Abstract
Background
There has been a lack of appropriate classification criteria for vasculitis in children.
Objective
To develop a widely accepted general classification for the vasculitides observed in children and specific and realistic classification criteria for common childhood vasculitides (Henoch‐Schönlein purpura (HSP), Kawasaki disease (KD), childhood polyarteritis nodosa (PAN), Wegener's granulomatosis (WG), and Takayasu arteritis (TA)).
Methods
The project was divided into two phases: (1) the Delphi technique was used to gather opinions from a wide spectrum of paediatric rheumatologists and nephrologists; (2) a consensus conference using nominal group technique was held. Ten international experts, all paediatricians, met for the consensus conference. Agreement of at least 80% of the participants was defined as consensus.
Results
Consensus was reached to base the general working classification for childhood vasculitides on vessel size. The small vessel disease was further subcategorised into “granulomatous” and “non‐granulomatous.” Final criteria were developed to classify a child as HSP, KD, childhood PAN, WG, or TA, with changes introduced based on paediatric experience. Mandatory criteria were suggested for all diseases except WG.
Conclusions
It is hoped that the suggested criteria will be widely accepted around the world because of the reliable techniques used and the international and multispecialist composition of the expert group involved.
Keywords: child, vasculitis, classification, childhood polyarteritis nodosa
Vasculitis is defined as inflammation of blood vessels.1 Although many vasculitides affect both adults and children, some, such as Kawasaki disease, occur almost exclusively in childhood. Other vasculitides (for example, temporal arteritis) rarely if ever occur in childhood, and others, like polyarteritis and Wegener's granulomatosis, have different aetiological, clinical, and prognostic characteristics in children.1,2 Thus it is inappropriate to apply adult classification criteria to vasculitis occurring in childhood. The chair of the working group on vasculitis of the Paediatric Rheumatology European Society (PReS) chair of Standing Committee on Paediatric Rheumatology in EULAR invited colleagues in the American College of Rheumatology (ACR) and European Society of Paediatric Nephrology (ESPN) to participate in the development of a classification specific for childhood vasculitis with the endorsement of the European League against Rheumatism (EULAR).
The objective was to reach consensus on a working general classification for the vasculitides observed in children, and on specific, realistic, and appropriate classification criteria for each category of vasculitic disease.
Methods
The overall goal of the project was to reach a consensus on classification criteria for childhood vasculitis that can be applied easily, mainly for research purposes, and that would be widely accepted. For this specific project it was decided to involve an international group of experts with extensive clinical experience of childhood vasculitis.
The Delphi and nominal group techniques (NGT)3,4 were used. The Delphi technique involves a series of well defined questionnaire based surveys. NGT is a structured face to face meeting designed to facilitate reaching consensus on the topic field of study. Consensus formation methodology must be designed so that each step is based on the results of the previous steps.
These techniques have been widely used in the past in the rheumatological medical literature for juvenile arthritis,5 juvenile systemic lupus erythematosus (SLE) and juvenile dermatomyositis,6 adult rheumatoid arthritis,7 and adult SLE8 A modified nominal group technique was used in the international consensus conference for the nomenclature of systemic (adult) vasculitides at Chapel Hill.9
The project was divided into two phases. In the first phase the Delphi technique was used to gather opinions from a wide range of paediatric rheumatologists and nephrologists. The second phase involved a consensus conference using NGT.
In the first phase paediatric rheumatologists and nephrologists were contacted at addresses obtained through the respective professional societies or bulletin boards within Europe and North and South America. The participants were members of the PReS and ESPN, as well as members of the “Pediatric Rheumatology Listserve.” A four page email survey was devised in which recipients were asked the following:
To choose the best working general classification for the vasculitides observed in children. For this purpose the participants were asked to choose between the criteria suggested by the Chapel Hill Consensus Conference,9 a modification for the Chapel Hill criteria,9 the modification of the Fink criteria by Dillon,1 and a classification proposed by Lie.10
To evaluate classification criteria for five important vasculitic diseases to determine whether each criterion in the existing classifications was appropriate for application in the paediatric population, and to suggest new criteria that should be included. The American College of Rheumatology criteria for Henoch‐Schönlein purpura (HSP),11 Takayasu arteritis (TA),12 Wegener's granulomatosis (WG),13 and polyarteritis nodosa (PAN)14 were reviewed by this process. The recipients were also asked for their opinion on the criteria for Kawasaki disease (KD),15 and the criteria for childhood PAN suggested by Brogan et al16 and Ozen et al.17 We did not work on the classification of very rare vasculitides or those where attempts had already been made, such as angiitis of the central nervous system.
