Antiphospholipid (Hughes) syndrome (APS) is a prothrombotic disorder associated with venous and arterial thrombosis. Arterial stenosis, particularly affecting the renal, coeliac and intracerebral arteries, has been observed. Anticoagulation with international normalised ratio ⩾3 may be able to improve hypertension and the renal function. We report a patient with APS and abdominal angina due to coeliac artery stenosis, whose condition improved on prolonged anticoagulation treatment.
A 39‐year‐old Caucasian woman was diagnosed with systemic lupus erythematosus and secondary Sjögren's syndrome in 1999. Her lupus anticoagulant tests (dilute Russell viper venom test) were positive more than once. However, no previous thrombosis or pregnancy loss was reported. She was treated with hydroxychloroquine 200 mg once daily and aspirin 75 mg/day. In December 2003, the patient had epigastric pain that was worse on eating, especially large meals, and a weight loss of about 6 kg. Clinically, an epigastric bruit was noted. Gastrointestinal endoscopy and colonoscopy were normal. Mesenteric angina was suspected and magnetic resonance angiography (MRA) showed a very tight stenosis of the coeliac artery of >90% (fig 1). Both renal arteries, superior mesenteric artery and the abdominal aorta were normal. Investigations for classical causes of mesenteric angina—hypertension, hypercholesterolaemia and diabetes—were negative; body mass index was normal; the patient did not smoke; and no cardiac arrhythmia was noted. Treatment with warfarin was begun, with a target international normalised ratio (INR) of 3.0–4.0. The median INR was maintained at >3.0. Ten months later, the abdominal pain had improved, the patient's weight remained stable and repeat MRA showed no change in the coeliac artery stenosis. Twenty two months after the diagnosis of coeliac artery stenosis, the abdominal pain completely disappeared and the patient's weight returned to normal. It will be interesting to note the changes in the stenotic lesion on high‐intensity anticoagulation when the patient is seen at follow‐up next year.
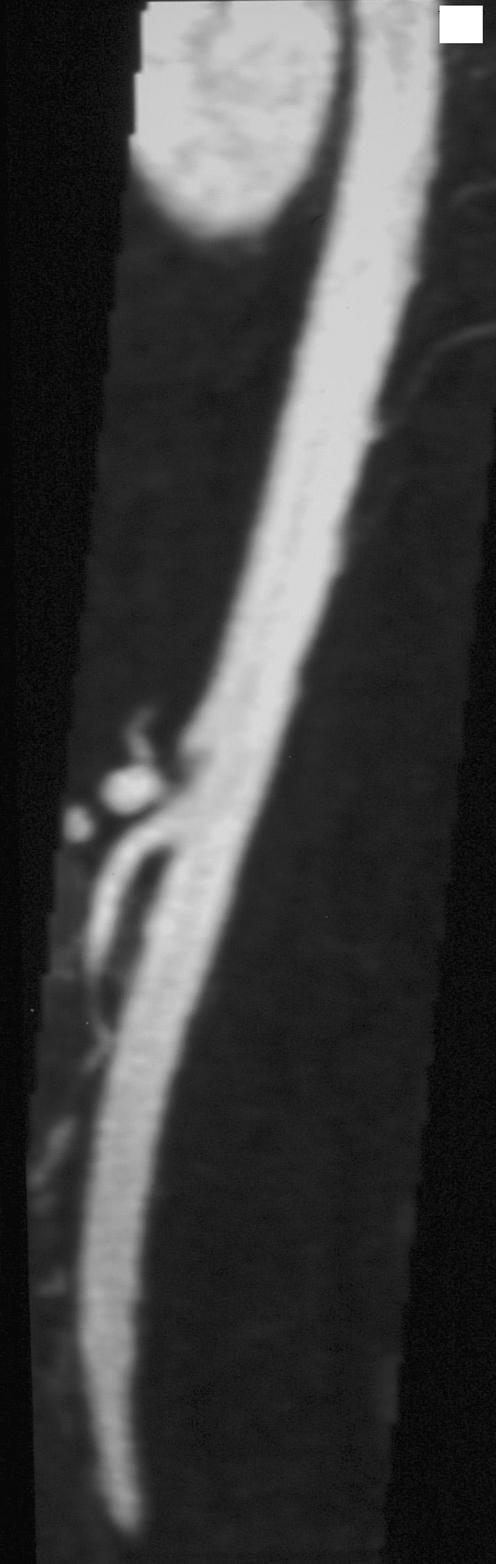
Figure 1 Magnetic resonance angiography showing coeliac artery stenosis in a patient with antiphospholipid syndrome the arrow indicates celiac arrery stenasis.
