Rheumatoid meningitis is a rare but lethal disorder that occurs in an elderly population with longstanding rheumatoid arthritis (RA).1 Although the majority of patients experience neurological symptoms, up to 26% of the patients were asymptomatic in a case series study as identified by necropsy.1 There is poor correlation between the severity of synovitis and neurological symptoms, which therefore imposes a challenge in the diagnosis of this condition.1 To date there are no established treatment regimens for rheumatoid meningitis, although most patients receive immunosuppressive agents. Although the anti‐tumour necrosis factor (TNF) agents have been proved to provide significant relief for the articular manifestations of RA, their effectiveness for rheumatoid meningitis has not been reported.2
A 58 year old woman with previous diagnoses of fibromyalgia and osteoarthritis was referred to the rheumatology clinic of the Massachusetts General Hospital (MGH) with worsening polyarthritis of both hands, wrists, knees, and ankles while receiving daily rofecoxib, 25 mg. Before the visit she had undergone extensive investigation for a 6 month history of progressive neurological symptoms, including severe headaches, emotional lability, left facial numbness, slurred speech, weakness and numbness of the extremities, frequent falls, and seizures. Brain magnetic resonance imaging (MRI) showed enhancement of the leptomeninges over the right cerebral convexity (figs 1A and C). Brain biopsy at the MGH showed chronic pachymeningitis and leptomeningitis exhibiting an ill‐defined granulomatous reaction with central necrosis and surrounding chronic active inflammation with numerous plasma cells, Russell bodies, and multinucleated giant cells (fig 2). Gram stain and cultures of the brain biopsy samples failed to show any organisms, nor were malignant cells identified.
Figure 1 Magnetic resonance images demonstrated abnormal gadolinium enhancement of the dura and leptomeninges, and hyperintense signal in the subarachnoid spaces before intravenous cyclophosphamide treatment (A, C). After 6 months of treatment with monthly intravenous cyclophosphamide and daily oral prednisone, almost complete resolution of these abnormal findings occurred (B, D). Coronal T1 weighted images after administration of intravenous gadolinium contrast (A, B), and axial FLAIR images (C, D). (R, right; L, left).
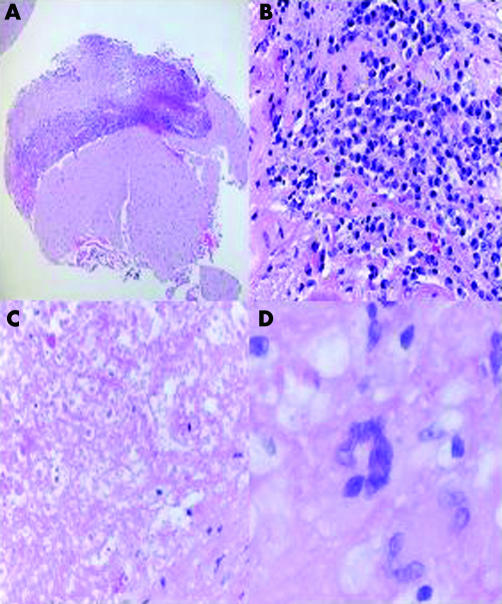
Figure 2 A biopsy of the dura and underlying brain showed thickening of the dura and leptomeninges with chronic inflammation (A). The inflammatory exudate consists of mature lymphocytes, plasma cells, and histiocytes (B) surrounding an area of bland necrosis with acellular debris (C). Occasional multinucleated cells are also present in the exudate (D). Haematoxylin and eosin stain. Original magnification (A) ×50; (B) ×400; (C) ×200; (D) ×600.
At the MGH rheumatology clinic, her musculoskeletal examination, MRI of the hands showing scattered erosions in the proximal carpal bones and distal radius, and laboratory findings (erythrocyte sedimentation rate 79 mm/1st h, C reactive protein 73.7 mg/l, rheumatoid factor 413 IU/ml, anti‐cyclic citrullinated protein antibody 12 U (normal <20 U)) were consistent with seropositive RA. After exclusion of other autoimmune processes a diagnosis of RA and rheumatoid meningitis was made.3
Treatment was started with monthly intravenous infusions of cyclophosphamide, 600 mg/m2 for 6 months, and daily oral prednisone, 40 mg for 2 weeks. Her prednisone was tapered to 15 mg over a 6 month period. Her neurological symptoms and brain MRI abnormalities completely resolved on this regimen (figs 1B and D). The polyarthritis recurred when her daily prednisone was tapered below 20 mg, but resolved after institution of infliximab. However, the neurological symptoms and brain MRI findings (MRI not shown) recurred 4 months after her cyclophosphamide was discontinued and after she had received three doses of infliximab within 3 months. A second course of intravenous cyclophosphamide and oral prednisone treatment was given and her brain MRI findings (MRI not shown) again resolved and the neurological symptoms remitted. The patient's polyarthritis recurred when her daily prednisone was tapered below 20 mg.