Subsequently, a second questionnaire was sent to participants who were going to attend the consensus conference. Participants were provided with background information on the responses from the first Delphi survey plus copies of other relevant reports9,10,11,12,13,14,15,16,17 to help assess classification criteria with regard to specificity and sensitivity (if available information existed), and their clinical usefulness in current clinical practice. The general objectives of these surveys were to obtain information on how well the current classification criteria were accepted in the international community and in what ways they could be modified beneficially for paediatric practice.
In the second phase of the project a consensus conference was convened in Vienna on 12–13 June 2005 with the financial support of EULAR, PReS, and the ACR The group consisted of 10 paediatricians (predominantly rheumatologists and nephrologists) from nine different countries from Europe (including Turkey), North America, and Asia (India and Japan). The chosen participants were experienced paediatricians, usually rheumatologists and nephrologists, chosen by the respective organisations based on experience, publications, and reputation. A moderator with expertise in NGT (NR) oversaw the implementation of this format at the meeting. The participants were asked to reach the final consensus based on the information gathered from the previous surveys, the medical literature, and clinical and scientific expertise. Attendees were asked to express their opinion in round robin guided discussion. Agreement of at least 80% of the participants was defined as consensus.
Results
Phase 1: Results of surveys through electronic mail
The majority of the responses were from paediatric rheumatologists. There was a good distribution among the pediatricians practising worldwide. The modification of the Chapel Hill classification was favoured by the most respondents (table 1). Various new criteria were suggested and others resulted in modification of existing criteria. New criteria suggested by at least 10 respondents were included in the second survey sent to the consensus conference members. In addition, two variables that were suggested by fewer than 10 respondents were also included as they were regarded as important.
Table 1 Responses to the suggested classifications.
| Classification | Survey 1 | Survey 2 | |
|---|---|---|---|
| Chapel Hill criteria 19949 | 25.5% | 18% | |
| Classification of Fink 86 modified by Dillon 981 | 27% | 27% | |
| Classification of Lie (1986–1991)10 | 11% | – | |
| Modified Chapel Hill criteria for children | 36% | 54% | |
| Total | 100% | 100% |
Values are percentages of respondents favouring the classifications. Superscript numbers are reference numbers.
In the second survey all participants agreed to revise the general classification for the vasculitides observed in children, and the existing classification criteria for five childhood vasculitic diseases. A majority of the respondents agreed that the modified Chapel Hill version was the most appropriate among the various alternative schemes that were detailed in the questionnaire, but with some additions and modifications.
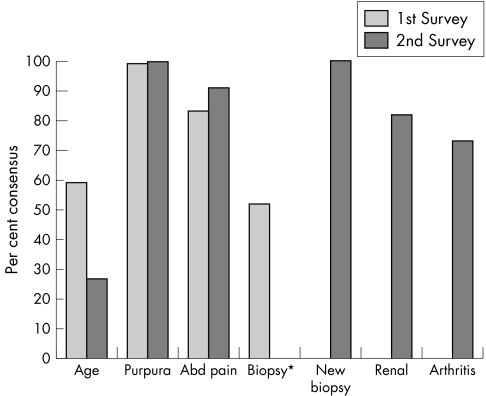
The types of response are summarised in fig 1.
Figure 1 Example of responses to the surveys regarding classification criteria for Henoch‐Schönlein purpura. The y axis represents percentage consensus. Renal involvement and arthritis were suggested by respondents of the first survey and thus were included in the subsequent second survey. According to the responses concerning the importance of IgA deposition, the “new biopsy” definition in the second survey was sent as “Any biopsy showing IgA deposition.” Respondents also considered renal involvement and arthritis in the second survey and over 80% agreed to add these as new classification criteria. *The original definition of the biopsy was assessed as “vessel wall granulocytes on biopsy” in the first survey.
Phase 2: Consensus conference
The members of the group reached consensus first on the specific classification criteria for each disease under discussion (HSP, KD, PAN, WG, and TA) and then on the best classification for paediatric vasculitides. Consensus was reached for all the diseases under discussion.
