Lupus enteritis is a term applied to the alimentary tract lesions in systemic lupus erythematosus (SLE) and may affect any part of the gastrointestinal tract. Previously, we reported clinical findings in patients with SLE who had acute abdominal pain, focusing on lupus enteritis.1 During follow‐up, several patients with lupus enteritis experienced recurrence after complete remission with high‐dose corticosteroids. To find the factors contributing to recurrence of lupus enteritis, we investigated 16 patients who were diagnosed for lupus enteritis between January 1993 and January 2003.
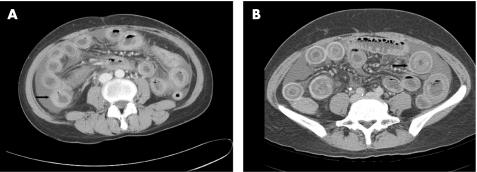
At first admission, we retrospectively reviewed patients' demographic data, laboratory data, including autoantibody profiles (anti‐dsDNA, anti‐Sm antibody, anti‐ribonucleoprotein antibody, anti‐Ro antibody, anti‐La antibody and antiphospholipid antibody), abdominal computed tomography scans and SLE disease activity index (SLEDAI; table 1). Lupus enteritis was diagnosed clinically and from abdominal computed tomography findings: bowel thickening ⩾3 mm, target sign, dilatation of intestine, engorgement of mesenteric vessels and increased attenuation of mesenteric fat (fig 1).2,3 Patients were treated with intravenous methylprednisolone (1 mg/kg/day) and switched to oral prednisolone (median 5 days), which was tapered slowly over a period of 10 months. Bowel wall thickness was measured by an experienced radiologist who had no information about the clinical outcome.
Table 1 Comparison of groups with non‐recurrent and recurrent lupus enteritis at initial admission.
| Non‐recurrent group (n = 7) | Recurrent group (n = 9) | p Value | |||
|---|---|---|---|---|---|
| Age (years)* | 32.1 (9.4) | 30.0 (6.3) | 0.75 | ||
| Sex | |||||
| Male | 1 | 1 | 0.70 | ||
| Female | 6 | 8 | 0.70 | ||
| White cell count (×109)/l* | 8.6 (4.7) | 5.4 (0.9) | 0.12 | ||
| Haemoglobin (g/l)* | 10.9 (2.6) | 12.1 (1.4) | 0.05 | ||
| Platelets (×109)/l* | 259.0 (88.7) | 257.6 (103.3) | 0.71 | ||
| ESR (mm/1/h)* | 52.1 (18.1) | 41.3 (19.2) | 0.34 | ||
| CRP (mg/l)* | 4.2 (4.2) | 1.6 (3.1) | 0.15 | ||
| C3 (mg/l)* | 56.2 (13.2) | 48.0 (9.0) | 0.24 | ||
| C4 (mg/l)* | 13.4 (5.1) | 13.0 (6.5) | 0.23 | ||
| Anti‐dsDNA (IU/ml)* | 69.8 (65.2) | 128.7 (156.2) | 0.87 | ||
| SLEDAI score* | 7.6 (6.0) | 7.9 (4.7) | 0.75 | ||
| PD cumulative dose (g)* | 14.7 (6.0) | 7.6 (2.4) | 0.02 | ||
| Duration of PD treatment (month)* | 50.0 (32.8) | 16.9 (7.4) | 0.04 | ||
| Thickness of bowel wall† (mm)* | 6.1 (2.6) | 9.0 (3.7) | 0.08 | ||
C, complement; CRP, C‐reactive protein; ESR, erythrocyte sedimentation rate; PD, prednisolone; SLEDAI, systemic lupus erythematosus disease activity index.
*Values are given as mean (SD).
†Measured at the most thickened site in the affected bowel on abdominal computed tomography scan.
Figure 1 Computed tomography scans of patients with non‐recurrent (A) and recurrent (B) lupus enteritis. Both scans show ascites, mesenteric congestion and diffuse oedematous change in nearly whole halo viscous with engorged mesenteric vessels. The arrow indicates the thickest wall segment of the affected bowel.
Of the 16 patients followed up for >30 months (median 67 months), 7 patients showed no evidence of recurrence whereas 9 had recurrent lupus enteritis. When we compared clinical characteristics in patients with non‐recurrent and recurrent lupus enteritis there were no differences in demographic and laboratory indices, including autoantibody profiles and SLEDAI score, between the two groups. However, in patients with non‐recurrent lupus enteritis, the cumulative dose of prednisolone (p = 0.02) and duration of treatment with prednisolone (p = 0.04) was significantly higher than in patients with recurrent lupus enteritis.
The wall thickness of the most thickened bowel in patients with recurrent lupus enteritis (mean (SD); 9.0 (3.7) mm) was greater than in patients with non‐recurrent lupus enteritis (6.1 (2.6) mm), although the difference was not significant (p = 0.08). All the five patients with bowel wall thickness ⩾9 mm experienced recurrence. This finding may be considered a high‐risk factor for recurrent lupus enteritis.
Cumulative dose and duration of treatment may be influenced by other complications of SLE, including lupus nephritis. In our study, class II lupus nephritis was newly diagnosed during prednisolone tapering in three patients (2/7 in non‐recurrent, 1/9 in recurrent group), prolonging the duration of treatment with prednisolone. Despite this confounding variable, the dose and duration of corticosteroids was related more closely to the recurrence of lupus enteritis than laboratory indices, including autoantibody profiles and SLEDAI score reflecting lupus activity.
Successful treatment with high‐dose prednisolone and intravenous pulse cyclophosphamide has been reported in many patients with intestinal vasculitis, and immunosuppressants such as cyclophosphamide may be recommended for patients with severe or steroid‐resistant lupus enteritis.4,5 In conclusion, longer treatment with corticosteroids or treatment with additional immunosuppressants may be considered in patients with lupus enteritis and with initial bowel wall thickening >9 mm.
Footnotes
Competing interests: None declared.
References
- 1.Lee C K, Ahn M S, Lee E Y, Shin J H, Cho Y S, Ha H K.et al Acute abdominal pain in systemic lupus erythematosus: focus on lupus enteritis (gastrointestinal vasculitis). Ann Rheum Dis 200261547–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ha H K, Lee S H, Rha S E, Kim J H, Byun J Y, Lim H K.et al Radiologic reatures of vasculitis involving the gastrointestinal tract. Radiographics 200020779–794. [DOI] [PubMed] [Google Scholar]
- 3.Byun J Y, Ha H K, Yu S Y, Min J K, Park S H, Kim H Y.et al CT features of systemic lupus erythematosus in patients with acute abdominal pain: emphasis on ischemic bowel disease. Radiology 1999211203–209. [DOI] [PubMed] [Google Scholar]
- 4.Cabrera G E, Scopelitis E, Cuellar M L, Silveira L H, Mena H, Espinoza L R. Pneumatosis cystoides intestinalis in systemic lupus erythematosus with intestinal vasculitis: treatment with high dose prednisone. Clin Rheumatol 199413312–316. [DOI] [PubMed] [Google Scholar]
- 5.Grimbacher B, Huber M, von Kempis J, Kalden P, Uhl M, Kohler G.et al Successful treatment of gastrointestinal vasculitis due to systemic lupus erythematosus with intravenous pulse cyclophosphamide: a clinical case report and review of the literature. Br J Rheumatol 1998371023–1028. [DOI] [PubMed] [Google Scholar]