Abstract
Objective
To assess the safety of adalimumab in global clinical trials and postmarketing surveillance among patients with rheumatoid arthritis (RA).
Methods
Safety data for adalimumab treated patients from randomised controlled trials, open label extensions, and two phase IIIb open label trials were analysed. In addition, postmarketing spontaneous reports of adverse events in the United States were collected following Food and Drug Administration approval of adalimumab on 31 December 2002.
Results
As of 15 April 2005, the RA clinical trial safety database analysed covered 10 050 patients, representing 12 506 patient‐years (PYs) of adalimumab exposure. The rate of serious infections, 5.1/100 PYs, was comparable to that reported on 31 August 2002 (4.9/100 PYs), and to published reports of RA populations naive to anti‐tumour necrosis factor (TNF) therapy. Following implementation of tuberculosis (TB) screening in clinical trials, the rate of TB decreased. There were 34 cases of TB as of this analysis (0.27/100 PYs). The standardised incidence ratio for lymphoma was 3.19 (95% CI 1.78 to 5.26), consistent with the observed increased incidence in the general RA population. As of 30 June 2005, there were an estimated 78 522 PYs of exposure to adalimumab in the US postmarketing period. Seventeen TB cases were spontaneously reported (0.02/100 PYs) from the US. Rates of other postmarketing events of interest, such as congestive heart failure, systemic lupus erythematosus, opportunistic infections, blood dyscrasias, lymphomas, and demyelinating disease, support observations from clinical trials.
Conclusion
Analyses of these data demonstrate that long term adalimumab treatment is generally safe and well tolerated in patients with RA.
Keywords: adalimumab, postmarketing surveillance, rheumatoid arthritis, safety, tumour necrosis factor antagonists
More than 1 million patients have been treated with the three currently available tumour necrosis factor (TNF) antagonists (adalimumab, etanercept, and infliximab) for a variety of diseases.1,2,3 These agents provide considerable benefit to patients with rheumatoid arthritis (RA). In RA patients unresponsive to treatment with traditional disease modifying antirheumatic drugs (DMARDs), therapy with a TNF antagonist has been shown to improve clinical signs and symptoms4,5,6 and effectively inhibit radiographic progression.5,6,7 Etanercept and infliximab have been extensively studied during the past decade and have demonstrated acceptable profiles of safety and tolerability.8,9,10,11 Nonetheless, because of the seriousness and unexpected nature of certain adverse events (AEs) that have been seen with all three agents in this class, safety concerns persist. These AEs include serious infections,12 opportunistic infections including tuberculosis (TB),13 demyelinating disorders,14 systemic lupus erythematosus (SLE)/lupus‐like syndrome,15 and lymphoproliferative disorders.16
It is unclear whether treatment with TNF antagonists is responsible for some of these AEs or whether they are more directly attributable to the severity and duration of the disease itself. The majority of patients with RA who enrolled in clinical trials with TNF antagonists had already experienced treatment failure with multiple DMARDs and had exhibited moderately to severely active disease of long standing duration; many were concomitantly treated with methotrexate (MTX). These characteristics are associated with an increased risk for comorbidities such as serious infection,17,18 lymphoma,19 and cardiac disease,20 independent of any additional risk that may be related to anti‐TNF therapy. In addition, definitive conclusions about the relative safety of TNF antagonists, which have never been compared in a head to head trial, cannot be drawn. The large study size needed for a controlled trial to measure rare events, the differences in design and patient populations of trials that have already been completed, and the many complex variables inherent to postmarketing surveillance all constrain the interpretation and comparison of existing data.21
Adalimumab (HUMIRA, Abbott Laboratories, Illinois, USA) is the first and only fully human, anti‐TNF monoclonal antibody currently approved by the United States Food and Drug Administration (FDA; 31 December 2002) and by the European Medicines Agency (EMEA; 10 September 2003) for the treatment of RA. More than 110 000 patients worldwide have been prescribed adalimumab, which is commercially available in the US and 62 other countries. Adalimumab is indicated in the US for reducing signs and symptoms, inhibiting the progression of structural damage, and improving physical function in adult patients with moderately to severely active RA who have had an inadequate response to one or more DMARDs.22 It is also indicated as first line treatment for early RA, as well as for the treatment of psoriatic arthritis. Adalimumab can be used alone or in combination with MTX or other DMARDs. The safety profile of adalimumab has been extensively studied in randomised controlled trials (RCTs),4,7,23,24 and in long term, open label extension trials (OLE).25 This current report offers a comprehensive analysis of adalimumab safety data collected since adalimumab's first study use in humans in 1997 to the date of this analysis.