Atherosclerotic coeliac artery stenosis usually occurs in elderly patients, smokers or patients with cardiac arythmia. Our patient did not have any of these risk factors. We avoided false‐positive coeliac artery stenosis secondary to arcuate ligament syndrome, as our patient was investigated by MRA in suspended inspiration.1 Antiphospholipid syndrome (APS) has recently been recognised in association with arterial stenosis2,3,4,5 of the renal,3 intracranial,4 and coeliac or mesenteric5 arteries. The arterial lesions seen in APS consist of smooth, well‐delineated narrowing at the proximal segment, distinct from atherosclerosis and fibromuscular dysplasia lesions.3 The underlying pathology and mechanism for these stenotic lesions are unknown, but may include thrombosis, accelerated atherosclerosis or proliferation of smooth muscle.3 Our recent reports suggest that anticoagulation with high INR (>3.0) may reverse the renal artery stenosis, with subsequent improvement of hypertension and renal function.2 These data suggested that thrombosis may be the basis for the development of coeliac artery stenosis in patients with APS. Although our patient never had any thrombosis, given her symptoms, positive lupus anticoagulant and coeliac artery stenosis, a consensus opinion about anticoagulation was reached among treating doctors, consulting surgeon and the patient.
Treatment of chronic abdominal angina in patients with atherosclerotic vascular disease classically relies on revascularisation.6 No effective medical treatment exists. Our observations constitute the first report on the clinical efficacy of prolonged anticoagulation in a patient with abdominal angina and coeliac artery stenosis. Although coeliac artery stenosis was still present 10 months after the introduction of anticoagulation, clinical signs improved and completely resolved 2 years later. As in renal artery stenosis, warfarin with a target INR of 3.0–4.0 may be considered in patients with coeliac artery stenosis and APS.
Abbreviations
APS - antiphospholipid syndrome
INR - international normalised ratio
MRA - magnetic resonance angiography
Footnotes
Competing interests: None declared.
References
- 1.Lee V, Morgan J, Andrew G, Pandharipande P V, Krinsky G A, Barker J A. Celiac artery compression by the median arcuate ligament: a pitfall of end‐expiratory MR imaging. Radiology 2003228437–442. [DOI] [PubMed] [Google Scholar]
- 2.Sangle S, D'Cruz D, Khamashta M A, Hughes G R V. Renal artery stenosis in hypertensive patients with antiphospholipid syndrome: the effect of anticoagulation. Arthritis Rheum 200343S359. [DOI] [PubMed] [Google Scholar]
- 3.Sangle S R, D'Cruz D P, Jan W, Karim M Y, Khamashta M A. Renal artery stenosis in antiphospholipid syndrome and hypertension. Ann Rheum Dis 200362999–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wong M, Sangle S, Jan W, Hughes G R V, D'Cruz D P. Intracerebral arterial stenosis with neurological events associated with antiphospholipid syndrome. Rheumatology 200544948–957. [DOI] [PubMed] [Google Scholar]
- 5.Sangle S, Jan W, Lav I, Berrett A, Rankin S C, Hughes G R V.et al Coeliac artery stenosis in patients with antiphospholipid syndrome/antiphospholipid antibodies [abstract 1596]. Arthritis Rheum 200552S596 [Google Scholar]
- 6.Sreenarasimhaiah J. Chronic mesenteric angina. Best Pract Res Clin Gastroenterol 200519283–295. [DOI] [PubMed] [Google Scholar]


