Abstract
Objective
To investigate the relative impact of radiographic osteoarthritis (ROA) and current knee pain on lower limb physical function, quadriceps strength, knee joint proprioception, and postural sway.
Methods
Using a 2×2 factorial design, 142 community derived subjects aged over 45 were divided into four subgroups based on the presence or absence of ROA (Kellgren & Lawrence >grade 2) and knee pain (as assessed by NHANES questions and a 100 mm visual analogue scale). Maximum isometric contraction of the quadriceps, knee joint proprioceptive acuity, static postural sway, and WOMAC index (both whole and function subscale) were assessed in all subjects.
Results
Compared with normal subjects, reported disability was greater for all other subgroups (p<0.01). Subjects with both ROA and knee pain reported the greatest disability, and those with knee pain only had greater disability than those with ROA only. Quadriceps weakness was observed in all groups compared with normal subjects (p<0.01), though they were no significant intergroup differences. Subjects with knee pain had a greater sway area than those without (p<0.05) but the presence of ROA was not associated with increased postural sway. No differences in proprioceptive acuity were observed between groups.
Conclusions
The presence of knee pain has a negative association with quadriceps strength, postural sway, and disability compared with ROA. However, the presence of pain‐free ROA has a significant negative influence on relative quadriceps strength and reported disability.
Keywords: knee pain, osteoarthritis, quadriceps strength, proprioception, postural sway
The risk of disability associated with knee osteoarthritis in those aged over 65 is reportedly greater than any other medical condition affecting the elderly.1 Over 30% of people over 65 years of age have radiographic knee osteoarthritis (ROA) and 25% of people experience knee pain.2 However, there is only a modest correlation between these features.2 Although the presence of ROA is associated with impaired physical function, the association with knee pain is significantly stronger.3,4,5 The odds of disability are doubled in those with knee pain compared with those with ROA alone, and the additional presence of ROA in those with knee pain does not increase this risk.3
Quadriceps strength is strongly associated with lower limb function in the elderly, and the established decline in strength of normal aging people is compounded by the presence of osteoarthritis.4,6,7 Quadriceps weakness has been demonstrated in subjects with ROA and or knee pain but is greater in those with both.8 Pain, intracapsular swelling, and structural remodelling have been cited as contributing factors.8,9
Knee joint proprioception is important in the activation of reflex responses which protect and stabilise the knee.10 Proprioceptive acuity diminishes with increasing age,9,11 and is further reduced in those with symptomatic knee osteoarthritis.12,13 Moderate but significant correlations have been reported between impaired knee proprioception and decreased function,9,11 but other studies have failed to confirm this relation.14
Control of balance requires integration of the visual, vestibular, somatosensory, and neuromuscular systems.15 Postural sway, the periodic translation of the body's centre of pressure used to maintain upright balance, has been shown to increase with age.7,9,16 Further increases in postural sway have been observed in subjects with knee osteoarthritis 12,17,18 and a relation with quadriceps weakness and increased disability shown.12 Inconsistent associations with pain and radiographic severity have been reported.12,18,19,20
While the association of ROA and knee pain with disability have been reported, the individual contributions of pain and ROA on quadriceps strength, proprioception, postural sway, and function have yet to be examined rigorously in a single population. We therefore undertook the following study to determine the relative impact of ROA and knee pain on quadriceps strength, proprioception, postural sway, and function by measuring these functions in individuals with ROA and knee pain using a factorial design.
Methods
Subjects
A 2×2 factorial design was used, with subjects derived from a postal survey concerned with knee pain. This survey, which has been described elsewhere,21 was conducted on 4057 men and women aged 47 to 70 registered at several large general practices in Nottingham. Postal invitations were sent to 409 subjects, which yielded a 44% response rate. These subjects were screened and allocated to one of four subgroups based on the presence or absence of knee pain and ROA. Subjects were excluded if they had rheumatoid arthritis, any lower limb joint replacements, lower limb amputations, severe cardiac conditions, or any neurological, visual, or vestibular condition that overtly impaired their balance. Sex, body mass index, drug use, and comorbidity were documented but did not form part of the eligibility criteria.
