Abstract
Objectives
Joint pain and radiographic osteoarthritis are often discordant.
Aim
To investigate this issue more closely by studying the detailed nature of pain and disability, and how this relates to radiographic osteoarthritis.
Methods
Population‐based study of 819 adults aged ⩾50 years with knee pain. The severity of knee pain, stiffness and disability was measured using a validated scale (the Western Ontario and McMaster Universities (WOMAC) Score) and pain persistence was recorded. Global severity was measured by the graded chronic pain scale. Three radiographic views of the knees were obtained—weight‐bearing posteroanterior metatarsophalangeal, supine skyline and supine lateral.
Results
745 participants with knee pain in the past 6 months were eligible (mean age 65 years, 338 men). Radiographic osteoarthritis was more common in those with a longer history and more persistent symptoms. A strong trend was found of radiographic osteoarthritis being more strongly associated with higher WOMAC scores for pain severity, stiffness and disability (adjusted odds ratio (95% confidence interval (CI)) for highest v lowest WOMAC category: 3.7 (2.0 to 6.7), 3.0 (2.0 to 4.6) and 2.8 (1.6 to 5.0), respectively). Those individual WOMAC items for pain and disability pertaining to weight‐bearing mobility were the most strongly associated with radiographic osteoarthritis. Combining pain persistence and global severity, persistent severe pain was associated with a significant increase in the occurrence of radiographic osteoarthritis (2.6 (95% CI 1.5 to 4.7)).
Conclusions
A consistent association was found between severity of pain, stiffness and physical function and the presence of radiographic osteoarthritis. This study highlights the potential contribution of underlying joint disease to the degree of pain and disability.
The discordance between radiographic osteoarthritis and the occurrence of knee pain in the general population has long been recognised1 and is well documented.2,3 Radiographic osteoarthritis occurring in apparently asymptomatic members of the general population argues against “shoe‐horning” the experience of joint pain and associated disability into a strict disease model.4 Despite this discordance, those with more severe radiographic disease have a higher prevalence of pain than those with less severe radiographic disease.5,6,7,8,9,10 This suggests that there is an association between structural markers of the disease and the illness, although several studies have emphasised that this is weak after the influence of other biomechanical, psychological and social factors have been taken into account.11,12,13
Before discarding the role of pathological disease in favour of predominantly psychosocial models of pain and disability, it is important to scrutinise the way that structure–pain associations have been studied. Early studies using restricted radiographic views of the knee may have underestimated the contribution of structural pathology to pain and disability, notably by excluding the patellofemoral joint.8,12 Pain and disability have often been represented in epidemiological studies by simple dichotomous variables—for example, pain absent or present, disability scores above a certain cut‐off point. Fewer studies have investigated severity and other aspects of pain, or task‐specific function.14,15 Studies in clinical settings have been limited to relatively small samples, often with incomplete radiographic views.16,17,18,19 Additionally, the associations of radiographic osteoarthritis with pain and disability may have been masked by adjusting the statistical analysis for variables that are not confounding causes of pain and disability but represent mechanisms through which the disease process (as evidenced by x ray films) influences levels of pain and disability.11
Previously, studies have often selected patients according to radiographic stage of the disease and then assessed pain and disability; however, patients present to clinicians with symptoms, not radiographic changes. An alternative approach is to use individuals with symptoms of pain and disability as a starting point20 and then describe the proportion of individuals with radiographic osteoarthritis. This approach considers the question “Does radiographic osteoarthritis occur more frequently in those with severe or persistent pain compared with those with mild or intermittent pain?” To deal with the issues outlined earlier, we conducted a detailed study of a sample of adults aged ⩾50 years, with self‐reported current or recent knee pain derived from the general population, and we used comprehensive radiographic assessment to investigate the associations between the nature and severity of the pain and disability and the presence of radiographic knee osteoarthritis.
Methods
Study design and population
The Knee Clinical Assessment Study is a prospective observational cohort study of people with knee pain, sampled from the general population. All patients aged ⩾50 years registered with three general practices in North Staffordshire, UK, were invited to take part in a two‐stage postal survey. Almost all patients in the UK are registered with a general practitioner, and local registers provide a convenient sampling framework for the open population irrespective of any consultation they have had. Respondents to this survey phase who indicated that they had experienced knee pain within the previous 12 months were invited to attend a research clinic for a detailed assessment. This consisted of clinical interview, physical examination, digital photography, plain radiographs, anthropometric measurement and a brief self‐complete questionnaire. A detailed description of the study has been previously published.21
This paper reports on cross‐sectional analyses of baseline data from the Knee Clinical Assessment Study. Participants with recent or current knee pain (defined as knee pain within the past 6 months) and complete radiographic data were included in this analysis. Ethical approval was obtained for all phases of the study.