GENERAL CLASSIFICATION OF THE VASCULITIDES OF CHILDHOOD
There was a general consensus, both during the mail surveys and at the consensus meeting, to use vessel size for classification purposes, as suggested at the Chapel Hill Consensus Conference for adult vasculitides. Thus the consensus group members used this framework when formulating a general classification for the vasculitides observed in childhood. Only paediatric diseases were considered. The members reached consensus on the need for “small vessel disease” to be subcategorised into “granulomatous” and “non‐granulomatous” varieties (table 2). It was also agreed by all members that a group of “other vasculitides” was required, into which diseases were placed that did not fit into any one category, or fitted into more than one category, or where an aetiological process was defined.
Table 2 New classification of childhood vasculitis.
| I Predominantly large vessel vasculitis |
| • Takayasu arteritis |
| II Predominantly medium sized vessel vasculitis |
| • Childhood polyarteritis nodosa |
| • Cutaneous polyarteritis |
| • Kawasaki disease |
| III Predominantly small vessels vasculitis |
| (A) granulomatous |
| • Wegener's granulomatosis |
| • Churg‐Strauss syndrome |
| (B) non‐granulomatous |
| • Microscopic polyangiitis |
| • Henoch‐Schönlein purpura |
| • Isolated cutaneous leucocytoclastic vasculitis |
| • Hypocomplementic urticarial vasculitis |
| IV Other vasculitides |
| • Behçet disease |
| • Vasculitis secondary to infection (including hepatitis B associated polyarteritis nodosa), malignancies, and drugs, including hypersensitivity vasculitis |
| • Vasculitis associated with connective tissue diseases |
| • Isolated vasculitis of the central nervous system |
| • Cogan syndrome |
| • Unclassified |
CLASSIFICATION CRITERIA FOR CHILDHOOD VASCULITIDES
Henoch‐Schönlein purpura
To fulfil classification criteria for HSP by the existing ACR criteria, two of the following were required: age less than 20 years, palpable purpura, abdominal pain, and vessel wall granulocytes on biopsy.11
All members agreed that the existing ACR criteria needed to be revised. The age criterion was deleted. The Delphi surveys highlighted the need to include “predominant IgA deposition” in the definition of the criterion describing “biopsy”. The surveys also suggested the addition of arthritis and renal involvement to the group of criteria. The group reached consensus on these points, and table 3 is the agreed modified classification criteria for HSP.
Table 3 Classification criteria for Henoch‐Schönlein purpura.
| Palpable purpura (mandatory criterion) in the presence of at least one of the following four features: |
| • Diffuse abdominal pain |
| • Any biopsy showing predominant IgA deposition |
| • Arthritis* or arthralgia |
| • Renal involvement (any haematuria and/or proteinuria) |
*Acute, any joint.
Kawasaki disease
The Japanese classification for KD requires the presence of five of the following six criteria: characteristic fever, bilateral conjunctivitis, changes of lips and oral cavity, polymorphous exanthema, changes of peripheral extremities, and cervical lymphadenopathy.18 The American classification differs in that fever plus four of the remaining five criteria are required. This format was adopted as the basis of the present revision.
Two modifications were made (table 4). The presence of perineal desquamation was added to the criterion describing changes in the extremities. In acknowledgement of the importance of coronary artery disease in defining KD,18,19 it was agreed that in the presence of fever and coronary arterial involvement demonstrated by echocardiography, fewer than four of the remaining five are needed to classify a patient as having KD. The precise number of criteria required for classification in the presence of coronary artery involvement was not defined and will be determined in a proposed validation study.
Table 4 Classification criteria for Kawasaki disease.
| Fever persisting for at least five days (mandatory criterion) plus four of the following five features: |
| • Changes in peripheral extremities or perineal area |
| • Polymorphous exanthema |
| • Bilateral conjunctival injection |
| • Changes of lips and oral cavity: injection of oral and pharyngeal mucosa |
| • Cervical lymphadenopathy |
| In the presence of coronary artery involvement(detected on echocardiography)and fever, fewer than four of the remaining five criteria are sufficient (the exact number of criteria required is to be defined in the validation phase). |
Childhood polyarteritis nodosa
The criteria for PAN in childhood proposed by Brogan et al16 and Ozen et al17 are modifications of the ACR criteria.14 It was agreed that none of these criteria was sufficient to classify children with PAN. Thus each criterion of the existing classifications were re‐evaluated using the nominal group technique, using the available data from the PReS registry of 110 patients2 to calculate sensitivity and specificity, as well as the clinical experience of the participants in the consensus meeting. Several modifications were made. One criterion in the ACR classification—positivity for hepatitis B surface antigen or antibody—was deleted. The role of hepatitis B was recognised in the classification (under vasculitides associated with infection). Other criteria were modified so that they are appropriate for the paediatric population (table 5).