The study was approved by the local ethics committee (EC00/06) and signed consent was obtained from all participants.
Radiographic status
Standardised anteroposterior extended weight bearing radiographs and skyline views (30° knee flexion) of both knees (obtained within the previous five years) were graded by a single reader using the Kellgren and Lawrence system and an atlas of standardised radiographs.22 ROA was defined as the presence of definite osteophytes and definite joint space narrowing (greater than Kellgren and Lawrence grade 2). Knees were considered normal if osteophytes and joint space narrowing were absent or if only possible osteophytes were observed (that is, less than Kellgren and Lawrence grade 2). Subjects with Kellgren and Lawrence grade 2 were excluded from the analysis.
Pain status
Knee pain was determined using two questions from the National Health and Nutrition Examinations Survey (NHANES),23 which ask “Have you ever had pain in or around your knees on most days for at least a month?” If so “Have you experienced any knee pain during the last year?” Only subjects answering yes to both parts were considered pain positive. They then scored their current knee pain on a 100 mm visual analogue scale (VAS) where 0 = no pain and 100 = worse pain ever. Scores less than 20 and greater than 80 mm on the VAS were excluded from the analysis.
Physical function
Measures of physical function were assessed by one investigator who was blinded to the x ray and pain status of the subjects. All tests were carried out on a single limb. The most affected knee by radiographic assessment or most symptomatic (in the case of painful knees) was assigned by an independent observer. Where these differed, the most symptomatic knee was assessed and for those with normal knees a random limb was chosen. The order in which the tests were carried out was block randomised.
Isometric quadriceps strength
Maximum voluntary contraction (MVC) was measured using a standard protocol.12 Subjects sat in a modified Tornvall chair with hips and knees flexed to 90° and pelvis secured. A non‐extendable strap attached around the test ankle was connected to a load cell (TKA‐100A), horizontal and perpendicular to the ankle. This was connected to an amplifier and digital display unit that showed the force generated (in Newtons) during isometric knee extension. Subjects were asked to push as hard as possible against the ankle strap until a peak value was obtained on the digital display unit. A 30 second rest period was allowed between each attempt and the mean of three MVCs was calculated for each subject.
Proprioceptive acuity
Proprioceptive acuity was measured using an active repositioning test in a modified Tornvall chair previously described.12 From a resting knee joint position of 90° flexion, the subject's knee was passively moved to a random angle (the criterion angle) between 20° and 50° of knee flexion out of vision of the patient. The knee was held at the criterion angle for five seconds before being returned to its resting position. The subject was asked to actively reposition their knee at the criterion angle. The accuracy to which this was achieved was recorded for three different criterion angles and the mean value calculated.
Postural sway
Postural sway was measured using the balance performance monitor (BPM) previously described by our group.12 Subjects were asked to stand as still as possible on two footplates for a period of 30 seconds for three tests under two conditions: eyes open and eyes closed. A 30 second rest period was allowed between each attempt. Postural sway was recorded at a rate of 10 Hz and the BPM produced a range of variables related to the movement of the subject's centre of pressure. These included the following:
sway path (the distance travelled by the subject's centre of pressure in mm);
sway area (the area of an ellipse encompassing the swat path in mm2);
lateral sway coefficient (an arbitrary value which denotes the standard deviation of weight shift around the subject's mean weight distribution).
The means for each sway variable was calculated for each condition.
Self reported function
Function was assessed using the self administered Western Ontario and MacMaster Universities osteoarthritis index (WOMAC).24 All sections of the index were completed.
Statistical analysis
Power calculations were based on a previous study of knee joint proprioception.12 Power was set at 0.8 and the level of statistical significance at p<0.05. Statistical analysis was carried out using SPSS v11. All tests were two tailed. Differences between the four subgroups were analysed using analysis of variance and the post‐hoc Scheffé test for normally distributed data and the Kruskal–Wallis and Mann–Whitney U tests for non‐normally distributed data. Ordinal data produced by the WOMAC index were subjected to both parametric and non‐parametric analysis, as recommended.25
Results
In all, 181 subjects between the ages of 50 and 82 were recruited to the study. Thirty nine were excluded, 12 because of coexisting conditions, 15 because of incomplete data, four because their current knee pain scores fell below 20 mm on the VAS, and a further eight because their x ray scores equalled Kellgren and Lawrence grade 2. A total of 142 subjects was included in the final analysis.