Data collection
Data on knee pain, stiffness and disability were gathered by self‐complete questionnaires. Pain persistence was assessed by single questionnaire items on episode duration,22 days of knee pain in the past 12 months,23 days of knee pain in the past 6 months24 and days of pain, aching or stiffness in the past month.25 An additional question at the personal interview asked participants the total length of time since the onset of their knee problem. The severity of knee pain, stiffness and disability were measured using the 24‐item Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index Likert version 3.0.26,27 Each item had five response options (none, mild, moderate, severe and extreme) and yields total subscale scores for pain (5 items, total score 0–20), stiffness (2 items, total score 0–8) and disability (17 items, total score 0–68).
Global severity—the combination of pain intensity and disability—was measured by the graded chronic pain status,24 which consisted of seven items relating to pain intensity and interference with daily activities, and classified individuals into four hierarchical categories (grade I, low intensity–low disability; grade II, high intensity–low disability; grade III, high disability–moderately limiting; and grade IV, high disability–severely limiting). When self‐completed, the validity and reliability of this measure was verified in a general population sample with chronic pain.28,29
For all consenting participants, we obtained three views of the knee at the clinic. A weight‐bearing posteroanterior semiflexed/metatarsophalangeal view according to the Buckland–Wright protocol,30 a skyline view and a lateral view. The skyline and lateral views were obtained with the patients in a supine position, with the knee flexed to 45° using a wedge for accuracy. The films were recorded in the radiology department at the University Hospital of North Staffordshire, Stoke on Trent, UK, by a team of six radiographers who had all undergone training to standardise the x rays and who met for regular quality control sessions.
Only one knee per individual was analysed, the “index knee”. In patients with unilateral knee pain, the index knee was this single painful knee. In those with bilateral knee pain the most painful knee was the index knee. In situations where participants thought that both knees were similarly painful, the index knee was selected at random.
A single reader (RD) scored all study films and was blinded to all clinical and questionnaire data. Intraobserver and interobserver repeatability was assessed in 50 participants (100 knees); the second reader for the interobserver assessment (PC) had previous experience of grading knee radiographs. Unweighted κ coefficients were calculated. The tibiofemoral joint was assessed using the posteroanterior view and the posterior compartment of the lateral view. The patellofemoral joint was assessed using the skyline and lateral view.
On the basis of those authors' original written description, a Kellgren and Lawrence (K&L) grade was assigned to both the posteroanterior and skyline views as follows: grade 0, no features of osteoarthritis; grade 1, minute osteophyte, doubtful significance; grade 2, definite osteophyte, unimpaired joint space; grade 3, definite osteophyte, moderate diminution of joint space; and grade 4, definite osteophyte, joint space greatly impaired with sclerosis of the subchondral bone.31 In the lateral view, superior and inferior patellar osteophytes were scored using a standard atlas.32 Osteophytes on the posterior tibial surface do not appear in the atlas but were judged on the same basis of severity as other osteophytes in the lateral view.
Osteoarthritis of the knee was defined as a K&L score ⩾2 on the PA view and/or K&L score≥2 on the skyline view and/or the presence of definite superior or inferior patellar osteophytes on the lateral view and/or the presence of posterior tibial osteophytes on the lateral view. Intrareader reliability scores for posteroanterior K&L score, skyline K&L score and lateral osteophytes were very good (unweighted κ = 0.81–0.98); interreader scores were also good (κ = 0.49–0.76).
Statistical analysis
The prevalence of radiographic knee osteoarthritis was described for each level of severity on all individual items relating to pain persistence, pain intensity, stiffness and physical function. Owing to small numbers, the severe and extreme categories for the individual WOMAC items were collapsed. Subscale scores of WOMAC pain and physical function were split into quintiles and the stiffness subscale into tertiles on the basis of their overall distribution, and the prevalence of radiographic knee osteoarthritis was calculated for each category. The associations between severity on each item and radiographic knee osteoarthritis were expressed first as crude odds ratios (ORs) with 95% confidence intervals (CIs), and then after adjustment for age (50–59, 60–69, 70–79, ⩾80 years), sex and body mass index (BMI ⩽24.9, 25–29.9, ⩾30 kg/m2). Finally, to investigate the association of radiographic osteoarthritis with the combination of pain persistence, pain severity and disability, we described the prevalence of radiographic knee osteoarthritis by graded chronic pain status, expressed separately for those with non‐persistent (<90 days knee pain in the previous 6 months) and persistent (⩾90 days) knee pain. Crude and adjusted ORs were calculated using non‐persistent, low‐intensity low‐disability pain (NP I) as the reference category.