Table 5 Classification criteria for childhood polyarteritis nodosa.
| A systemic illness characterised by the presence of either a biopsy showing small and mid‐size artery necrotising vasculitis OR angiographic abnormalities* (aneurysms or occlusions) (mandatory criteria), plus at least two of the following: |
| • Skin involvement (livedo reticularis, tender subcutaneous nodules, other vasculitic lesions) |
| • Myalgia or muscle tenderness |
| • Systemic hypertension, relative to childhood normative data |
| • Mononeuropathy or polyneuropathy |
| • Abnormal urine analysis and/or impaired renal function† |
| • Testicular pain or tenderness |
| • Signs or symptoms suggesting vasculitis of any other major organ system (gastrointestinal, cardiac, pulmonary, or central nervous system) |
*Should include conventional angiography if magnetic resonance angiography is negative.
†Glomerular filtration rate of less than 50% normal for age.
To classify a child as having PAN requires a biopsy that shows small and mid‐size artery necrotising vasculitis or angiographic abnormalities (aneurysms or occlusions) in addition to at least two of the systemic features shown in table 5.
Cutaneous polyarteritis
The group agreed that a second category of necrotising vasculitis was necessary to describe the following clinical and laboratory features seen in childhood, as distinct from the systemic illness of childhood PAN:
cutaneous polyarteritis characterised by the presence of subcutaneous nodular, painful, non‐purpuric lesions with or without livedo reticularis, with no systemic involvement (except for myalgia, arthralgia, and non‐erosive arthritis);
skin biopsy showing necrotising non‐granulomatous vasculitis;
negative tests for antineutrophil cytoplasmic antibodies (ANCA);
cutaneous polyarteritis associated with serological or microbiological evidence of streptococcal infection.
No formal classification criteria were proposed beyond this definition of a clinical syndrome.
Microscopic polyangiitis
The group also proposed a third category of necrotising vasculitis, microscopic polyangiitis, as this has clinical and laboratory features distinct from the above two categories. Microscopic polyangiitis is a necrotising pauci‐immune vasculitis affecting predominantly small vessels and often associated with a high titre of myeloperoxidase antineutrophil cytoplasmic antibodies (MPO)‐ANCA or positive perinuclear‐ANCA (p‐ANCA) staining. Necrotising glomerulonephritis is very common.9 Pulmonary capillaritis often occurs, in the absence of granulomatous lesions of the respiratory tract. The only modification of the Chapel Hill report is that ANCA was added to the description of microscopic polyangiitis. No formal classification criteria were proposed beyond this definition of a clinical syndrome.
Wegener's granulomatosis
The ACR criteria require the presence of two of the following four features for classification as WG: nasal‐oral inflammation, abnormal chest x ray, abnormal urinalysis, and granulomatous inflammation on biopsy.13 Based on the frequency of clinical findings in children and the availability of improved technology, modifications were made to these criteria. The presence of subglottic, tracheal, or endobronchial stenosis, and the presence of a high titre of proteinase 3 (PR3)‐ANCA or positive cytoplasmic ANCA (c‐ANCA) staining were added as new criteria (table 6). Slight modifications were made in two of the existing items for similar reasons. Classification of a child as having WG requires the presence of three of the newly defined set of six criteria (table 6).
Table 6 Classification criteria for Wegener's granulomatosis.
| Three of the following six features should be present: |
| • Abnormal urinalysis* |
| • Granulomatous inflammation on biopsy† |
| • Nasal sinus inflammation |
| • Subglottic, tracheal, or endobronchial stenosis |
| • Abnormal chest x ray or CT |
| • PR3 ANCA or C‐ANCA staining |
*Haematuria and/or significant proteinuria.
†If a kidney biopsy is done it characteristically shows necrotising pauci‐immune glomerulonephritis.