Table 1 shows the anthropometric data for each subgroup. There were more women than men in each subgroup, but this difference was significant only for the normal subgroup (p<0.01). No differences existed between subgroups for age or height. Subjects with both pain and ROA were significantly heavier and had a greater body mass index (BMI) than normal subjects (p<0.01). Subjects with pain without ROA also had a greater BMI than the normal subjects (p = 0.05).
Table 1 Anthropometric data of each subgroup.
| ROA−, KP− | ROA+, KP− | ROA−, KP+ | ROA+, KP+ | |
|---|---|---|---|---|
| Male | 17 | 7 | 9 | 14 |
| Female | 38 | 16 | 19 | 22 |
| Total | 55 | 23 | 28 | 36 |
| Age (years) | 67.49 (8.45) | 69.22 (5.78) | 67.36 (6.46) | 68.78 (7.80) |
| Height (m) | 1.65 (0.09) | 1.64 (0.11) | 1.67(0.09) | 1.65 (0.09) |
| Weight (kg) | 70.42 (12.79) | 76.78 (15.66) | 74.66(13.82) | 80.44 (12.16) |
| BMI (kg/m2) | 25.89 (3.97) | 28.45 (4.69) | 26.70 (3.93) | 29.72 (4.40) |
Values are n or mean (SD).
BMI, body mass index; KP+, knee pain positive; KP−, knee pain negative; ROA+, radiographic osteoarthritis positive; ROA−, radiographic osteoarthritis negative.
Table 2 presents the results for the physical function tests and self reported WOMAC scores.
Table 2 Descriptive data for measures of physical function and self reported function.
| Variable | Unit | ROA−, KP− | ROA+, KP− | ROA−, KP+ | ROA+, KP+ |
|---|---|---|---|---|---|
| Quadriceps strength | N | 26.58 (9.62) | 22.19 (7.03) | 20.67 (8.74) | 19.47 (7.57) |
| Quadriceps strength: weight | N/kg | 0.38 (0.10) | 0.29 (0.08) | 0.28 (0.11) | 0.24 (0.08) |
| Proprioceptive acuity | degrees | 5.10 (3.02) | 5.06 (2.84) | 6.52 (4.00) | 5.84 (3.20) |
| Sway area (eyes open) | mm2 | 305.21 (279.64) | 332.12 (278.96) | 553.73 (592.18) | 632.44 (1043.18) |
| Sway path (eyes open) | mm | 347.05 (113.46) | 357.58 (135.55) | 366.06 (103.89) | 402.28 (149.21) |
| Lateral sway coefficient (eyes open) | 2.62 (1.42) | 2.65 (1.88) | 3.27 (2.05) | 3.36 (2.05) | |
| WOMAC scores | |||||
| Overall (0–96) | 4 (4 to 7.3) | 12 (4 to 18) | 29.5 (21 to 41.75) | 40 (34 to 54) | |
| Subscales: | |||||
| Pain (0–20) | 0 (0 to 1) | 1 (0 to 2) | 6 (4.0 to 8.8) | 8 (5.0 to 10.8) | |
| Stiffness (0–8) | 0 (0) | 1 (0 to 2) | 4 (2.0 to 4.0) | 4 (3.0 to 4.0) | |
| Function (0–68) | 4 (4 to 6) | 8 (4 to 16) | 18 (13.0 to 29.4) | 30 (24.0 to 30.0) |
Values are mean (SD) or median (interquartile range).
KP+, knee pain positive; KP−, knee pain negative; ROA+, radiographic osteoarthritis positive; ROA−, radiographic osteoarthritis negative; WOMAC, Western Ontario and MacMaster Universities osteoarthritis index.