Methods
Analysis of adalimumab global safety in RA clinical trials
The clinical trial safety database analysed for this report included cumulative data for RA patients who participated in RCTs and subsequent OLEs. All RCT patients were eligible to enrol in extension trials during which they received adalimumab 40 mg subcutaneously every other week. The database analysed also included data from two 12 week, phase IIIb, open label trials: the Access to Therapy (Act) trial, conducted in the US, and the Research in Active RA (ReAct) trial, conducted at more than 400 sites across Europe and Australia. Each included RA patients with an inadequate response to at least one prior DMARD, including biologics. Adalimumab was added to existing antirheumatic therapies. In ReAct, patients who completed the initial 12 week treatment period entered an extension period and were followed until adalimumab was commercially available in their respective countries. This analysis does not include data from the clinical trial of adalimumab in early RA (PREMIER).
Rates of serious adverse events (SAEs) were tabulated as events per 100 patient‐years (E/100 PYs) of adalimumab exposure. In some cases, more than one event may have occurred in an individual patient. An SAE was defined according to regulatory criteria as an AE that was fatal or life threatening; required or prolonged inpatient hospitalisation; resulted in persistent or significant disability, congenital anomaly, birth defect, miscarriage, or elective abortion; or required medical/surgical intervention to prevent another serious outcome. The clinical trial safety database was assessed on 31 August 2002 for inclusion in a US regulatory safety update. Data from a cut‐off date of 15 April 2005 were used for the purpose of this report. Table 1 provides an overview of the number of patients and duration of adalimumab exposure at these time points.
Table 1 Adalimumab RA clinical safety database.
| Patients | Exposure (PYs) | |
|---|---|---|
| US regulatory safety update, | ||
| 31 August 2002 | ||
| Adalimumab | 2468 | 4870 |
| Placebo | 832 | 365 |
| Through 15 April 2005 | ||
| Open label extension studies | 2504 | 8047 |
| Act | 936 | 208 |
| ReAct | 6610 | 4251 |
| Total | 10 050 | 12 506 |
Act, Access to Therapy trial; PY, patient‐years; ReAct, Research in Active RA trial.
Tuberculosis screening
During the early phase of the adalimumab development program, study protocols did not include screening procedures for TB. For studies initiated after September 1999, protocols called for TB screening to be implemented. However, for patients who were already enrolled in ongoing adalimumab studies, no TB screening was required.
The type of screening initiated varied by location. For studies initiated in Europe where there has been extensive use of the Bacille Calmette Guerin (BCG) vaccine, TB screening consisted of a medical history and chest x ray (that is, no tuberculin skin test (TST) was required). After 2001, both a TST and a chest x ray were required. For studies initiated in the US and Canada, the screening procedure included a TST, and, when indicated, a chest x ray as well. Patients were excluded from studies if they had active TB. Most patients diagnosed with latent TB (LTB) received isoniazid prophylaxis prior to the first dose of adalimumab.
TST antigen for the skin test was obtained locally by the investigator and was not standardised across countries. Interpretation of a positive test was based on prevailing local guidelines, which varied among countries.
Malignancies
Cancer incidence rates and types were evaluated in all patients in the clinical trial safety database. Standardised incidence ratios (SIRs) were calculated to compare the incidence rates for adalimumab treated RA patients with the expected rates for the sex and age matched general population derived from the Surveillance, Epidemiology and End Results (SEER) database of the US National Cancer Institute.26 Patients less than 20 years of age were excluded for the SIR calculation as the population in the SEER database does not include those in this age group.