ANCA, antineutrophil cytoplasmic antibodies.
Takayasu arteritis
The classification of TA by the ACR criteria requires fulfilment of three of six criteria: age less than 40 years, claudication of the extremities, decreased brachial pulse, blood pressure difference >10 mm Hg, bruit over subclavian arteries or aorta, and arteriographic abnormalities.12 In the revised criteria, “angiographic abnormalities” was made a mandatory criterion, although details of the abnormalities remain to be determined (table 7). The angiographic technique can be conventional angiography, angiography guided by computed tomography, or magnetic resonance angiography (MRA). The presence of decreased peripheral artery pulses or claudication of the extremities or both was incorporated into a single criterion. Hypertension (age appropriate) was included as a criterion as it may be the sole presenting symptom in children (table 7). The age criterion was deleted. Thus the classification of a child as having TA requires the presence of angiographic abnormalities plus the presence of one or more of the four newly defined set of criteria (table 7).
Table 7 Classification criteria for Takayasu arteritis.
| Angiographic abnormalities (conventional, CT, or MR) of the aorta or its main branches (mandatory criterion), plus at least one of the following four features: |
| • Decreased peripheral artery pulse(s) and/or claudication of extremities |
| • Blood pressure difference >10 mm Hg |
| • Bruits over aorta and/or its major branches |
| • Hypertension (related to childhood normative data) |
CT, computed tomography; MR, magnetic resonance.
Discussion
The aim of this project was to develop classification criteria applicable to childhood vasculitides. This was achieved using Delphi and NGT consensus formation techniques, resulting in the first internationally agreed classification of vasculitis in childhood. The utilisation of NGT has many advantages. It offers more focused discussion compared with traditional (free for all) meetings, and generates a greater flow of ideas.3,4 It also allows equal participation of the participants. This was important in relation to the consensus conference because there were different subspecialties involved in addition to different nationalities.
The aim of developing a working classification for childhood and of individual vasculitides of childhood required a definition of “childhood” as well. The latter has hitherto been arbitrary and varies across the world.20 When talking about childhood we propose that we should concur with the UN/Unicef definition of childhood as 18 years and under.
Participating paediatricians agreed that there was a need for revision of the existing criteria in the light of current practice. It is hoped that the international character of the consensus conference will enable these criteria to meet the needs of paediatricians across the world. We approached the problem by addressing the clinical utility of each criterion. New criteria were introduced when they were considered to be important and frequent in childhood disease. Some criteria in existing disease definitions were modified in view of advances in technology such as the CT or MR, or to make them appropriate for the paediatric age range. Another major change was the inclusion of mandatory criteria for four diseases in order to increase the specificity of the criteria. Finally, some criteria were deleted (for example, patient age, as all patients to whom that criterion would apply would be children).
Comments specific to the general classification of childhood vasculitic diseases
It was agreed that vessel size, as in the Chapel Hill format, would form the backbone of the criteria. Various changes were introduced. We used the term “predominantly” in reference to vessel size, in acknowledgement of the overlap of size of affected vessels in some patients.19 The classification does not include diseases not encountered in childhood such as temporal arteritis, and includes various diseases not addressed by the classifications of vasculitis in adults. Small vessel vasculitis was subdivided according to the presence of granulomas as this feature has important distinguishing implications. Finally a category of “other vasculitides” was included for those vasculitides in which an aetiological process was defined, or in which no other classification category was appropriate.
Comments specific to Henoch‐Schönlein purpura
The major change in the criteria was to make palpable purpura a mandatory criterion, as it has been shown to improve the specificity of the criteria significantly when tested in an international study of patients with PAN.2 The characteristic biopsy findings were clarified. As IgA deposition is highly characteristic of HSP, the criterion requires the predominance of IgA in the renal or skin biopsy. As IgA tissue deposition can occur in several other diseases, it seemed important to define IgA deposits as being predominant.
As arthritis is common in childhood HSP, it was included as a criterion.
Comments specific to Kawasaki disease
The features of the existing criteria were accepted in both questionnaire surveys and at the consensus conference.
Because of the importance of coronary artery disease, as pointed out in the fifth revised edition of the Japan Kawasaki disease research committee guidelines18 and the American Heart Association (AHA) diagnostic guidelines,19 children with typical echocardiographic changes could be classified as having KD without fulfilling four of the remaining criteria, although the number of criteria remains to be determined.