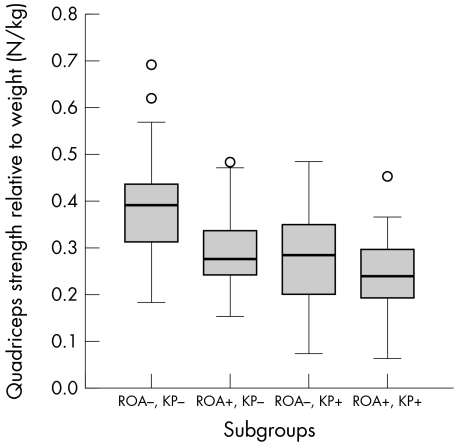
Quadriceps strength
Quadriceps strength was measured in Newtons and expressed as a ratio relative to body weight (N/kg). Reduced strength was observed in all subgroups compared with the normal subjects (p<0.01), but there were no significant differences between the subgroups (fig 1).
Figure 1 Box plot of quadriceps strength relative to weight (N/kg) for each subgroup. KP+, knee pain positive; KP−, knee pain negative; ROA+, radiographic osteoarthritis positive; ROA−, radiographic osteoarthritis negative. Empty circles indicate minor outliers.
Proprioceptive acuity
A wide range of proprioceptive acuity scores was observed (0.67 to 17.33) but no differences were found between groups. A trend was observed where subjects with knee pain (regardless of the presence of ROA) had poorer proprioceptive acuity than subjects without knee pain, at (mean (SD)) 6.14 (3.55)° v 5.09 (2.95)°, but this did not reach statistical significance (t = 1.92, p = 0.057).
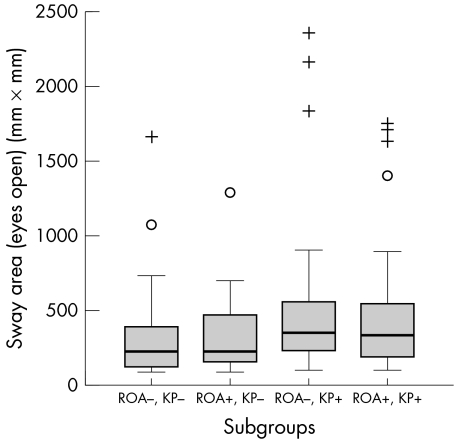
Postural sway
Increased sway area was demonstrated in subjects with painful ROA (p = 0.02) and those with pain without ROA (p<0.01) compared with normal subjects (fig 2). Subjects with ROA without pain did not differ from normal subjects.
Figure 2 Box plots showing sway area (eyes open) for each subgroup. KP+, knee pain positive; KP−, knee pain negative; ROA+, radiographic osteoarthritis positive; ROA−, radiographic osteoarthritis negative. Empty circles indicate minor outliers; crosses indicate extreme outliers.
When subjects were analysed with respect to pain only (regardless of ROA), those with pain were found to have increased postural sway for several variables: sway area with eyes open (z = −3.09, p<0.01) sway path with eyes open (z = −2.02, p<0.05), and lateral sway coefficient with eyes open (z = −2.06, p<0.05). No differences were found between subjects with and without ROA (regardless of knee pain). Adjusting for quadriceps strength and age did not affect the results.
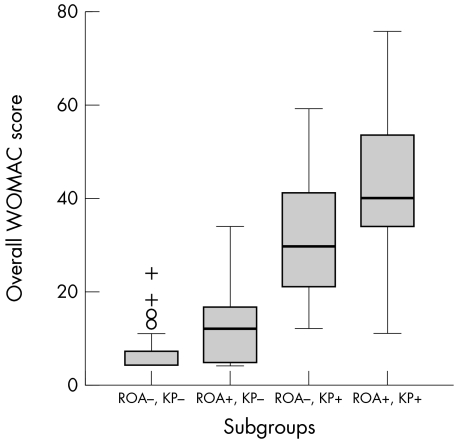
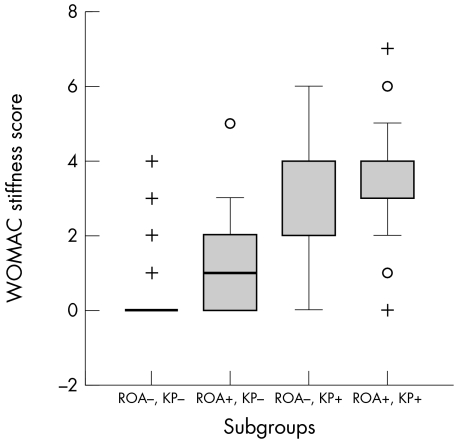
WOMAC scores
Normal subjects reported less disability (entire index score and function subscale) than other subgroups (p<0.01), and all differences between subgroups were significant (p<0.01) (fig 3). Significant differences in scores for reported knee joint stiffness were also observed between normal subjects and all other subgroups (p<0.001) (fig 4).