US postmarketing surveillance
The adalimumab postmarketing safety database contains spontaneous reports from health care providers, consumers, and medical literature that were received and reviewed since 31 December 2002 (when adalimumab received FDA approval for RA). The events were classified according to terms used by the reporter and coded using Medical Dictionary of Regulatory Activities (MedDRA) scientific terminology. As these were voluntary reports, additional information was requested, whenever necessary and possible, through direct contact with reporting physicians or patients, per standard procedures. All available US cases reported during the period of 31 December 2002 to 30 June 2005 were reviewed and analysed for this safety report. The data on particular event categories relevant to TNF antagonist therapy are presented as E/100 PYs based on estimated postmarketing patient‐year exposure. These must be interpreted in the context of the limitations of all postmarketing data collection, such as uncertain causality, incomplete medical information, under‐reporting, unverified diagnoses, duplicate reports, and confounders (for example, disease severity, concomitant medications).27
Results
Adalimumab global safety in RA clinical trials
As of 31 August 2002, 2468 patients with RA had received adalimumab in clinical trials, representing 4870 PYs of exposure (table 1). Through 15 April 2005, the date of this safety analysis, 10 050 patients (12 506 PYs) had participated in adalimumab RA clinical trials, more than 300 of whom have had at least 5 years of exposure to adalimumab. Four of the adalimumab RCTs were pivotal trials which have been published.4,7,23,24 Patients in the pivotal trials had moderately or severely active, long standing disease (average duration of approximately 11 years), and the majority had failed treatment with prior DMARDs. The rates for SAEs of interest reported in the clinical trial safety database (RCTs/OLEs, Act, and ReAct) as of April 2005 were compared with the rates reported 2.5 years earlier in August 2002 (table 2).
Table 2 Rates of selected adverse events.
| All RA trials as of 31 August 2002* (E/100 PYs) | All RA trials as of 15 April 2005† (E/100 PYs) | |
|---|---|---|
| Tuberculosis | 0.27 | 0.27 |
| Histoplasmosis | 0.06 | 0.03 |
| Demyelinating diseases | 0.08 | 0.08 |
| Lymphoma | 0.21 | 0.12 |
| SLE/lupus‐like syndrome | 0.08 | 0.10 |
| Congestive heart failure | 0.29 | 0.28 |
*n = 2468, 4870 PYs; †n = 10 050, 12 506 PYs.
E/100 PYs, events per 100 patient‐years.
Serious infections
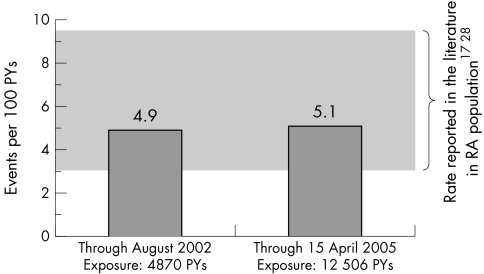
The rate of serious infections in the clinical trial safety database as of April 2005 was 5.1/100 PYs. This rate is nearly identical to that observed in August 2002 (4.9/100 PYs) and is similar to rates reported for the general RA population (fig 1).17,28 Four cases of histoplasmosis were reported, all in endemic areas (0.03/100 PYs). No cases of coccidioidomycosis have been reported in RA clinical trials.
Figure 1 Serious infection rates in adalimumab RA clinical trials.
Tuberculosis
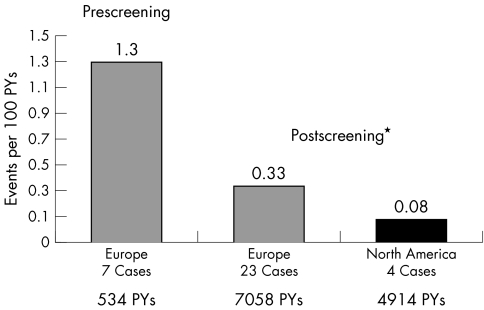
Prior to routine TB screening in adalimumab RA clinical trials, seven cases of TB were reported in Europe (fig 2), with 534 PYs of adalimumab exposure (1.3/100 PYs). Following the initiation of TB screening, 23 cases were reported in Europe, with 7058 PYs of exposure (0.33/100 PYs). As of this analysis, only four cases had been reported in North America after 4914 PYs of exposure (0.08/100 PYs). Retrospective analysis found variable TB screening practices. One of the four patients had a 9 mm PPD reading and did not receive TB preventive therapy prior to treatment with adalimumab.
Figure 2 TB rates in adalimumab RA clinical trials. *Rates after implementation of TB screening procedures.
Of the 866 patients who had received TB prophylaxis, five (0.6%) developed TB as of this analysis. All five patients, who were participants in the ReAct trial, had significant TST reactions (one with accompanying ulceration) but had no evidence of active TB based on chest x ray/thoracic imaging. TB prophylaxis was started at least a month prior to adalimumab therapy for these five patients.