The desquamation frequently seen in the perineum was included with the changes in extremities as a modified criterion. On the other hand irritability, which was suggested as a new criterion in the first survey, was not accepted by the consensus group as it was too non‐specific. There are very rare patients without fever and one should bear this in mind.
Comments specific to polyarteritis nodosa
Paediatric data during the last 10 years have shown that PAN in children is hard to classify using the definitions applicable to adults.21 In childhood disease streptococcal infections are frequently implicated in the aetiology. Paediatricians often base their diagnosis on abnormal angiography or on a biopsy showing necrotising small or medium size arteritis.16,19 The latter is also part of the definition recommended by the Chapel Hill consensus conference.9 We decided that abnormal angiography or a characteristic biopsy are mandatory criteria for the diagnosis of the disease.
Another revision was the removal of the evidence for hepatitis B surface antigen as it was felt that this was not a major feature in paediatrics, thanks to the improving vaccination protocols.
The recent paediatric PAN registry has shown that cutaneous disease is quite common in childhood; thus a definition for this entity was introduced.19 Microscopic polyangiitis was also defined by the group, and a positive MPO‐ANCA criterion was added to the Chapel Hill report as this was the collective experience of the experts around the table.
Comments specific to Wegener's granulomatosis
Subglottic, tracheal, or endobronchial stenosis was added as a new criterion as these features were noted to be frequent in childhood disease.22 WG is a disease where improving technology has affected clinical practice. Computed tomography is almost always a part of investigation, which no longer relies on a plain chest radiography. Thus definitions of WG based on radiological imaging have been updated in the new criteria.
ANCA testing was not included in the ACR criteria, and in the Chapel Hill criteria the presence of ANCA in WG was referred to but not included in the definition. Both the respondents of the questionnaire surveys and the consensus group strongly felt that this feature should be included in the final set of criteria. The need to fulfil three criteria reflected the experience of the participants.
Comments specific to Takayasu arteritis
The angiographic definition was updated according to current clinical practice and was a required criterion for classification. Although hypertension is non‐specific, it was noted to be common and often the only presenting sign.23 Therefore hypertension was included as a new criterion.
Conclusions
A consensus was reached for a new international classification of childhood vasculitis. We believe this was an important task as appropriate classification criteria for vasculitis in children have been missing for far too long. It is hoped that the international and multispecialist composition of the expert group involved will facilitate the applicability of this classification for most vasculitic diseases in children seen around the world. The next step will be to validate these criteria using patients and control groups.
Acknowledgements
We would like to thank all our colleagues who have kindly provided their input by answering the initial survey.
Abbreviations
ACR - American College of Rheumatology
ANCA - antineutrophil cytoplasmic antibodies
ESPN - European Society of Paediatric Nephrology
EULAR - European League against Rheumatism
HSP - Henoch‐Schönlein purpura
KD - Kawasaki disease
NGT - nominal group techniques
PAN - polyarteritis nodosa
PReS - Paediatric Rheumatology European Society
TA - Takayasu arteritis
WG - Wegener's granulomatosis
References
- 1.Dillon M. Primary vasculitis in children. In: Maddison PJ, Isenberg DA, Woo P, Glass DN, editors. Oxford textbook of rheumatology. Oxford: Oxford University Press, 19981402–1412.