Figure 3 Box plots showing overall WOMAC scores for each subgroup. KP+, knee pain positive; KP−, knee pain negative; ROA+, radiographic osteoarthritis positive; ROA−, radiographic osteoarthritis negative; WOMAC, Western Ontario and MacMaster Universities osteoarthritis index. Empty circles represent minor outliers; crosses represent extreme outliers.
Figure 4 Box plots showing WOMAC stiffness scores for each subgroup. KP+, knee pain positive; KP−, knee pain negative; ROA+, radiographic osteoarthritis positive; ROA−, radiographic osteoarthritis negative; WOMAC, Western Ontario and MacMaster Universities osteoarthritis index. Empty circles represent minor outliers; crosses represent extreme outliers.
Discussion
Summary of findings
Subjects with knee pain had weaker quadriceps strength, greater postural sway, and greater self reported disability than subjects with ROA. Subjects with ROA had weaker quadriceps strength and greater disability than normal subjects, but postural sway was not found to differ. Proprioceptive acuity did not differ between any of the groups.
Evaluation of methodology and population studied
The radiographic definition of knee osteoarthritis used for this study was set to include the presence of definite osteophytes and definite joint space narrowing. Intraobserver reliability for scoring radiographs was high (κ >0.7). Radiographs for the study were obtained between 1997 and 2001. Consequently, five years may have elapsed between radiographs being obtained and participation in the study. The incidence of new knee ROA in the over‐60s has been estimated at less than 2%,26 and therefore two subjects with previously pain‐free normal knees may have developed new ROA.
Knee pain was determined by questions taken from the NHANES study.23 It has been noted previously that the wording of the questions does not require the presence of current knee pain,21 and therefore subjects were also required to score their current knee pain on a 100 mm VAS. Scores below 20 mm and greater than 80 mm were excluded to minimise the influence of pain severity. When analysed, the results were not affected by pain severity.
Reproducibility for measures of quadriceps strength, proprioceptive acuity, and postural sway have been reported previously by our group as good.12
This was a community derived sample. The age of the population was normally distributed, with no difference between the four subgroups. Subjects with knee pain and ROA, and knee pain without ROA, had a significantly greater BMI than normal subjects. Increased weight and obesity are both recognised risk factors for the development of knee osteoarthritis and knee pain,27,28,29 though the mean BMI for each subgroup did not fall within the obese range.30
The findings of the study
Our study confirms previous findings that individuals with both ROA and knee pain experience greater disability than those with either ROA or pain alone, and that the presence of pain has a stronger association than radiological change.3,4,31 However, the disability experienced by subjects with ROA without pain was also significantly greater than in those with normal knees (p = 0.01).
Reduced quadriceps strength has been widely demonstrated in the presence of ROA and knee pain.7,9,12 This study confirms that individuals with pain or ROA or both are weaker than normal subjects (p<0.01). However, there were no significant differences between these subgroups. It is known that measurement of MVC does not account for variation in muscle activation resulting from pain, joint effusion, arthrogenic muscle inhibition, or motivational factors which reportedly reduce activation, and in turn the force generated, by as much as 60%.32 It has also been suggested that deterioration of quadriceps strength may reach a critical threshold below which function is compromised.4 Subjects participating in this study were living independently in the community and it is therefore unlikely that their quadriceps strength would have decreased beyond a level where functional daily activities became impossible.
