Foot problems constitute a major problem in up to 90% of patients with rheumatoid arthritis, causing pain and functional limitations.1,2 Forefoot deformities are often complicated by ulcers, which can infect the foot and result in major septic complications. Although no data are available on the effect of foot problems on function and quality of life in patients with rheumatoid arthritis, in patients with diabetes mellitus these scores drop substantially.3
Foot problems can be treated by the use of orthotic devices and custom‐made shoes, or by a variety of surgical techniques.1,4 We conducted a cross‐sectional, multicentre study to assess the burden of forefoot problems and current management in 285 consecutive patients with rheumatoid arthritis in five university and non‐university centres between January and April 2004. The mean age of patients was 57 years (SD 12.6), the mean disease duration was 9.7 years (SD 7.9) and the mean score of health assessment questionnaire5 was 1.17 (SD 0.79). In all, 89% of the patients were on disease‐modifying antirheumatic drugs.
A history or presence of any foot ulcer, the use of orthotic devices, custom‐made shoes and foot surgery were noted. Patients were also evaluated by the American Orthopaedic Foot and Ankle Society for Metatarsophalangeal Joint I‐Forefoot Score.6 Correlations were analysed using Spearman's rank analysis or χ2 test.
The results of the American Orthopaedic Foot and Ankle Society analysis showed an overall mean of 70.1 (SD 18.4), which correlated significantly with the scores of health assessment questionnaire (R = −0.40, p<0.001) and disease duration (R = −0.21, p = 0.003). Forefoot pain was debilitating in 6% of patients, marked in 28%, mild in 47% and absent in 19%.
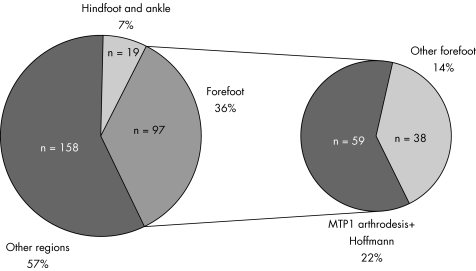
In all, 13% of the patients had presented in the course of disease with foot wounds, with 5% having an active ulcer at the time of the survey; 4% of the patients had had multiple wound problems. Also, 42% of the patients reported wearing insoles; 12% had worn insoles but had discontinued their use, and 25% of patients were wearing custom‐made shoes. Fourteen patients had already used either insoles (n = 7) or custom‐made shoes (n = 7) when an ulcer occurred, and in four patients this event led to additional modifications. Only six patients did not have footwear modification before or after the occurrence of an ulcer. Table 1 shows an overview of foot and ankle procedures carried out. The share of foot and ankle procedures carried out is shown in fig 1.
Table 1 Types of foot and ankle procedures carried out because of rheumatoid arthritis.
| Joint non‐sacrificing foot procedures7 (16/81 procedures) | Joint sacrificing foot procedures7 (100/193 procedures) |
|---|---|
| Release or repair (n = 8) | Arthroplasty (n = 5) |
| Achilles tendon (n = 2) | Ankle (n = 4) |
| Posterior tibial tendon (n = 6) | MTP1 (n = 1) |
| Resection of nodules (n = 5) | Resection arthroplasty (n = 39) |
| Foot (n = 5) | Lesser toes (Hoffmann) (n = 32) |
| Keller–Lelievre (n = 5) | |
| Keller of the fifth ray (n = 2) | |
| Wound surgery (n = 1) | Arthrodesis (n = 56) |
| “Classic” hallux valgus correction (n = 1) | MTP1 (n = 27) PIP of the lesser toes (n = 20) |
| Lesser ray shortening (n = 1) | IP of the Hallux (n = 2) |
| Hindfoot (triple arthrodesis) (n = 7) |
IP, interphalangeal joint; MTP, metatarsophalangeal joint; PIP, proximal interphalangeal joint.