Lymphoma
Ten cases of lymphoma were seen after 4870 PYs of adalimumab exposure (0.21/100 PYs); and 15 lymphomas were seen after 12 506 PYs of exposure (0.12/100 PYs). The following types of lymphoma were reported, none of which were predominant: Hodgkin's disease, B cell lymphoma, T cell lymphoma, central nervous system lymphoma, and mucosa associated lymphoid tissue (MALT) lymphoma. Analysis of the incidence of lymphoma in adalimumab clinical trials, in comparison with that of the normal population in the SEER database, resulted in an SIR of 3.19 (95% CI 1.78 to 5.26). This was consistent with SIRs reported for RA populations naive to anti‐TNF therapy (table 3).29,30,31,32
Table 3 Incidence of lymphoma in RA patients29,30,31,32.
| Study | Country | No. of patients with RA | Years of follow up, mean (max) | SIR for cancer | SIR for lymphoma (odds ratio/RA activity level) |
|---|---|---|---|---|---|
| Gridley et al29 | Sweden | 11 683 | 8.6 (20) | 1.0 | 2.0 |
| Mellemkjaer et al30 | Denmark | 20 699 | 7 (15) | 1.1 | 2.5 |
| Isomaki et al31 | Finland | 46 101 | 4.6 (7) | 1.1 | 2.7 |
| Adalimumab 2005 | Global | 10 024* | 1.2 (7.7) | 1.06 | 3.19 |
| 1.0 (low) | |||||
| Baecklund et al32 | Sweden | 11 683 | 8.6 (20) | – | 5.4 (medium) |
| 25.8 (high) |
*As of 15 April 2005.
Demyelinating disorders
Four cases of demyelinating disorder were reported among RA patients who had received adalimumab after 4870 PYs of adalimumab exposure (0.08/100 PYs). Ten cases were reported after 12 506 PYs of exposure (0.08/100 PYs): six cases of multiple sclerosis, two cases of non‐specific demyelination, and two cases of Guillain‐Barré syndrome.
SLE and lupus‐like syndrome
SLE and lupus‐like syndromes have rarely been associated with adalimumab in clinical trials and do not appear to be increasing in frequency (table 2). Four cases were reported after 4870 PYs of adalimumab exposure and 13 cases after 12 506 PYs. For those reported as SLE or lupus‐like syndrome, presenting manifestations were mostly cutaneous lesions, photosensitivity, and serositis (pleural and/or pericardial). One was a case of biopsy‐proven cutaneous lupus erythematosus. No significant internal organ involvement has been observed in any of these cases.
One patient was diagnosed with anti‐phospholipid antibody syndrome. Another patient was reported to have deep vein thrombosis associated with positive anti‐cardiolipin antibodies.
Congestive heart failure (CHF)
Forty four patients had a medical history of CHF, and three (7%) reported CHF events while in adalimumab trials. Thirty two cases of CHF were observed among 10 006 (0.3%) patients who did not report a medical history of CHF. In the overall RA clinical trial safety database, the rate of CHF was stable between the two time points of analysis that spanned more than 2.5 years (table 2).
US postmarketing surveillance
From 31 December 2002 to 30 June 2005, the estimated postmarketing patient exposure to adalimumab was 78 522 PYs. The US rates for events of interest to physicians prescribing TNF antagonists are shown in table 4.
Table 4 Selected events in the US postmarketing period: 31 December 2002 to 30 June 2005.
| AEs | Reported rates* (E/100 PYs) |
|---|---|
| Tuberculosis | 0.02 |
| Lymphoma | 0.04 |
| Congestive heart failure | 0.06 |
| Demyelinating disease | 0.01 |
| Systemic lupus erythematosus | 0.03 |
| Opportunistic infections | 0.06 |
| Blood dyscrasias | 0.08 |
*78 522 PYs.
Cumulatively, 17 cases of TB were reported in the defined postmarketing period (0.02/100 PYs), of which five had extrapulmonary involvement. Twenty five of the 46 opportunistic infections reported were candidiasis, of which 22 were localised oral/vaginal candidiasis. The remaining 21 reported opportunistic infections involved eight different organisms.
Discussion
TNF antagonist therapy has dramatically altered the therapeutic landscape in rheumatology. However, TNF antagonists are thought to be associated with AEs that, in a small percentage of patients, may reflect the same immunomodulatory properties mediating efficacy. These could be infections, including TB and opportunistic infections, or AEs resulting from inappropriate immune/inflammatory cell activity, such as lymphoma, autoimmune, and demyelinating diseases.