Diminished proprioceptive acuity has been observed in patients with painful ROA.11,12,33 However, our results did not reveal any difference between the four subgroups. This was somewhat surprising but could be attributed to various factors. Knee joint swelling is a possible confounding variable. The effects of acute joint swelling on joint proprioception have been inconclusive and no acute effusions were noted among the participant in the study. However, it has been proposed that chronic effusion may influence proprioception by either the inflammatory constituents of the fluid or the effects on capsular compliance.34 It is possible that some subjects may have had chronic intracapsular swelling. Knee joint swelling has also been shown to have an inhibitory effect on the motor neurone activity in the quadriceps, which may have affected the active repositioning of the limb.35 It has also been suggested that diminished proprioception may precede structural changes,13,36 which could counteract the group effects of subjects without ROA. As with quadriceps strength, it is also possible that the decline in proprioceptive acuity reaches a threshold that preserves function and beyond which the decline does not progress. It was noted that the mean values for proprioceptive acuity for each group in this study were greater than those reported in other studies that used the same method for testing joint position sense,20,31 but were less than those used to determine the power of the study.12
Subjects with knee osteoarthritis have shown greater postural sway, than controls, denoting poorer balance.12,18,31 In this study, subjects with knee pain (both with and without ROA) had a significantly greater sway area (eyes open) compared with normal subjects. When all subjects with knee pain were compared with pain‐free subjects, they were found to have greater sway in the various ways tested. No differences were found between subjects with and without ROA, which may suggest that the presence of knee osteoarthritis has little bearing on postural sway, or that individuals are better able to compensate for aberrations in sway caused by ROA than caused by pain. A correlation between pain intensity and postural sway has been reported but was not observed in this study.18,19 All groups showed greater postural sway with their eyes shut, but performance with eyes open was more discriminatory between groups. There were no particular variables that consistently demonstrated differences between groups.
Implications of the findings
Although each subgroup showed differences in terms of function, there was wide variability within the four groups, confirming the heterogeneity of knee osteoarthritis and knee pain. Those with knee pain showed increased postural sway, reduced quadriceps strength, proprioceptive acuity, and physical function compared with those with ROA. However, those with ROA were also weaker and reported poorer function than normal subjects. This does not infer causality, and there are other factors that may have contributed to the results.
Statistically it has been shown that people with ROA but without knee pain are different from those with normal pain‐free knees. They have a significantly greater BMI, weaker quadriceps strength, and report greater stiffness and disability than normal subjects. It is not yet clear whether this difference in reported disability is clinically important. A recent report estimated that a WOMAC function subscale score of 31/100 was a baseline value of function that patients consider acceptable.36 If this were applied to our study population then the disability reported by this group would not be clinically significant. However, this group is relatively unstudied as a population and our study has highlighted the need for further prospective investigation to determine the factors associated with the development of knee pain and increased disability.
Future work
The association of structural change and knee pain with joint stiffness provided an interesting adjunct to this study. Differences in reported knee stiffness as determined by the WOMAC index were found between those with normal knees and all other groups. Those with knee pain reported greater joint stiffness than those with ROA, but both were statistically significant (though it is uncertain whether this difference is clinically relevant). It is beyond the scope of this paper to speculate on the possible mechanisms but it would appear that anatomical remodelling is not the only factor involved. Knee stiffness as a clinical symptom has been relatively ignored but it has been shown to double the odds for locomotor disability compared with structural changes,3 and the preliminary findings in this study warrant further exploration.
Acknowledgements
We would like to thank Margaret Ball, Eleanor Berrill, Sally Doherty, Joanna Ramowski, and Margaret Wheeler from the Division of Academic Rheumatology and the Division of Physiotherapy Education for their assistance with this project.