Figure 1 Share of foot and ankle procedures carried out, compared with those carried out in other anatomical regions. MTP, metatarsophalangeal.
In all, 48 patients had a total of 97 forefoot procedures; 12 patients had a total of 19 hindfoot and ankle procedures (7 had undergone both forefoot and hindfoot procedures). Only five patients were dissatisfied with the results. A trend towards earlier foot surgery was seen in patients diagnosed in 1990 or later. Of the cohort diagnosed before 1990 (n = 71), only one patient was operated on the foot or ankle region in the first 5 years of disease, whereas in the cohort diagnosed thereafter, and having a disease duration of at least 5 years (n = 128), 12 patients were operated.
The burden of foot problems in rheumatoid arthritis is impressive and deserves the attention of the treating doctors. The use of the Disease Assessment Score 28 in clinical practice, although increasing the effectiveness of medical treatment,8,9 should be accompanied by a specific foot and ankle examination. The occurrence of foot wounds frequently forms the starting point of a cascade of orthotic and surgical treatment strategies, and deserves attention in an era of biological treatments. Surgical treatment has changed over the past 10–15 years,9 with some groups reporting less surgery.7 Our study suggests a trend to earlier intervention in foot and ankle surgery, possibly owing to the changing expectation levels of patients and doctors. In foot and ankle surgery, joint sacrificing procedures still form the mainstay of treatment.
Footnotes
Funding: This study was supported by a grant from the Belgian “Fonds voor Wetenschappelijk Reuma Onderzoek”.
Competing interests: None.
Competing interests: None declared
References
- 1.Coughlin M J. Rheumatoid forefoot reconstruction. A long‐term follow‐up study. J Bone Joint Surg 200082322–341. [PubMed] [Google Scholar]
- 2.Michelson J, Easley M, Wigley F M, Hellmann D. Foot and ankle problems in rheumatoid arthritis. Foot Ankle Int 199415608–613. [DOI] [PubMed] [Google Scholar]
- 3.Price P, Harding K. The impact of foot complications on health‐related quality of life in patients with diabetes. J Cutan Med Surg 2000445–50. [DOI] [PubMed] [Google Scholar]
- 4.Grifka J K. Shoes and insoles for patients with rheumatoid foot disease. Clin Orthop 199734018–25. [DOI] [PubMed] [Google Scholar]
- 5.Fries J F, Spitz P, Kraines R G, Holman H R. Measurement of patient outcome in arthritis. Arthritis Rheum 198023137–145. [DOI] [PubMed] [Google Scholar]
- 6.Kitaoka H B, Alexander I J, Adelaar R S, Nunley J A, Myerson M S, Sanders M. Clinical rating system for the ankle‐hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 199415349–353. [DOI] [PubMed] [Google Scholar]
- 7.Boonen A, Matricali G A, Verduyckt J, Taelman V, Verschueren P, Sileghem A.et al Orthopaedic surgery in patients with rheumatoid arthritis. A shift towards more frequent and earlier non joint‐sacrificing surgery. Ann Rheum Dis 2005 [DOI] [PMC free article] [PubMed]
- 8.Fransen J, Bernelot Moens H, Speyer I, van Riel P L C M. The effectiveness of systematic monitoring of RA disease activity in daily practice (TRAC): a multi centre, cluster‐randomised controlled trial. Ann Rheum Dis 2005641294–1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fuchs H A, Brooks R H, Callahan L F, Pincus T. A simplified twenty‐eight joint quantitative articular index in rheumatoid arthritis. Arthritis Rheum 198932531–537. [DOI] [PubMed] [Google Scholar]
- 10.da Silva E, Doran M F, Crowson C S, O'Fallon W M, Matteson E L. Declining use of orthopedic surgery in patients with rheumatoid arthritis? Results of a long‐term, population‐based assessment. Arthritis Rheum 200349216–220. [DOI] [PubMed] [Google Scholar]