As far as we know, this is the first report of the recurrence of rheumatoid meningitis during treatment with the anti‐TNF agent infliximab despite simultaneous resolution of symptomatic polyarthritis. Cyclophosphamide and prednisone had previously produced a complete response of neurological symptoms and MRI abnormalities, as reported in another patient.4 The reasons for recurrence of meningitis in our patient during infliximab treatment are unclear, but one possibility is restricted access of the agent—that is, monoclonal antibodies with high molecular weights, into the central nervous system through the intact blood‐brain barrier. Although the penetration of infliximab across the blood‐brain barrier has not been measured, the penetration of other therapeutic monoclonal antibodies is between 0.1% and 0.3% of serum levels in patients with leptomeningeal cancer.5,6 None the less, responses of central nervous system lymphoma to intravenous rituximab,7 metastatic breast cancer to trastuzumab,8 and neuro‐Behçet's disease9 and neurosarcoidosis10 to infliximab have been reported. Conceivably, therefore, failure of treatment by infliximab is related to the ineffectiveness of an anti‐TNF agent for the granulomatous disease of rheumatoid meningitis.11 Rituximab or other monoclonal antibodies may have promising therapeutic effects for rheumatoid meningitis in the future as rituximab has been shown to be effective for different autoimmune diseases, including RA.12 Further reports of the effect of these agents on the extra‐articular manifestations of RA are needed.
References
- 1.Bathon J M, Moreland L W, Dibartolomeo A G. Inflammatory central nervous system involvement in rheumatoid arthritis. Semin Arthritis Rheum 198918258–266. [DOI] [PubMed] [Google Scholar]
- 2.Hochberg M C, Lebwohl M G, Plevy S E, Hobbs K F, Yocum D E. The benefit/risk profile of TNF‐blocking agents: findings of a consensus panel. Semin Arthritis Rheum 200534819–836. [DOI] [PubMed] [Google Scholar]
- 3.Micheli F, Scorticati M C, Pikielny R, Zurru C, Gatto E M. Pachymeningeal thickening in rheumatoid arthritis. Eur Neurol 199333397–398. [DOI] [PubMed] [Google Scholar]
- 4.Yucel A E, Kart H, Aydin A, Agildere A M, Benli S, Altinorrs A.et al Pachymeningitis and optic neuritis in rheumatoid arthritis: Successful treatment with cyclophosphamide. Clin Rheumatol 200120136–139. [DOI] [PubMed] [Google Scholar]
- 5.Pestalozzi B C, Brignoli S. Trastuzumab in CSF. J Clin Oncol 2000182349–2351. [DOI] [PubMed] [Google Scholar]
- 6.Rubenstein J L, Combs D, Rosenberg J, Levy A, McDermott M, Damon L.et al Rituximab therapy for CNS lymphomas: targeting the leptomeningeal compartment. Blood 2003101466–468. [DOI] [PubMed] [Google Scholar]
- 7.Wong E T, Tishler R, Barron L, Wu J K. Immunochemotherapy with rituximab and temozolomide for central nervous system lymphomas. Cancer 2004101139–145. [DOI] [PubMed] [Google Scholar]
- 8.Baculi R H, Suki S, Nisbett J, Leeds N, Groves M. Meningeal carcinomatosis from breast carcinoma responsive to trastuzumab. J Clin Oncol 2001193297–3298. [DOI] [PubMed] [Google Scholar]
- 9.Sarwar H, McGrath H, Jr, Espinoza L R. Successful treatment of long‐standing neuro‐Behçet's disease with infliximab. J Rheumatol 200532181–183. [PubMed] [Google Scholar]
- 10.Sollberger M, Fluri F, Baumann T, Sonnet S, Tamm M, Steck A J.et al Successful treatment of steroid‐refractory neurosarcoidosis with infliximab. J Neurol 2004251760–761. [DOI] [PubMed] [Google Scholar]
- 11.Wegener's Granulomatosis Etanercept Trial (WGET) Research Group Etanercept plus standard therapy for Wegener's granulomatosis. N Engl J Med 2005352351–361. [DOI] [PubMed] [Google Scholar]
- 12.Edwards J C, Szczepanski L, Szechinski J, Filipowicz‐Sosnowska A, Emery P, Close D R.et al Efficacy of B‐cell‐targeted therapy with rituximab in patients with rheumatoid arthritis. N Engl J Med 20043502572–2581. [DOI] [PubMed] [Google Scholar]