. Intra‐arterial tumor necrosis factor‐alpha impairs endothelium‐dependent vasodilatation and stimulates local tissue plasminogen activator release in humans. Arterioscler Thromb Vasc Biol 200323695–701. [DOI] [PubMed] [Google Scholar]
- 8.Luqmani R A, Bacon P A, Moots R J, Janssen B A, Pall A, Emery P.et al Birmingham Vasculitis Activity Score (BVAS) in systemic necrotizing vasculitis. QJM 199487671–678. [PubMed] [Google Scholar]
- 9.Broadley A J, Korszun A, Abdelaal E, Moskvina V, Jones C J, Nash G B.et al Inhibition of cortisol production with metyrapone prevents mental stress‐induced endothelial dysfunction and baroreflex impairment. J Am Coll Cardiol 200546344–350. [DOI] [PubMed] [Google Scholar]
- 10.Mangos G J, Walker B R, Kelly J J, Lawson J A, Webb D J, Whitworth J A. Cortisol inhibits cholinergic vasodilation in the human forearm. Am J Hypertens 2000131155–1160. [DOI] [PubMed] [Google Scholar]
- 11.Booth A D, Jayne D R, Kharbanda R K, McEniery C M, Mackenzie I S, Brown J.et al Infliximab improves endothelial dysfunction in systemic vasculitis: a model of vascular inflammation. Circulation 20041091718–1723. [DOI] [PubMed] [Google Scholar]
- 12.Gonzalez‐Juanatey C, Testa A, Garcia‐Castelo A, Garcia‐Porrua C, Llorca J, Gonzalez‐Gay M A. Active but transient improvement of endothelial function in rheumatoid arthritis patients undergoing long‐term treatment with anti‐tumor necrosis factor alpha antibody. Arthritis Rheum 200451447–450. [DOI] [PubMed] [Google Scholar]
- 13.Zaenker M, Aries P M, Herlyn K, Lamprecht P, Bacon P A, Gross W L. Accelerated atherosclerosis in Wegener's granulomatosis (WG): a sonographic case‐control study on intima media thickness [abstract]. Arthritis Rheum 200246(suppl)S185 [Google Scholar]
- 14.de Leeuw K, Sanders J S, Stegeman C, Smit A, Kallenberg C G, Bijl M. Accelerated atherosclerosis in patients with Wegener's granulomatosis. Ann Rheum Dis 200564753–759. [DOI] [PMC free article] [PubMed] [Google Scholar]