For this adalimumab safety report, two sources of information were used: the RA clinical trial safety database and US spontaneous postmarketing reports. From these sources, the rates of clinical trial SAEs and postmarketing AEs were found to be low and stable over time.
The increased risk for serious infection in patients with RA may be partly attributable to alterations in immunoregulation that accompany RA.33 However, additional risk factors include increased age, disease severity, comorbid illnesses (such as diabetes mellitus), and the use of corticosteroids or other immunosuppressive medications.18 Published cohort studies have tried to elucidate the risk of serious infection among infliximab treated and etanercept treated patients. Phillips et al34 found no difference in rates of infection before and after exposure to etanercept, while Kroesen et al12 demonstrated an increase in the rate of serious infection from 0.008 events/year before therapy with infliximab and etanercept, to 0.181 events/year after TNF antagonist therapy exposure. The British Society of Rheumatology Biologics Register estimated the incidence rate of serious infections with the use of biologic agents to be 5.0–6.5/100 PYs, with no significant differences between adalimumab, etanercept, and infliximab.35 The rates of serious infections in adalimumab treated patients from the adalimumab clinical trial safety database were 4.9/100 PYs on 31 August 2002, and 5.1/100 PYs on 15 April 2005. These rates fall within the range of serious infection rates observed for the general RA population naive to TNF antagonists (fig 1).17,28 The stability of the adalimumab rate over time shows that, as OLE experience accrued in the years following RCT exposure, serious infections did not become more frequent. These data also suggest that the administration of adalimumab in clinical trials did not increase the rate of serious infections beyond that expected without adalimumab. Nonetheless, the risk for serious infections with anti‐TNF therapy should be discussed with patients, especially those on concomitant immunosuppressive medications and those who have predisposing comorbid illnesses.
TNF plays a role in host defence against Mycobacterium tuberculosis by mediating granuloma homeostasis and containment of latent disease.36 Cases of TB have been documented in patients treated with TNF blockade with etanercept, infliximab, and adalimumab.37 It is believed that most such cases are a result of reactivation of LTB. Accordingly, the labels of all three TNF antagonists carry a warning regarding the increased risk of TB, and the Centers for Disease Control (CDC) recommend all patients be screened for TB prior to initiating anti‐TNF therapy.38 During the first 534 PYs of adalimumab exposure in clinical trials, screening for TB was not required and seven TB cases were reported, all in Europe (1.3/100 PYs). After routine TB screening was introduced in adalimumab clinical trials, the rate of TB was 0.33/100 PYs in Europe as of April 2005. This 75% decrease in the overall rate of TB in clinical trials in Europe may underestimate the true effectiveness of screening because several of the postscreening cases could have been detected by more stringent screening criteria. The incidence in North America is lower, with four cases representing a rate of 0.08/100 PYs. In this regard, the CDC recommends that induration ⩾5 mm diameter be considered a positive PPD result in immunosuppressed patients, such as those with RA.38 The importance of applying a high level of vigilance, conducting careful histories, and initiating prophylactic TB treatment for LTB prior to anti‐TNF therapy cannot be overemphasised. The duration of treatment for LTB needed before TNF antagonist therapy can be safely administered is uncertain because of a lack of published data that could guide clinical decisions.
Opportunistic infections have been reported with the use of all three TNF antagonists.37 They include histoplasmosis, listeriosis, pulmonary aspergillosis, and Pneumocystis carinii pneumonia. In the adalimumab clinical trial safety database as of April 2005, four cases of histoplasmosis (0.03/100 PYs) were seen, all in endemic areas. In the US postmarketing database, opportunistic infections had an overall rate of 0.06/100 PYs and included infections from nine different organisms. These results confirm that opportunistic infections can occur in patients receiving adalimumab, but they appear to be infrequent and involve a variety of organisms.