Results
Participants
Between August 2002 and September 2003, 819 people attended the research clinic, of whom 745 were eligible for the current analysis (407 women and 338 men; mean (standard deviation (SD)) age 65.2 (8.6) years; mean (SD) BMI 29.6 (5.2) kg/m2). Reasons for ineligibility were patient declined radiography (n = 2), incomplete radiographic data (total knee replacement in index knee (n = 15), unlabelled posteroanterior views (n = 2), absent patella (n = 2) and skyline views deemed uninterpretable (n = 5)), existing diagnosis of inflammatory arthritis, verified by medical record review (n = 16) and no knee pain in the past 6 months (n = 32).
In all, 509 (68.3%) patients from the study sample were classified as having radiographic osteoarthritis in the index knee. The distribution of compartmental radiographic osteoarthritis was combined tibiofemoral/patellofemoral osteoarthritis in 301 (40.4%), isolated patellofemoral osteoarthritis in 178 (23.9%) and isolated tibiofemoral osteoarthritis in 30 (4.0%). The remaining 236 (31.7%) had no evidence of radiographic osteoarthritis.
Association between pain persistence and radiographic osteoarthritis
Radiographic osteoarthritis was more common in those with a longer history and more persistent symptoms. A trend of increasing strength of association with increasing severity of symptoms was observed for most variables and ORs remained significant when adjusted for age and sex. Radiographic osteoarthritis was more common in people with symptoms that had begun >1 year ago, who had not been pain free for a month for >10 years, had >3 months of knee pain in the past 12 months and >90 days of pain in the past 6 months (table 1). When pain, aching or stiffness in the past month was dichotomised (as used to define symptomatic osteoarthritis33) the age‐sex‐adjusted OR for radiographic osteoarthritis was 1.6 (1.1 to 2.1) for most/all days compared with no/few/some days.
Table 1 Occurrence of radiographic knee osteoarthritis in relation to knee pain duration and persistence.
| Adjusted OR (95% CI) | |||||
|---|---|---|---|---|---|
| Variable | Total | Patients with ROA, n (%) | OR (95% CI) | For age and sex | For age, sex and BMI |
| Total duration of symptoms (years) | |||||
| <1 | 91 | 46 (51) | 1 | 1 | 1 |
| 1–5 | 257 | 172 (67) | 2.0 (1.2 to 3.2) | 2.2 (1.3 to 3.7) | 2.0 (1.2 to 3.4) |
| 5–10 | 150 | 100 (67) | 2.0 (1.2 to 3.3) | 1.9 (1.1 to 3.4) | 1.9 (1.0 to 3.3) |
| ⩾10 | 247 | 191 (77) | 3.3 (2.0 to 5.5) | 3.2 (1.9 to 5.4) | 3.0 (1.7 to 5.2) |
| Last time pain free for a month | |||||
| <3 months | 232 | 153 (66) | 1 | 1 | 1 |
| 3–6 months | 94 | 60 (64) | 0.9 (0.6 to 1.5) | 0.9 (0.6 to 1.6) | 1.1 (0.6 to 1.8) |
| 7–12 months | 57 | 31 (54) | 0.6 (0.3 to 1.1) | 0.6 (0.3 to 1.1) | 0.5 (0.3 to 1.0) |
| 1–2 years | 68 | 46 (68) | 1.1 (0.6 to 1.9) | 1.3 (0.7 to 2.3) | 1.1 (0.6 to 2.1) |
