Thrombocytopenia in patients with systemic lupus erythematosus (SLE) requires immunosuppressive treatment to restore normal platelet counts and treat concomitant organ involvement in other systems.1,2,3,4,5,6 However, relapses are quite common during the course of the disease.7
From 1995 to 2004, 38 consecutive patients with SLE with a first episode of thrombocytopenia (platelet count <100 000/μl) were retrospectively assessed. Platelet counts, disease activity (European Consensus Lupus Activity Measurement (ECLAM)),8 C3 level, type of treatment and organ involvement were recorded at onset of thrombocytopenia. Relapse was twice defined as a drop in platelet count <100 000/μl after achieving response (increase >150 000). Severe thrombocytopenia (<20 000/μl) was recorded in 34.2% of patients with rare haemorrhagic manifestations. Organ involvement included, in descending order, arthritis (31.6%), renal disease (29%), rash (18.5%), manifestations of the central nervous system (13.2%) and serositis (9%). Low C3 levels (mean 46.0 (standard deviation (SD) 11.9 mg/dl)) were noted in 39.5% of patients, indicating possible complement activation. This group did not exhibit statistically significant differences in platelet counts, disease activity or clinical features compared with those with normal C3 levels. Anticardiolipin antibodies were recorded in 31.6% of patients unassociated with lower platelet counts (mean 36.7 (SD 28.3×103) v 49.1 (SD 32.3×103)/μl; p = 0.22). All patients had active disease (mean ECLAM 3.1 (SD 1.6)) and received immunosuppressive treatment, including corticosteroids (n = 38), cyclophosphamide (n = 10), azathioprine (n = 4) and mucofenolate mofetil (n = 1), the selection criteria of which were based on the major organ involvement. Intravenous immunoglobulin was used as an adjuvant in patients with severe thrombocytopenia. All but one patient had achieved response in platelet counts. However, 36.8% of patients relapsed during disease course (median 1, range 0.3–7 years).
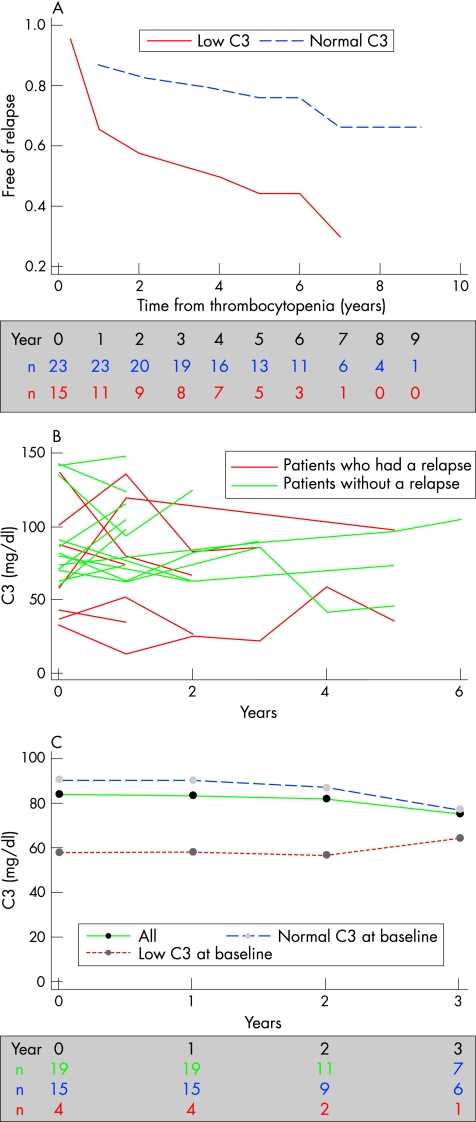
Low complement levels (C3 <55 mg/dl) at the onset of thrombocytopenia predicted relapse (hazard ratio 3.07, 95% confidence interval 1.03 to 9.17, p = 0.04), whereas disease activity or therapeutic interventions did not. The effect persisted after adjusting for ECLAM score (table 1, fig 1A). Nineteen patients, having at least two C3 serial measurements (median 3, range 2–7) were eligible for further analysis, and individual profiles were constructed (fig 1B). C3 levels during relapse of thrombocytopenia were low in all patients (fig 1B). Recent evidence associates low C3 levels with certain SLE features, including nephritis and haematological manifestations.7,9 Despite complement consumption being a well‐known activity marker, none of the relapsing patients displayed flares in other systems, other than thrombocytopenia itself, indicating that the predictive value of C3 in this group was independent of other systems involved.