Both the present analysis of adalimumab and previous studies of other TNF antagonists have found no association between TNF antagonist therapy and non‐lymphomatous cancers. Several reports show that, in the absence of TNF antagonists, the risk for lymphoma in patients with RA is more than double that of the general population (table 3).29,30,31,32 Risk factors thought to be associated with this increased rate of lymphoma are the severity and duration of the disease. A case‐control study of RA patients found that the odds ratio for lymphoma was increased approximately 5‐ or 25‐fold for patients whose RA disease activity over time was moderate or high, respectively.32
Most patients in adalimumab clinical trials had moderately to severely active RA at study entry, which increased their risks for lymphoma. The SIR of 3.19 for lymphoma in adalimumab treated patients is consistent with that expected in RA patients naive to TNF antagonists. During a March 2003 FDA advisory meeting, the lymphoma SIR reported in RA clinical trials was 6.35 for infliximab and 3.47 for etanercept.39 Given the unprecedented efficacy of TNF antagonists compared with traditional DMARDs in controlling RA disease activity, what remains to be seen with long term observations is whether or not anti‐TNF therapy can actually lower the risk for lymphoma in RA.
Demyelinating disease was seen infrequently with adalimumab, both in clinical trials and in US postmarketing reports. Some cases occurred in patients with evidence of neurologic symptoms prior to initiation of adalimumab therapy. This indicates that caution is warranted when initiating the use of anti‐TNF therapy in patients with symptoms suggestive of pre‐existing central nervous system disease.14
Analyses of safety data from adalimumab global clinical trials and US postmarketing reports show that adalimumab therapy is generally safe and well tolerated in patients with RA. There were no new safety signals that suggest a considerable difference compared with other TNF antagonists. Furthermore, the rates of serious infections and lymphoma for patients treated with adalimumab appear to be similar to those reported for the general RA population, as well as for patients treated with etanercept or infliximab. As with any anti‐TNF agent, it would be prudent for physicians and patients alike to remain vigilant in monitoring for serious and opportunistic infections, as well as lymphoma. Overall, the relatively low rates of occurrence of these SAEs with adalimumab therapy do not appear to outweigh the substantial clinical benefits adalimumab offers the RA population.
Acknowledgements
The authors thank Michael Nissen, ELS, of Abbott Laboratories; and Discovery International of Chicago for their writing and editorial assistance in the development of this manuscript. The authors also thank Joseph Beason of Abbott Laboratories for his assistance with data acquisition.
Abbreviations
AE - adverse event
CDC - Centers for Disease Control
CHF - congestive heart failure
DMARD - disease modifying antirheumatic drug
E/100 PYs - events per 100 patient‐years
FDA - Food and Drug Administration
LTB - latent TB
MTX - methotrexate
OLE - open label extension trial
PY - patient‐year
RA - rheumatoid arthritis
RCT - randomised controlled trial
SAE - serious adverse event
SEER - Surveillance, Epidemiology and End Results
SIR - standardised incidence ratio
SLE - systemic lupus erythematosus
TB - tuberculosis
TNF - tumour necrosis factor
TST - tuberculin skin test
Footnotes
Competing interests: none declared
References
- 1.Abbott Laboratories HUMIRA® (adalimumab). Information available at: www.humira.com (accessed 2 February 2006)
- 2.Wyeth Pharmaceuticals Inc Enbrel: Etanercept. Information available at: www.enbrel.com (accessed 2 February 2006)
- 3.Centocor, Inc Remicade: Infliximab. Information available at: www.remicade.com (accessed 2 February 2006)
- 4.Weinblatt M E, Keystone E C, Furst D E, Moreland L W, Weisman M H, Birbara C A.et al Adalimumab, a fully human anti‐tumor necrosis factor alpha monoclonal antibody, for the treatment of rheumatoid arthritis in patients taking concomitant methotrexate: the ARMADA trial. Arthritis Rheum 20034835–45. [DOI] [PubMed] [Google Scholar]