| 3–5 years | 120 | 83 (69) | 1.2 (0.7 to 1.9) | 1.2 (0.7 to 2.0) | 1.1 (0.7 to 1.9) |
| 6–10 years | 83 | 60 (72) | 1.4 (0.8 to 2.3) | 1.2 (0.7 to 2.2) | 1.1 (0.6 to 2.0) |
| ⩾10 years | 91 | 76 (84) | 2.6 (1.4 to 4.9) | 2.5 (1.3 to 4.7) | 2.1 (1.1 to 4.1) |
| Knee pain in the past 12 months | |||||
| <7 days | 56 | 28 (50) | 1 | 1 | 1 |
| 1–4 weeks | 92 | 56 (61) | 1.6 (0.8 to 3.0) | 1.8 (0.9 to 3.6) | 1.8 (0.9 to 3.8) |
| 1–<3 months | 109 | 69 (63) | 1.7 (0.9, 3.3) | 1.8 (0.9, 3.6) | 1.9 (0.9 to 3.8) |
| ⩾3 months | 435 | 324 (74) | 2.9 (1.7 to 5.1) | 2.7 (1.5 to 5.0) | 2.7 (1.4 to 4.9) |
| Days of knee pain in the past 6 months | |||||
| 1–30 | 352 | 226 (64) | 1 | 1 | 1 |
| 31–89 | 192 | 125 (65) | 1.0 (0.7 to 1.5) | 1.0 (0.7 to 1.5) | 0.9 (0.6 to 1.3) |
| ⩾90 | 201 | 158 (79) | 2.1 (1.4 to 3.1) | 1.9 (1.2 to 2.8) | 1.6 (1.0 to 2.4) |
| Pain, aching or stiffness in the past month | |||||
| No days | 37 | 14 (38) | 1 | 1 | 1 |
| Few days | 176 | 120 (68) | 3.5 (1.7 to 7.4) | 4.0 (1.8 to 8.9) | 3.8 (1.7 to 8.4) |
| Some days | 192 | 123 (64) | 2.9 (1.4 to 6.1) | 3.2 (1.5 to 6.9) | 2.9 (1.3 to 6.3) |
| Most days | 218 | 153 (70) | 3.9 (1.9 to 8.0) | 4.1 (1.9 to 8.8) | 3.5 (1.6 to 7.6) |
| All days | 122 | 99 (81) | 7.1 (3.2 to 15.8) | 6.9 (3.0 to 16.1) | 5.6 (2.4 to 13.2) |
BMI, body mass index; ROA, radiographic osteoarthritis.
When pain or aching or stiffness in the last month is dichotomised for most/all days with reference to no/few/some, the age‐sex‐adjusted OR (95% CI) is 1.6 (1.1 to 2.1).
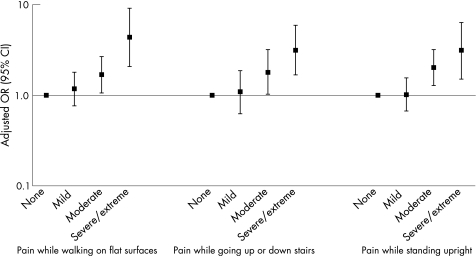
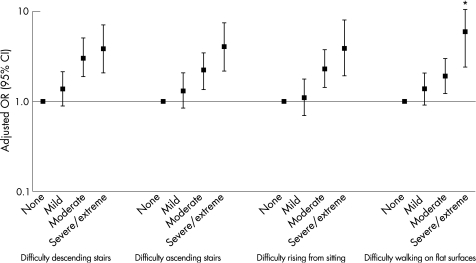
Association between WOMAC and radiographic osteoarthritis
We found evidence of a trend of stronger associations with worsening WOMAC scores (figs 1, 2; table 2). Higher WOMAC scores for pain severity, stiffness and physical functioning were more strongly linked to radiographic osteoarthritis (age‐sex‐adjusted OR (95% CI) for highest v lowest category: 3.7 (2.0 to 6.7), 3.0 (2.0 to 4.6) and 2.8 (1.6 to 5.0), respectively). The relationship between radiographic osteoarthritis and pain was evident in all five individual pain items of the WOMAC scale. Trends of association were observed in all items, but weight‐bearing activities were more strongly associated with radiographic osteoarthritis, pain while walking on a flat surface being the strongest (severe/extreme v none: OR 4.3, 95% CI 2.1 to 9.1). Similar trends of association were evident for individual WOMAC items related to stiffness and physical functioning.
Figure 1 Odds of radiographic knee osteoarthritis for individual pain items on the Western Ontario and McMaster Universities score.
Figure 2 Odds of radiographic osteoarthritis for individual function items on the Western Ontario and McMaster Universities score. *Upper 95% CI = 14.52.