- 2.Ozen S, Anton J, Arisoy N.et al Juvenile polyarteritis: results of a multicenter survey of 110 children. J Pediatr 2004145517–522. [DOI] [PubMed] [Google Scholar]
- 3.Sniderman A D. Clinical trials, consensus conferences, and clinical practice. Lancet 1999354(9175)327–330. [DOI] [PubMed] [Google Scholar]
- 4.Delbecq A L, Van de Ven A H, Gustafson D H.Group techniques for program planning. A guide to nominal group and Delphi processes. Glenview, Illinois: Scott, Foresman, 1975
- 5.Giannini E H, Ruperto N, Ravelli A, Lovell D J, Felson D T, Martini A. Preliminary definition of improvement in juvenile arthritis. Arthritis Rheum 1997401202–1209. [DOI] [PubMed] [Google Scholar]
- 6.Ruperto N, Ravelli A, Murray K J, Lovell D J, Andersson‐Gare B, Feldman B M.et al Preliminary core sets of measures for disease activity and damage assessment in juvenile systemic lupus erythematosus and juvenile dermatomyositis. Rheumatology (Oxford) 2003421452–1459. [DOI] [PubMed] [Google Scholar]
- 7.Felson D T, Anderson J J, Boers M, Bombardier C, Furst D, Goldsmith C.et al American College of Rheumatology preliminary definition of improvement in rheumatoid arthritis. Arthritis Rheum 199538727–735. [DOI] [PubMed] [Google Scholar]
- 8.Smolen J S, Strand V, Cardiel M, Edworthy S, Furst D, Gladman D.et al Randomized clinical trials and longitudinal observational studies in systemic lupus erythematosus: consensus on a preliminary core set of outcome domains. J Rheumatol 199926504–507. [PubMed] [Google Scholar]
- 9.Jennette J C, Falk R J, Andrassy K, Bacon P A, Churg J, Gross W L.et al Nomenclature of systemic vasculitides. Proposal of an international consensus conference. Arthritis Rheum 199437187–192. [DOI] [PubMed] [Google Scholar]
- 10.Lie J T. Nomenclature and classification of vasculitis: plus ca change, plus c'est la meme chose. Arthritis Rheum 199437181–186. [DOI] [PubMed] [Google Scholar]
- 11.Mills J A, Michel B A, Bloch D A, Calabrese L H, Hunder G G, Arend W P.et al The American College of Rheumatology 1990 criteria for the classification of Henoch‐Schönlein purpura. Arthritis Rheum 1990331114–1121. [DOI] [PubMed] [Google Scholar]
- 12.Arend W P, Michel B A, Bloch D A, Hunder G G, Calabrese L H, Edworthy S M.et al The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum 1990331129–1134. [DOI] [PubMed] [Google Scholar]
- 13.Leavitt R Y, Fauci A S, Bloch D A, Michel B A, Hunder G G, Arend W P.et al The American College of Rheumatology 1990 criteria for the classification of Wegener's granulomatosis. Arthritis Rheum 1990331101–1107. [DOI] [PubMed] [Google Scholar]
- 14.Lightfoot R W, Michel B A, Bloch D A, Hunder G G, Zvaifler N J, McShane D J.et al The American College of Rheumatology 1990 criteria for the classification of polyarteritis nodosa. Arthritis Rheum 1990331088–1093. [DOI] [PubMed] [Google Scholar]
- 15.Kawasaki T. Acute febrile mucocutaneous lymph node syndrome with lymphoid involvement with specific desquamation of the fingers and the toes. Jpn J Allergy 196716178–222. [PubMed] [Google Scholar]
- 16.Brogan P A, Davies R, Gordon I, Dillon M J. Renal angiography in children with PAN. Pediatr Nephrol 200217277–283. [DOI] [PubMed] [Google Scholar]
- 17.Ozen S, Besbas N, Saatci U, Bakkaloglu A. Diagnostic criteria for polyarteritis nodosa in childhood. J Pediatr 19922206–209. [DOI] [PubMed] [Google Scholar]
- 18.Japan Kawasaki Disease Research Committee Diagnostic guidelines for Kawasaki disease, fifth edition, Tokyo 2002
- 19.Newburger J W, Takahashi M, Gerber M A, Gewitz M H, Tani L Y, Burns J C.et al Diagnosis, treatment, and long‐term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics 20041141708–1733. [DOI] [PubMed] [Google Scholar]
- 20.Pediatrics Council on Child and Adolescent Health Age limits of pediatrics. Pediatrics 198881736. [PubMed] [Google Scholar]
- 21.Ozen S. Vasculitis in children. In: Isenberg DA, Maddison PJ, Woo P, Glass DN, Breedveld FC, editors. Oxford textbook of rheumatology. Oxford: Oxford University Press, 2004993–998.
- 22.Belostotsky V M, Shah V, Dillon M J. Clinical features in 17 paediatric patients with Wegener granulomatosis. Pediatr Nephrol 200217754–761. [DOI] [PubMed] [Google Scholar]
- 23.Jain S, Sharma N, Singh S, Bali H K, Kumar L, Sharma B K. Takayasu arteritis in children and young Indians. Int J Cardiol 200075(suppl 1)S153–S157. [DOI] [PubMed] [Google Scholar]