Abbreviations
BPM - balance performance monitor
MVC - maximum voluntary contraction
NHANES - National Health and Nutrition Examinations Survey
ROA - radiographic osteoarthritis
VAS - visual analogue scale
WOMAC - Western Ontario and MacMaster Universities osteoarthritis index
References
- 1.Guccione A A, Felston D T, Anderson J J, Anthony J M, Zhang Y, Wilson P W.et al The effects of specific medical conditions on the functional limitations of elders in the Framingham study. Am J Public Health 199484351–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Felson D T, Naimark A, Anderson J, Kazis L, Castelli W, Meenan R F. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum 198730914–918. [DOI] [PubMed] [Google Scholar]
- 3.Odding E, Valkenburg H A, Algra D, Vandenouweland F A, Grobbee D E, Hofman A. Associations of radiological osteoarthritis of the hip and knee with locomotor disability in the Rotterdam study. Ann Rheum Dis 199857203–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McAlindon T E, Cooper C, Kirwan J R, Dieppe P A. Determinants of disability in osteoarthritis of the knee. Ann Rheum Dis 199352258–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davis M A, Ettinger W H, Neuhaus J M, Mallon K P. Knee osteoarthritis and physical functioning: evidence from the NHANES I Epidemiologic Followup Study. J Rheumatol 199118591–598. [PubMed] [Google Scholar]
- 6.Hyatt R H, Whitelaw M N, Bhat A, Scott S, Maxwell J D. Association of muscle strength with functional status of elderly people. Age Ageing 199019330–336. [DOI] [PubMed] [Google Scholar]
- 7.Messier S P, Glasser J L, Ettinger W H, Craven T E, Miller M E. Declines in strength and balance in older adults with chronic knee pain: a 30‐month longitudinal, observational study. Arthritis Rheum 200247141–148. [DOI] [PubMed] [Google Scholar]
- 8.Slemenda C, Brandt K D, Heilman D K, Mazzuca S, Braunstein E M, Katz B P.et al Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med 199712797–104. [DOI] [PubMed] [Google Scholar]
- 9.Hurley M V, Rees J, Newham D J. Quadriceps function, proprioceptive acuity and functional performance in healthy young, middle‐aged and elderly subjects. Age Ageing 19982755–62. [DOI] [PubMed] [Google Scholar]
- 10.Lattanzio P J, Petrella R J. Knee proprioception: a review of mechanisms, measurements, and implications of muscular fatigue. Orthopedics 199821463–470. [DOI] [PubMed] [Google Scholar]
- 11.Pai Y C, Rymer W Z, Chang R W, Sharma L. Effect of age and osteoarthritis on knee proprioception. Arthritis Rheum 1997402260–2265. [DOI] [PubMed] [Google Scholar]
- 12.Hassan B S, Mockett S, Doherty M. Static postural sway, proprioception, and maximal voluntary quadriceps contraction in patients with knee osteoarthritis and normal control subjects. Ann Rheum Dis 200160612–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharma L, Pai Y C, Holtkamp K, Rymer W Z. Is knee joint proprioception worse in the arthritic knee versus the unaffected knee in unilateral knee osteoarthritis? Arthritis Rheum 1997401518–1525. [DOI] [PubMed] [Google Scholar]
- 14.Bennell K L, Hinman R S, Metcalf B R, Crossley K M, Buchbinder R, Smith M.et al Relationship of knee joint proprioception to pain and disability in individuals with knee osteoarthritis. J Orthop Res 200321792–797. [DOI] [PubMed] [Google Scholar]
- 15.Pollock A S, Durward B R, Rowe P J, Paul J P. What is balance? Clin Rehabil 200014402–406. [DOI] [PubMed] [Google Scholar]
- 16.Lord S R, Ward J A. Age‐associated differences in sensori‐motor function and balance in community dwelling women. Age Ageing 199423452–460. [PubMed] [Google Scholar]
- 17.Wegener L, Kisner C, Nichols D. Static and dynamic balance responses in persons with bilateral knee osteoarthritis. J Orthop Sports Phys Ther 19972513–18. [DOI] [PubMed] [Google Scholar]