Table 1 Univariate and multivariate Cox‐regression analysis.
| Hazard ratio | 95% CI | p Value | |
|---|---|---|---|
| Univariate analysis | |||
| Age at thrombocytopenia | 0.98 | 0.95 to 1.02 | 0.47 |
| ECLAM | 1.16 | 0.84 to 1.64 | 0.35 |
| Corticosteroids | 1.19 | 0.39 to 3.68 | 0.76 |
| Cyclophosphamide | 1.36 | 0.41 to 4.50 | 0.61 |
| Intravenous immunoglobulin | 1.50 | 0.50 to 4.46 | 0.47 |
| Azathioprine | 0.64 | 0.08 to 4.98 | 0.67 |
| Anticardiolipin | 0.82 | 0.25 to 2.68 | 0.74 |
| Low C3 | 3.07 | 1.03 to 9.17 | 0.04 |
| Multivariate analysis | |||
| ECLAM* | 0.99 | 0.69 to 1.44 | 0.98 |
| Low C3 | 3.08 | 1.02 to 9.28 | 0.04 |
ECLAM, European Consensus Lupus Activity Measurement.
Variable definition (high v low dose corticosteroids prednisololone ⩾0.5 mg/kg/day v <15 mg/day, cyclophosphamide: 750 mg/m2/month intravenous v no administration; intravenous immunoglobulin: 400 mg/kg/day for 5 days v no administration; azathioprine: 150 mg/day v no administration; anticardiolipin antibodies: positive v negative).
*Low complement was not scored in ECLAM in multivariate analysis for a more accurate comparison.
Figure 1 (A) Predicted probabilities based on Cox's regression analysis of the remaining patients free of relapse according to complement activity at the onset of thrombocytopenia: 83% at 2 years and 76% at 5 years will be free of relapse if C3 levels are normal. Only 58% and 44% of patients respectively, will be free of relapse if C3 levels are low. (B) Individual profile of patients with at least two serial C3 measurements (n = 19). Relapses occurred (A) in all patients presenting with low C3 levels at onset of thrombocytopenia and (B) in three patients with normal C3 levels at the onset of thrombocytopenia but subsequent drops. (C) Longitudinal analysis (panel‐corrected standard errors, with first‐order autocorrelation). Average predicted profile for C3, stratified for baseline C3 levels. Low baseline C3 levels is associated with sustained low values over time.
Baseline C3 was an independent predictor, and a difference of −10 mg/dl at baseline predicted sustained mean levels by −7.17 (95% CI −5.86 to −8.49; p<0.001) after adjustment for protein loss in the urine. When average predicted profiles were plotted after stratification for low C3 levels, patients with low baseline C3 will have sustained low C3 levels (fig 1C).
Therefore, low baseline C3 levels seem to correlate with an increased risk of relapse in thrombocytopenia in patients with SLE, and predict subsequent C3 measurements. Active patients with a history of thrombocytopenia and a low complement level are likely to experience relapse in thrombocytopenia, regardless of other system flares. The study limitations regard its retrospective characteristics. As 50% of patients lack serial time measurements of C3 level, results should be interpreted with caution. A prospective study incorporating serial platelet counts, C3 levels and other clinical and laboratory parameters, although harder to perform, would prove to be more efficient.
Footnotes
Competing interests: None declared.
References
- 1.Arnal C, Piette J C, Leone J, Taillan B, Hachulla E, Roudot‐Thoraval F.et al Treatment of severe immune thrombocytopenia associated with systemic lupus erythematosus: 59 cases. J Rheumatol 20022975–83. [PubMed] [Google Scholar]
- 2.Boumpas D T, Barez S, Klippel J H, Balow J E. Intermittent cyclophosphamide for the treatment of autoimmune thrombocytopenia in systemic lupus erythematosus. Ann Intern Med 1990112674–677. [DOI] [PubMed] [Google Scholar]
- 3.Avina‐Zubieta J A, Galindo‐Rodriguez G, Robledo I, Vela‐Ojeda J, Vadillo‐Buenfil M, Rosas‐Cabral A.et al Long‐term effectiveness of danazol corticosteroids and cytotoxic drugs in the treatment of hematologic manifestations of systemic lupus erythematosus. Lupus 20031252–57. [DOI] [PubMed] [Google Scholar]
- 4.Kneitz C, Wilhelm M, Tony H P. Effective B cell depletion with rituximab in the treatment of autoimmune diseases. Immunobiology 2002206519–527. [DOI] [PubMed] [Google Scholar]
- 5.Vasoo S, Thumboo J, Fong K Y. Refractory immune thrombocytopenia in systemic lupus erythematosus: response to mycophenolate mofetil. Lupus 200312630–632. [DOI] [PubMed] [Google Scholar]
- 6.You Y N, Tefferi A, Nagorney D M. Outcome of splenectomy for thrombocytopenia associated with systemic lupus erythematosus. Ann Surg 2004240286–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ziakas P D, Giannouli S, Zintzaras E, Tzioufas A G, Voulgarelis M. Lupus thrombocytopenia: clinical implications and prognostic significance. Ann Rheum Dis 2005641366–1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mosca M, Bencivelli W, Vitali C, Carrai P, Neri R, Bombardieri S. The validity of the ECLAM index for the retrospective evaluation of disease activity in systemic lupus erythematosus. Lupus 20009445–450. [DOI] [PubMed] [Google Scholar]
- 9.Ho A, Barr S G, Magder L S, Petri M. A decrease in complement is associated with increased renal and hematologic activity in patients with systemic lupus erythematosus. Arthritis Rheum 2001442350–2357. [DOI] [PubMed] [Google Scholar]