Table 2 Occurrence of radiographic knee osteoarthritis in relation to Western Ontario and McMaster Universities subscale scores.
| Variable | Total | Patients with ROA, n (%) | OR (95% CI) | Adjusted OR (95% CI) | |
|---|---|---|---|---|---|
| For age and sex | For age, sex and BMI | ||||
| Pain subscale score (0–20) | |||||
| 0–2 | 154 | 91 (59) | 1 | 1 | 1 |
| 3–4 | 102 | 65 (64) | 1.2 (0.7 to 2.0) | 1.1 (0.6 to 1.9) | 1.1 (0.7 to 2.0) |
| 5–6 | 116 | 75 (65) | 1.3 (0.8 to 2.1) | 1.0 (0.6 to 1.8) | 1.0 (0.6 to 1.7) |
| 7–10 | 193 | 142 (74) | 1.9 (1.2 to 3.0) | 1.5 (0.9 to 2.4) | 1.4 (0.9 to 2.3) |
| 11–20 | 124 | 105 (85) | 3.8 (2.1 to 6.9) | 3.7 (2.0 to 6.7) | 2.8 (1.5 to 5.3) |
| Stiffness subscale score (0–8) | |||||
| 0–1 | 184 | 100 (54) | 1 | 1 | 1 |
| 2–3 | 232 | 162 (70) | 1.9 (1.3 to 2.9) | 1.0 (1.3 to 3.0) | 1.7 (1.1 to 2.7) |
| 4–10 | 278 | 219 (79) | 3.1 (2.1 to 4.7) | 2.0 (2.0 to 4.6) | 2.5 (1.6 to 3.9) |
| Physical functioning subscale score (0–68) | |||||
| 0–5 | 135 | 74 (55) | 1 | 1 | 1 |
| 6–15 | 150 | 87 (58) | 1.1 (0.7 to 1.8) | 1.0 (0.6 to 1.7) | 1.0 (0.6 to 1.6) |
| 16–24 | 135 | 101 (75) | 2.5 (1.5 to 4.1) | 2.0 (1.2 to 3.5) | 1.8 (1.0 to 3.1) |
| 25–35 | 137 | 110 (80) | 3.4 (2.0 to 5.8) | 2.9 (1.7 to 5.2) | 2.6 (1.4 to 4.6) |
| 35–68 | 134 | 106 (79) | 3.1 (1.8 to 5.3) | 2.8 (1.6 to 5.0) | 2.2 (1.2 to 3.9) |
BMI, body mass index; ROA, radiographic knee osteoarthritis.
The patterns of association with radiographic osteoarthritis were similar for both morning stiffness and stiffness after sitting, lying or resting during the day. Individual physical functioning items involving weight‐bearing mobility showed the strongest association with radiographic osteoarthritis. OR adjusted for age and sex (95% CI), severe/extreme v none of radiographic knee osteoarthritis for individual physical function items of the WOMAC were as follows: walking on a flat surface 5.9 (2.4 to 14.5), ascending stairs 4.0 (2.2 to 7.4), rising from sitting 3.9 (1.9 to 7.8) and descending stairs 3.8 (2.1 to 7.0).
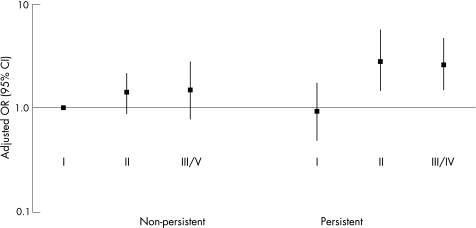
Association between combined pain persistence or global severity and radiographic osteoarthritis
The prevalence of radiographic osteoarthritis was significantly increased only when pain was persistent and of high intensity (⩾grade II) when compared with the reference group with non‐persistent, low‐intensity pain (OR adjusted for age and sex, 95% CI for P II v NP I 2.8 (1.4 to 5.6), fig 3). Pain that was non‐persistent, even if severe and highly disabling, was not associated with a significantly higher prevalence of radiographic osteoarthritis.
Figure 3 Occurrence of radiographic knee osteoarthrits in relation to combined persistence and graded chronic pain scale classification.
Discussion
Older people reporting knee pain will more likely than not have definite evidence of radiographic osteoarthritis irrespective of the nature, frequency and severity of their symptoms and disability. In this study, the proportion of patients with radiographic osteoarthritis in their index knee was 68%, slightly higher than that reported in previous population‐based studies.34 As this study was not a comparison with asymptomatic individuals, we cannot state how much of this radiographic osteoarthritis would have been present anyway. However, it is the observed trend of radiographic knee osteoarthritis and pain and disability within individuals with symptoms that is the main contribution of this study.