- 18.Hinman R S, Bennell K L, Metcalf B R, Crossley K M. Balance impairments in individuals with symptomatic knee osteoarthritis: a comparison with matched controls using clinical tests. Rheumatology 2002411388–1394. [DOI] [PubMed] [Google Scholar]
- 19.Jadelis K, Miller M E, Ettinger W H, Messier S P. Strength, balance, and the modifying effects of obesity and knee pain: results from the Observational Arthritis Study in Seniors (OASIS). J Am Geriatr Soc 200149884–891. [DOI] [PubMed] [Google Scholar]
- 20.Birmingham T B, Kramer J F, Kirkley A, Inglis J T, Spaulding S J, Vandervoort A A. Association among neuromuscular and anatomic measures for patients with knee osteoarthritis. Arch Phys Med Rehabil 2001821115–1118. [DOI] [PubMed] [Google Scholar]
- 21.O'Reilly S C, Muir K R, Doherty M. Screening for pain in knee osteoarthritis: which question? Ann Rheum Dis 199655931–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Altman R D, Hochberg M, Murphy W A, Wolfe F, Lequesne M. Atlas of individual radiographic features in osteoarthritis. Osteoarthritis Cartilage 19953(suppl A)3–70. [PubMed] [Google Scholar]
- 23.National Center for Health Statistics Basic data on arthritis of the knee, hip and sacroiliac joint in adult ages 27–74 years: United States 1971–1975. Hyattsville: National Center for Health Statistics, 1979, DHEW Publication No (PHS)70–1661 (Vital and Health Statistics, series 11; No 213) [PubMed]
- 24.Bellamy N, Buchanan W, Goldsmith C, Campbell J, Stitt L W. Validation study of WOMAC: a health status instrument for measuring clinically‐important patient‐relevant outcome following total hip or knee arthroplasty in osteoarthritis. J Orthop Rheumatol 1988195–108. [PubMed] [Google Scholar]
- 25.Bellamy N.WOMAC Osteoarthritis Index: a user's guide. London, Ontario: University of Western Ontario, 1995
- 26.Felson D T, Zhang Y, Hannan M T, Naimark A, Weissman B N, Aliabadi P.et al The incidence and natural history of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum 1995381500–1505. [DOI] [PubMed] [Google Scholar]
- 27.Hart D J, Doyle D V, Spector T D. Incidence and risk factors for radiographic knee osteoarthritis in middle‐aged women: the Chingford Study. Arthritis Rheum 19994217–24. [DOI] [PubMed] [Google Scholar]
- 28.Felson D T, Anderson J J, Naimark A, Walker A M, Meenan R F. Obesity and knee osteoarthritis. The Framingham Study. Ann Intern Med 198810918–24. [DOI] [PubMed] [Google Scholar]
- 29.Anderson J J, Felson D T. Factors associated with osteoarthritis of the knee in the first national Health and Nutrition Examination Survey (HANES I). Evidence for an association with overweight, race, and physical demands of work. Am J Epidemiol 1988128179–189. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organisation Obesity. Preventing and managing the global epidemic. Report of a WHO Consultation on Obesity. Geneva: WHO, 1998 [PubMed]
- 31.Hurley M V, Scott D L, Rees J, Newham D J. Sensorimotor changes and functional performance in patients with knee osteoarthritis. Ann Rheum Dis 199756641–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Young A. Current issues in arthrogenous inhibition. Ann Rheum Dis 199352829–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barrett D S, Cobb A G, Bentley G. Joint proprioception in normal, osteoarthritic and replaced knees. J Bone Joint Surg Br 19917353–56. [DOI] [PubMed] [Google Scholar]
- 34.Sharma L, Pai Y C. Impaired proprioception and osteoarthritis. Curr Opin Rheumatol 19979253–258. [DOI] [PubMed] [Google Scholar]
- 35.Hopkins J T, Ingersoll C D, Krause B A, Edwards J E, Cordova M L. Effect of knee joint effusion on quadriceps and soleus motoneuron pool excitability. Med Sci Sports Exerc 200133123–126. [DOI] [PubMed] [Google Scholar]
- 36.Tubach F, Ravaud P, Baron G, Falissard B, Logeart I, Bellamy N.et al Evaluation of clinically relevant states in patient reported outcomes in knee and hip osteoarthritis: the patient acceptable symptom state. Ann Rheum Dis 20056434–37. [DOI] [PMC free article] [PubMed] [Google Scholar]