Abstract
We developed a highly sensitive and specific assay for the rapid detection of smallpox virus DNA on both the Smart Cycler and LightCycler platforms. The assay is based on TaqMan chemistry with the orthopoxvirus hemagglutinin gene used as the target sequence. With genomic DNA purified from variola virus Bangladesh 1975, the limit of detection was estimated to be approximately 25 copies on both machines. The assay was evaluated in a blinded study with 322 coded samples that included genomic DNA from 48 different isolates of variola virus; 25 different strains and isolates of camelpox, cowpox, ectromelia, gerbilpox, herpes, monkeypox, myxoma, rabbitpox, raccoonpox, skunkpox, vaccinia, and varicella-zoster viruses; and two rickettsial species at concentrations mostly ranging from 100 fg/μl to 1 ng/μl. Contained within those 322 samples were variola virus DNA, obtained from purified viral preparations, at concentrations of 1 fg/μl to 1 ng/μl. On the Smart Cycler platform, 2 samples with false-positive results were detected among the 116 samples not containing variola virus tested; i.e., the overall specificity of the assay was 98.3%. On the LightCycler platform, five samples with false-positive results were detected (overall specificity, 95.7%). Of the 206 samples that contained variola virus DNA ranging in concentrations from 100 fg/μl to 1 ng/μl, 8 samples were considered negative on the Smart Cycler platform and 1 sample was considered negative on the LightCycler platform. Thus, the clinical sensitivities were 96.1% for the Smart Cycler instrument and 99.5% for the LightCycler instrument. The vast majority of these samples were derived from virus-infected cell cultures and variola virus-infected tissues; thus, the DNA material contained both viral DNA and cellular DNA. Of the 43 samples that contained purified variola virus DNA ranging in concentration from 1 fg/μl to 1 ng/μl, the assay correctly detected the virus in all 43 samples on both the Smart Cycler and the LightCycler platforms. The assay may be useful for the early detection of smallpox virus infections should such infections occur as a result of a deliberate or an accidental recurrence.
Smallpox, once a devastating disease, was eradicated in 1977, but stocks of variola virus still exist. Amid serious concerns that the virus may emerge as a biological weapon, efforts are mounting to replenish the vaccine supply and develop new drugs and diagnostic methods for the early detection of infection. DNA-based techniques have been developed for the early detection and identification of several orthopoxviruses. These methods include PCR, nucleic acid sequencing, and restriction fragment length polymorphism analysis (3, 14, 15, 16, 17, 21, 22, 23). Of those methods, sequencing provides the highest level of specificity for species or strain identification, but the sequencing techniques available at present are not yet practical as rapid diagnostic tools in most laboratories. Restriction fragment length polymorphism analysis also provides a high level of specificity, and when it is combined with PCR amplification, it can offer a high level of sensitivity; however, it is not yet suitable for rapid diagnosis, as it involves multiple highly technical steps and may not be appropriate for all types of samples. One of the most promising approaches for rapid and sensitive diagnosis is the real-time 5′ nuclease PCR assay, also known as the TaqMan assay. Previously, we reported on the selection of the gene for the hemagglutinin, a gene that distinguishes the genus Orthopoxvirus from other poxvirus genera, as a suitable sequence target for genus- and species-specific PCR tests (1, 2, 10, 11) and the potential utility of 5′ nuclease assays for the diagnosis of orthopoxvirus infections (10, 11). Here, we report on the development of a real-time TaqMan assay based on the hemagglutinin gene for the sensitive and specific detection of variola virus, the causative agent of smallpox, on portable real-time detection devices: the Smart Cycler instrument (Cepheid, Sunnyvale, Calif.) and the LightCycler instrument (Roche Molecular Systems, Indianapolis, Ind.).
MATERIALS AND METHODS
Viruses and DNA preparation.
The orthopoxviruses and controls used in the study (Table 1) included 48 isolates of variola virus; 25 different strains and isolates of camelpox, cowpox, ectromelia, gerbilpox, herpes, monkeypox, myxoma, rabbitpox, raccoonpox, skunkpox, vaccinia, and varicella-zoster viruses; and two rickettsial species. The origins, propagation, and harvesting procedures for these viruses are documented elsewhere (23). Variola virus infectious titers were determined by the plaque assay and were between 108 and 1010 PFU/ml. DNA was extracted from virus-infected cells, virions, and scabs by using the Aquapure DNA kit (Bio-Rad). Briefly, 100 μl of the cell lysate or scab suspensions was mixed with 500 μl of Aquapure lysis buffer, the mixture was incubated at 55°C for 4 to 12 h and cooled to 37°C, and 5 μl (12 μg) of Aquapure RNase solution was added. The mixture was incubated at 37°C for 5 min, and then 200 μl of Aquapure protein precipitation solution was added and the components were mixed by vortexing. The samples were centrifuged at 13,000 × g for 20 min, the supernatants were transferred into sterile microcentrifuge tubes, 600 μl of isopropanol was added, and the DNA was precipitated by centrifugation at 13,000 × g for 5 min. The DNA was washed once with 70% alcohol, suspended in 50 μl of Aquapure DNA hydration buffer, and stored at −20°C until use. Prior experiments demonstrated that the material was noninfectious after 60 min of incubation at 55°C in Aquapure lysis buffer.