- 5.Bathon J M, Martin R W, Fleischmann R M, Tesser J R, Schiff M H, Keystone E C.et al A comparison of etanercept and methotrexate in patients with early rheumatoid arthritis. N Engl J Med 20003431586–1593. [DOI] [PubMed] [Google Scholar]
- 6.Lipsky P E, van der Heijde D M F M, St Clair E W, Furst D E, Breedveld F C, Kalden J R.et al Infliximab and methotrexate in the treatment of rheumatoid arthritis. N Engl J Med 20003431594–1602. [DOI] [PubMed] [Google Scholar]
- 7.Keystone E C, Kavanaugh A F, Sharp J T, Tannenbaum H, Hua Y, Teoh L S.et al Radiographic, clinical, and functional outcomes of treatment with adalimumab (a human anti‐tumor necrosis factor monoclonal antibody) in patients with active rheumatoid arthritis receiving concomitant methotrexate therapy: a randomized, placebo‐controlled, 52‐week trial. Arthritis Rheum 2004501400–1411. [DOI] [PubMed] [Google Scholar]
- 8.Lebwohl M, Gottlieb A, Wallis W, Zitnik R. Safety and efficacy of over 7 years of etanercept therapy in a global population of patients with rheumatoid arthritis. J Am Acad Dermatol 200552(Suppl 1)P195 [Google Scholar]
- 9.Maini R N, Breedveld F C, Kalden J R, Smolen J S, Furst D, Weisman M H.et al Sustained improvement over two years in physical function, structural damage, and signs and symptoms among patients with rheumatoid arthritis treated with infliximab and methotrexate. Arthritis Rheum 200450(4)1051–1065. [DOI] [PubMed] [Google Scholar]
- 10.Fleischmann R, Stern R, Iqbal I. Etanercept — review of efficacy and safety after five years of clinical use. Therapy 2004111–23. [Google Scholar]
- 11.Genovese M C, Bathon J M, Fleischmann R M, Moreland L W, Martin R W, Whitmore J B.et al Long‐term safety, efficacy and radiographic outcomes with etanercept treatment in patients with early rheumatoid arthritis. J Rheumatol 2005321232–1242. [PubMed] [Google Scholar]
- 12.Kroesen S, Widmer A F, Tyndall A, Hasler P. Serious bacterial infections in patients with rheumatoid arthritis under anti‐TNF‐alpha therapy. Rheumatology 200342617–621. [DOI] [PubMed] [Google Scholar]
- 13.Bieber J, Kavanaugh A. Consideration of the risk and treatment of tuberculosis in patients who have rheumatoid arthritis and receive biologic treatments. Rheum Dis Clin North Am 200430257–270. [DOI] [PubMed] [Google Scholar]
- 14.Mohan N, Edwards E T, Cupps T R, Oliverio P J, Sandberg G, Crayton H.et al Demyelination occurring during anti‐tumor necrosis factor alpha therapy for inflammatory arthritides. Arthritis Rheum 2001442862–2869. [DOI] [PubMed] [Google Scholar]
- 15.Charles P J, Smeenk R J, De Jong J, Feldmann M, Maini R N. Assessment of antibodies to double‐stranded DNA induced in rheumatoid arthritis patients following treatment with infliximab, a monoclonal antibody to tumor necrosis factor alpha: findings in open‐label and randomized placebo‐controlled trials. Arthritis Rheum 2000432383–2390. [DOI] [PubMed] [Google Scholar]
- 16.Wolfe F, Michaud K. Lymphoma in rheumatoid arthritis: the effect of methotrexate and anti‐tumor necrosis factor therapy in 18,572 patients. Arthritis Rheum 2004501740–1751. [DOI] [PubMed] [Google Scholar]
- 17.Doran M F, Crowson C S, Pond G R, O'Fallon W M, Gabriel S E. Frequency of infection in patients with rheumatoid arthritis compared with controls: a population‐based study. Arthritis Rheum 2002462287–2293. [DOI] [PubMed] [Google Scholar]
- 18.Doran M F, Crowson C S, Pond G R, O'Fallon W M, Gabriel S E. Predictors of infection in rheumatoid arthritis. Arthritis Rheum 2002462294–2300. [DOI] [PubMed] [Google Scholar]
- 19.Baecklund E, Askling J, Rosenquist R, Ekbom A, Klareskog L. Rheumatoid arthritis and malignant lymphomas. Curr Opin Rheumatol 200416254–261. [DOI] [PubMed] [Google Scholar]
- 20.Wolfe F, Michaud K. Heart failure in rheumatoid arthritis: rates, predictors, and the effect of anti‐tumor necrosis factor therapy. Am J Med 2004116305–311. [DOI] [PubMed] [Google Scholar]
- 21.Fleischmann R M. Examining the efficacy of biologic therapy: are there real differences? J Rheumatol 200229(S65)27–32. [PubMed] [Google Scholar]