Whether based on persistence of knee pain within a given time, the severity of pain and stiffness, or the degree of difficulty with locomotor activities attributed to the knee problem, there is a clear increase in the prevalence of definite radiographic osteoarthritis across categories of these characteristics. These trends were consistent across each of the measures used in this study. They were steeper for pain severity and degree of difficulty, with items of weight‐bearing mobility such as walking on flat surfaces and climbing stairs, consistent with the findings of Odding et al15 and LaValley et al,33 and persisted after adjusting for age, sex and BMI. Generally, only those with the most persistent pain and those scoring in the severe/extreme categories for pain and functional difficulty on the WOMAC scale, had significantly higher odds of radiographic osteoarthritis compared with those in the least persistent or least severe categories.
When combining persistence and severity, a threshold effect was apparent for those with persistent, high‐intensity pain and accompanying interference with activities. This was based on an existing method of classifying chronic pain,35 but the same effect was found when the item on “symptom days in the past month” was combined with WOMAC pain quintiles (data not shown).
The emphasis in this paper is on grading pain and disability, and relating this to a particular definition of osteoarthritis. Whether the isolated osteophyte of K&L's grade 2 should be labelled as osteoarthritis or not is currently being debated. We repeated the analysis of the association of overall WOMAC scores after redefining radiographic osteoarthritis as K&L ⩾grade 3 (which requires some joint space narrowing in addition to osteophytosis) and using ⩽grade 2 as the comparison group. The associations were similar but stronger for pain, stiffness and physical function subscales (OR adjusted for age and sex, 95% CI for highest v lowest quintile of WOMAC: 4.4 (2.6 to 7.8), 3.0 (2.1 to 5.0) and 4.1 (2.3 to 7.3), respectively). This indicates that, however the label of osteoarthritis is applied, there is a strong trend of association with increasing levels of pain and disability and the presence of radiographic osteoarthritis.
The strengths of our study include the use of
three radiographic views, the posteroanterior, skyline and lateral, to capture the maximum number of individuals with radiographic osteoarthritis;
recommended measures of pain and function such as the WOMAC scale19;
the graded chronic pain status as a means of classifying combined pain and disability severity35; and
a sampling frame that identified people with a wide range of severity and duration of knee pain, unselected for their use of healthcare.
Our study provides partial corroboration for the clinical description of osteoarthritis as typically involving more longstanding and persistent pain, worse on weight‐bearing activities.36,37 These results suggest that radiographic changes are more common in those with more severe symptoms. In support of this, the pattern of associations was generally consistent across measures, a trend of increasing strength of association with severity was often evident, and in some cases the association was strong. Unlike previous studies, we chose not to adjust for factors such as quadriceps weakness, anxiety or depression in the belief that these may not be truly extraneous confounders but form part of the mechanism of association or are predominantly consequences of pain and disability. When we adjusted for BMI in addition to age and sex, there was little change in the ORs and most results remained significant.
Conclusion
Our study on structure–pain associations in individuals with symptoms has found a relatively consistent relationship between increasing persistence and severity of pain and disability and the prevalence of radiographic osteoarthritis. A threshold effect in the prevalence of radiographic osteoarthritis was evident at the point when pain became persistent and of high intensity. This study has essentially imaged more of the knee joint with multiple views than in many previous studies, and this may have contributed to the increased associations with pain and disability compared with these earlier studies. The next logical step would be to consider the severity and compartmental involvement of radiographic osteoarthritis and its relationship with symptoms, described in the recent publication from Szebenyi et al.38
We have not studied people free of pain, and therefore have not dealt with the broader question of whether radiographic osteoarthritis causes knee pain. However, we have found that, in individuals with symptoms, the worse their pain and disability, the more likely they are to have radiographic osteoarthritis.
The associations we have found are stronger than those previously observed. This has important implications for our understanding of the contribution of regional osteoarthritis pathology to the biopsychosocial model of chronic joint pain in older people.
Acknowledgements
This study is supported financially by a programme grant awarded by the Medical Research Council, UK (Grant Code G9900220) and by Support for Science funding secured by North Staffordshire Primary Care Research Consortium for NHS service support costs.
We thank Dr Krysia Dziedzic, June Handy, Charlotte Clements, Jonathan Hill, Helen Myers, Dr Ross Wilkie and Dr Laurence Wood for their contribution towards aspects of the conception and design of the study and to the acquisition of data and comments during the drafting of the manuscript; Dr Jacqueline Saklatvala, Carole Jackson, Julia Myatt, Janet Wisher, Sue Stoker, Sandra Yates, Kath Hickson from the Department of Radiography, Haywood Hospital, for acquisition of data; and Professor Chris Buckland‐Wright for advice and training on the radiographic techniques. We also thank the administrative and health informatics staff at Keele University's Primary Care Sciences Research Centre, and the staff and patients of the participating general practices.
