Treatments directed against the proinflammatory cytokine tumour necrosis factor α (TNFα) are effective in rheumatoid arthritis and spondyloarthropathies. In patients with inflammatory arthritis secondary to psoriasis, chronic skin plaques also resolve with this treatment. We report on a series of clinical cases in which, conversely, there was a first presentation of psoriasis while on anti‐TNF treatment.
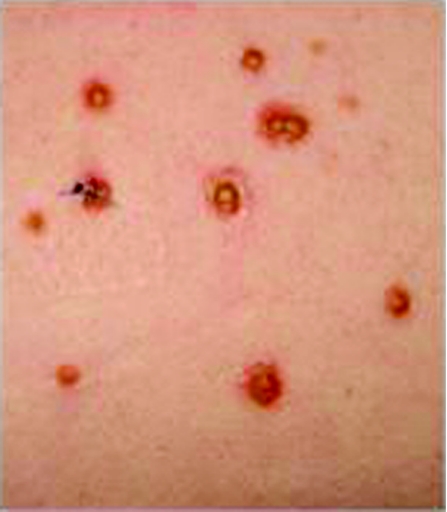
The first case is that of a 49‐year‐old man with established ankylosing spondylitis, who was started on infliximab and showed an excellent response. After 8 months of treatment, he developed an erythematous, pustular rash over his back (fig 1). No clinical or serological evidence of infection was found and his medication, including methotrexate, was stable.
Figure 1 Vesicular rash on the patient's back. The lesions formed small pustules on a red base with areas of encrustation. The eruption suggested pustular psoriasis.
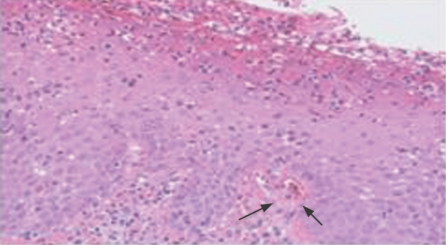
Although antinuclear antibodies were positive, the rash was not suggestive of photosensitivity. Histological examination of the lesion showed that it was consistent with acute pustular psoriasis (fig 2), which resolved by increasing the methotrexate dose.
Figure 2 Haematoxylin and eosin stain of skin lesion showing orthokeratosis of the epidermis, with perivascular lymphocytic infiltrate in the superficial papillary dermis. Neutrophils in the superficial stratum spinosum are consistent with acute psoriasis.
The second case was that of a 68‐year‐old woman with psoriatic arthritis (PsA), who was started on infliximab, with initial resolution of her plaque psoriasis and inflammatory arthritis. She subsequently developed a new variant of psoriasis that was flexural, affecting her axillae and groin. This resolved with topical treatments.
The final case is that of a 54‐year‐old woman with seropositive rheumatoid arthritis, who was started on adalimumab. After 10 months of treatment, she developed hyperkeratotic skin lesions consistent with guttate psoriasis. There was a positive family history of plaque psoriasis. Her rash completely resolved with conservative management.
Blockade of TNFα is an effective treatment for recalcitrant plaque psoriasis.1,2,3 In contrast, we report three cases in which anti‐TNF treatment is associated with new‐onset psoriasis. The psoriasis phenotype varied between pustular, flexural or guttate, respectively. The exact aetiology of this is unclear. It may represent asymptomatic infection. Guttate psoriasis may be precipitated by Group A β‐haemolytic streptococcal infection, where superantigens are hypothesised to play a part in disease pathogenesis.4 Triggering by varicella zoster has been reported.5 Colonisation of skin by microbes, including yeasts and gut flora, may have a role in the pathogenesis of psoriasis.6 Therefore, anti‐TNF treatment may predispose a susceptible person to the development of psoriasis triggered by common, commensal organisms.
The development of psoriasis is probably multifactorial. The association of ankylosing spondylitis with psoriasis is recognised. In the patient with a diagnosis of rheumatoid arthritis, there was a family history of psoriasis, suggesting that there was an additional genetic risk.7
The development of new‐onset psoriasis in patients on anti‐TNF treatment is not common.8 We describe three cases out of approximately 400 patients who have been treated since 1999. The effect of TNF blockade, combined with other precipitating factors, seems to occasionally result in dysregulation of T cells in the epidermis and increased keratinocyte proliferation, with the subsequent development of psoriasis.
Abbreviations
TNF - tumour necrosis factor
Footnotes
Competing interests: None.
Informed consent was obtained for publication of the patients' details in this report.
References
- 1.O'Quinn R P, Miller J L. The effectiveness of tumor necrosis factor alpha antibody (infliximab) in treating recalcitrant psoriasis: a report of 2 cases. Arch Dermatol 2002138644–648. [DOI] [PubMed] [Google Scholar]
- 2.Nikas S N, Voulgari P V, Takalou I P, Katsimbri P, Drosos A A. Healing of psoriatic skin lesions, and improvement of psoriatic arthritis resistant to immunosuppressive drugs, after infliximab treatment. Ann Rheum Dis 2005641665–1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leonardi C L, Powers J L, Matheson R T, Goffe B S, Zitnik R, Wang A.et al Etanercept monotherapy in patients with psoriasis. N Eng J Med 2003345248. [DOI] [PubMed] [Google Scholar]
- 4.Valdimarsson H, Baker B S, Jonsdottir I, Powles A, Fry L. Psoriasis: a T cell mediated autoimmune disease induced by streptococcal superantigens? Immunol Today 199516145–149. [DOI] [PubMed] [Google Scholar]
- 5.Ito T, Furukawa F. Psoriasis guttate acuta triggered by varicella zoster virus infection. Eur J Dermatol 200010226–227. [PubMed] [Google Scholar]
- 6.Skinner R B, Rosenburgh E W, Noah P W. Antimicrobial treatment of psoriasis. Dermatol Clin 199513909–913. [PubMed] [Google Scholar]
- 7.Naldi L, Peli L, Parazzini F, Carrel C F. Family history of psoriasis, stressful life events and recent infectious disease are risk factors for a first episode of acute guttate psoriasis: results of a case‐ control study. J Am Acad Dermatol 200144433–438. [DOI] [PubMed] [Google Scholar]
- 8.Sfikakis P P, Iliopoulos A, Elezoglou A, Kittas C, Stratigos A. Psoriasis induced by anti‐TNF therapy: a paradoxical adverse reaction. Arthritis Rheum 2005522513–2518. [DOI] [PubMed] [Google Scholar]