- 22.Abbott Laboratories HUMIRA® (adalimumab) [prescribing information]. Abbott Park, IL: Abbott Laboratories, October, 2005
- 23.Furst D E, Schiff M H, Fleischmann R M, Strand V, Birbara C A, Compagnone D.et al Adalimumab, a fully human anti tumor necrosis factor‐alpha monoclonal antibody, and concomitant standard antirheumatic therapy for the treatment of rheumatoid arthritis: results of STAR (Safety Trial of Adalimumab in Rheumatoid Arthritis). J Rheumatol 2003302563–2571. [PubMed] [Google Scholar]
- 24.van de Putte L B, Atkins C, Malaise M, Sany J, Russell A S, van Riel P L.et al Efficacy and safety of adalimumab as monotherapy in patients with rheumatoid arthritis for whom previous disease modifying antirheumatic drug treatment has failed. Ann Rheum Dis 200463508–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schiff M H, Burmester G R, Pangan A L, Kupper H, Spencer‐Green G T. Global safety in adalimumab (HUMIRA®) rheumatoid arthritis clinical trials. Arthritis Rheum 200450(Suppl)S562 (poster presentation 1472 at the 2004 Annual Scientific Meeting of the American College of Rheumatology, 16–21 October 2004, San Antonio, TX) [Google Scholar]
- 26.NCI Surveillance, Epidemiology and End Results (SEER) Program Public‐Use Data (1973–1999). National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch, released April 2002, based on the November 2001 submission
- 27.Brewer T, Colditz G A. Postmarketing surveillance and adverse drug reactions: current perspectives and future needs. JAMA 1999281824–829. [DOI] [PubMed] [Google Scholar]
- 28.Singh G, Ramey D, Rausch P, Schettler J. Serious infections in rheumatoid arthritis: relationship to immunosuppressive use. Arthritis Rheum 199942(Suppl)S242 (abstract 1029 at the 1999 Annual Scientific Meeting of the American College of Rheumatology, 13–17 November 1999, Boston, MA) [Google Scholar]
- 29.Gridley G, McLaughlin J K, Ekbom A, Klareskog L, Adami H O, Hacker D G.et al Incidence of cancer among patients with rheumatoid arthritis. J Natl Cancer Inst 199385307–311. [DOI] [PubMed] [Google Scholar]
- 30.Mellemkjaer L, Linet M S, Gridley G, Frisch M, Moller H, Olsen J H. Rheumatoid arthritis and cancer risk. Eur J Cancer 199632A1753–1757. [DOI] [PubMed] [Google Scholar]
- 31.Isomaki H A, Hakulinen T, Joutsenlahti U. Excess risk of lymphomas, leukemia and myeloma in patients with rheumatoid arthritis. J Chronic Dis 197831691–696. [DOI] [PubMed] [Google Scholar]
- 32.Baecklund E, Ekbom A, Sparen P, Feltelius N, Klareskog L. Disease activity and risk of lymphoma in patients with rheumatoid arthritis: nested case‐control study. BMJ 1998317180–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Koetz K, Bryl E, Spickschen K, O'Fallon W M, Goronzy J J, Weyand C M. T cell homeostasis in patients with rheumatoid arthritis. Proc Natl Acad Sci U S A 2000979203–9208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Phillips K, Husni M E, Karlson E W, Coblyn J S. Experience with etanercept in an academic center: are infection rates increased? Arthrits Care Res 20024717–21. [DOI] [PubMed] [Google Scholar]
- 35.Dixon W, Hyrich K, Watson K, Silman A, Symmons D, the BSR Biologics Register Serious infection rates in patients receiving biologic therapy in the United Kingdom: results from the BSR Biologic Register (BSRBR). Rheumatology 200544(Suppl 1)i11 [Google Scholar]
- 36.Gardam M A, Keystone E C, Menzies R, Manners S, Skamene E, Long R.et al Anti‐tumor necrosis factor agents and tuberculosis risk: mechanisms of action and clinical management. Lancet Infect Dis 20033148–155. [DOI] [PubMed] [Google Scholar]
- 37.Keystone E C. Safety of biologic therapies ― an update. J Rheumatol 200532(Suppl)8–12. [PubMed] [Google Scholar]
- 38. Tuberculosis associated with blocking agents against tumor necrosis factor‐alpha — California, 2002–2003. MMWR Morb Mortal Wkly Rep 200453(30)683–686. [PubMed] [Google Scholar]
- 39. FDA Briefing Document. Update on the TNF blocking agents. FDA 3–4–2003. Available at: http://www.fda.gov/ohrms/dockets/ac/03/briefing/3930B1_01_B‐TNF.Briefing.pdf (accessed 6 February 2006)