Abbreviations
BMI - body mass index
K&L - Kellgren and Lawrence
WOMAC Score - Western Ontario and McMaster Universities Score
Footnotes
Competing interests: None.
References
- 1.Cobb S, Merchant W R, Rubin T. The relation of symptoms to osteoarthritis. J Chronic Dis 19575197–204. [DOI] [PubMed] [Google Scholar]
- 2.Cicuttini F M, Baker J, Hart D J, Spector T D. Association of pain with radiological changes in different compartments and views of the knee joint. Osteoarthritis Cartilage 19964143–147. [DOI] [PubMed] [Google Scholar]
- 3.Hannan M T, Felson D T, Pincus T. Analysis of discordance between radiographic change and knee pain in osteoarthritis of the knee. J Rheumatol 2000271513–1517. [PubMed] [Google Scholar]
- 4.Dieppe P A. Relationship between symptoms and structural change in osteoarthritis. What are the important targets for osteoarthritis therapy? J Rheumatol 200431(Suppl 70)50–53. [PubMed] [Google Scholar]
- 5.Kellgren J H, Lawrence J S. Rheumatism in miners. Part II: x‐ray study. Br J Ind Med 19529197–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lawrence J S, Bremner J M, Bier F. Osteo‐arthrosis. Prevalence in the population and relationship between symptoms and x‐ray changes. Ann Rheum Dis 1966251–24. [PMC free article] [PubMed] [Google Scholar]
- 7.Felson D T, Naimark A, Anderson J, Kazis L, Castelli W, Meenan R F. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum 198730914–918. [DOI] [PubMed] [Google Scholar]
- 8.Davis M A, Ettinger W H, Neuhaus J M, Barclay J D, Segal M R. Correlates of knee pain among US adults with and without radiographic knee osteoarthritis. J Rheumatol 1992191943–1949. [PubMed] [Google Scholar]
- 9.Lethbridge‐Cejku M, Scott W W, Jr, Reichle R, Ettinger W H, Zonderman A, Costa P.et al Association of radiographic features of osteoarthritis of the knee with knee pain: data from the Baltimore Longitudinal Study of Aging. Arthritis Care Res 19958182–188. [DOI] [PubMed] [Google Scholar]
- 10.Lanyon P, O'Reilly S, Jones A, Doherty M. Radiographic assessment of symptomatic knee osteoarthritis in the community: definitions and normal joint space. Ann Rheum Dis 199857595–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McAlindon T E, Cooper C, Kirwan J R, Dieppe P A. Determinants of disability in osteoarthritis of the knee. Ann Rheum Dis 199352258–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jordan J M, Luta G, Renner J B, Linder G F, Dragomir A, Hochberg M C.et al Self‐reported functional status in osteoarthritis of the knee in a rural southern community: the role of sociodemographic factors, obesity, and knee pain. Arthritis Care Res 19969273–278. [DOI] [PubMed] [Google Scholar]
- 13.O'Reilly S C, Jones A, Muir K R, Doherty M. Quadriceps weakness in knee osteoarthritis: the effect on pain and disability. Ann Rheum Dis 199857588–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jordan J, Luta G, Renner J, Dragomir A, Hochberg M, Fryer J. Knee pain and knee osteoarthritis severity in self‐reported task specific disability: the Johnston County Osteoarthritis Project. J Rheumatol 1997241344–1349. [PubMed] [Google Scholar]
- 15.Odding E, Valkenburg H A, Algra D, Vandenouweland F A, Grobbee D E, Hofman A. Associations of radiological osteoarthritis of the hip and knee with locomotor disability in the Rotterdam Study. Ann Rheum Dis 199857203–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Summers M N, Haley W E, Reveille J D, Alarcon G S. Radiographic assessment and psychological variables as predictors of pain and functional impairment in osteoarthritis of the knee or hip. Arthritis Rheum 198831204–209. [DOI] [PubMed] [Google Scholar]
- 17.Salaffi F, Cavalieri F, Nolli M, Ferraccioli G. Analysis of disability in knee osteoarthritis. Relationship with age and psychological variables but not with radiographic score. J Rheumatol 1991181581–1586. [PubMed] [Google Scholar]
- 18.van Baar M E, Dekker J, Lemmens J A M, Oostendorp R A B, Bijlsma J W J. Pain and disability in patients with osteoarthritis of hip or knee: the relationship with articular, kinesiological, and psychological characteristics. J Rheumatol 199825125–133. [PubMed] [Google Scholar]
- 19.Creamer P, Lethbridge‐Cejku M, Hochberg M C. Determinants of pain severity in knee osteoarthritis: effect of demographic and psychosocial variables using 3 pain measures. J Rheumatol 1999261785–1792. [PubMed] [Google Scholar]
- 20.Creamer P. Current perspectives on the clinical presentation of joint pain in human OA. In: Chadwick DJ, Goode J, eds. Osteoarthritic joint pain. Novartis Foundation Symposium 260. Chichester: Wiley, 200364–78. [PubMed]
- 21.Peat G, Thomas E, Handy J, Wood L, Dziedzic K, Myers H.et al The Knee Clinical Assessment Study—CAS(K). A prospective study of knee pain and knee osteoarthritis in the general population. BMC Musculoskelet Disord 200454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.de Vet H C W, Heymans M W, Dunn K D, Pope D P, van der Beek A J, Macfarlane G J.et al Episodes of low back pain. A proposal for uniform definitions to be used in research. Spine 2002272409–2416. [DOI] [PubMed] [Google Scholar]
- 23.Jinks C, Lewis M, Ong B N, Croft P. A brief screening tool for knee pain in primary care I validity and reliability. Rheumatology 200140528–536. [DOI] [PubMed] [Google Scholar]
- 24.Von Korff M, Ormel J, Keefe F J, Dworkin S F. Grading the severity of chronic pain. Pain 199250133–149. [DOI] [PubMed] [Google Scholar]
- 25.Altman R.et al Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Arthritis Rheum 1986291039–1049. [DOI] [PubMed] [Google Scholar]
- 26.Bellamy N.WOMAC osteoarthritis index. A user's guide. Ontario: London Health Services Centre, 1996
- 27.Jinks C, Jordan K, Croft P. Measuring the population impact of knee pain and disability with the Western Ontario and McMaster Universities osteoarthritis index (WOMAC). Pain 200210055–64. [DOI] [PubMed] [Google Scholar]
- 28.Smith B H, Penny K I, Purves A M, Munro C, Wilson B, Grimshaw J.et al The Chronic Pain Grade questionnaire: validation and reliability in postal research. Pain 199771141–147. [DOI] [PubMed] [Google Scholar]
- 29.Penny K I, Purves A M, Smith B H, Chambers W A, Smith W C. Relationship between the chronic pain grade and measures of physical, social and psychological well‐being. Pain 199979275–279. [DOI] [PubMed] [Google Scholar]
- 30.Buckland‐Wright C, Wolfe F, Ward R J, Flowers N, Hayne C. Substantial superiority of semiflexed (MTP) views in knee osteoarthritis: a comparative radiographic study, without fluroscopy, of standing extended, semiflexed (MTP), and Schuss views. J Rheumatol 1999262664–2674. [PubMed] [Google Scholar]
- 31.Lawrence J S.Rheumatism in populations. London: Heinemann, 197799–100.
- 32.Burnett S, Hart D, Cooper C, Spector T.A radiographic atlas of osteoarthritis. London: Springer, 1994
- 33.LaValley M, McAlindon T E, Evans S, Chaisson C E, Felson D T. Problems in the development and validation of questionnaire‐based screening instruments for ascertaining cases with symptomatic knee osteoarthritis: the Framingham Study. Arthritis Rheum 2001441105–1113. [DOI] [PubMed] [Google Scholar]
- 34.Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis 20016091–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Von Korff M, Jensen M P, Karoly P. Assessing global pain severity by self‐report in clinical and health services research. Spine 2000253140–3151. [DOI] [PubMed] [Google Scholar]
- 36.Primary Care Rheumatology Society Knee osteoarthritis: management options 1999. http://www.eguidelines.co.uk
- 37.Institute for Clinical Systems Improvement Health care guideline: diagnosis and treatment of adult degenerative joint disease (DJD) of the knee. 8th edn. 2004. http://www.icsi.org/index.asp (accessed 30 Oct 2006)
- 38.Szebenyi B, Hollander A P, Dieppe P, Quilty B, Duddy J, Clarke S.et al Associations between pain, function, and radiographic features in osteoarthritis of the knee. Arthritis Rheum 200654230–235. [DOI] [PubMed] [Google Scholar]