TABLE 1.
List of orthopoxviruses and other viral and rickettsial species tested in a blinded study
| Species or sample | Strain, isolate, or source |
|---|---|
| Camelpox virus | 78-I-903 |
| Camelpox virus | LLCb |
| Camelpox virus | 2379 |
| Cowpox virus | Brighton |
| Ectromelia virus | Moscow |
| Gerbilpox virus | CDCc |
| Herpes simplex virus type 1 | HFEMd |
| Herpes simplex virus type 1 | Justin |
| Herpes simplex virus type 2 | v02 |
| Human genomic DNA | supT |
| Monkey genomic DNA | BSC40 |
| Monkeypox virus | Zaire 79-0005 |
| Monkeypox virus | 79-0266 |
| Monkeypox virus | v96-I-16 |
| Myxoma virus | CDC |
| Rabbitpox virus | CDC |
| Raccoonpox virus | CDC |
| Rickettsia conorii | CDC |
| Rickettsia akari | CDC |
| Skunkpox virus | CDC |
| Vaccinia virus | IHDWe |
| Vaccinia virus | Lister |
| Vaccinia virus | Wyeth/Dryvax |
| Vaccinia virus | Wyeth clone |
| Vaccinia virus | pGS68-9-v1-1-1 |
| Varicella-zoster virus | OKA |
| Varicella-zoster virus | Webster |
| Water | NAa |
| Variola virus | 102 |
| Variola virus | 103 |
| Variola virus | 7124 |
| Variola virus | 7125 |
| Variola virus | 66-39 |
| Variola virus | 68-59 |
| Variola virus | 68-258 |
| Variola virus | 70-222 |
| Variola virus | 70-228 |
| Variola virus | 72-119 |
| Variola virus | 72-143 |
| Variola virus | 73-175 |
| Variola virus | 73-225 |
| Variola virus | 77-1252 |
| Variola virus | 77-1605 |
| Variola virus | 77-227 |
| Variola virus | Afghanistan Variolator 4 |
| Variola virus | Bombay |
| Variola virus | Brazil Garcia |
| Variola virus | BSH |
| Variola virus | Butler |
| Variola virus | Congo |
| Variola virus | Ethiopia 17 |
| Variola virus | Harper |
| Variola virus | Harvey |
| Variola virus | Heidelberg |
| Variola virus | Higgins |
| Variola virus | Hinton |
| Variola virus | Horn |
| Variola virus | Iran |
| Variola virus | Juba |
| Variola virus | K1629 |
| Variola virus | Kali Mathu |
| Variola virus | Kembula |
| Variola virus | Minn. 124 |
| Variola virus | MS Lee |
| Variola virus | Nepal |
| Variola virus | New Delhi |
| Variola virus | Nigeria Kudano |
| Variola virus | Nur Islam |
| Variola virus | Rafiq Lahore |
| Variola virus | Rumbec |
| Variola virus | Shahzaman |
| Variola virus | Solaiman |
| Variola virus | Stillwell |
| Variola virus | Yamada |
NA, not applicable.
LLCMK2 monkey kidney cell passage of Somalia camelpox virus.
CDC, Centers for Disease Control and Prevention.
HF strain.
IHDW, International Health Department.
PCR primers, target sequences, and fluorogenic probe.
The sequences of primers OPXJ7R3U (5′-TCATCTGGAGAATCCACAACA-3′) and OPXJ7R3L (5′-CATCATTGGCGGTTGATTTA-3′) and probe VARJ7R3P (5′-CAAGACGTCGGGACCAATTACTAATA-3′) were selected from the sequence of the hemagglutinin gene (open reading frame J7R; GenBank accession no. L22579) with the aid of Oligo software (version 5.0; National Biosciences). The primers were synthesized by using standard phosphoramidite chemistry with an ABI 394 DNA/RNA synthesizer (Applied Biosystems). The TaqMan probe was synthesized by Perkin-Elmer Biosystems (Foster City, Calif.) and contained 6-carboxyfluorescein at the 5′ end and 6-carboxytetramethylrhodamine and a phosphate at the 3′ end.
Cloning and sequencing of variola virus J7R fragment.
A fragment of 942 bp which contained the hemagglutinin gene was amplified by PCR from the J7R open reading frame of variola virus Bangladesh 1975 genomic DNA. The fragment was cloned into the pCR-Script Amp SK(+) vector (Stratagene, La Jolla, Calif.). Briefly, the amplified fragment was purified by ammonium acetate and ethanol precipitation and resuspended in 20 μl of TE (Tris, EDTA) buffer, and 2 to 4 μl of the purified DNA was ligated to 10 ng of the pCR-Script Amp SK(+) vector with T4 DNA ligase. A portion of the ligation reaction (2 μl) was used to transform Epicurian Coli XII-Blue MRF′ Kan electroporation-competent cells. The transformed cells were incubated in SOC medium for 1 h at 37°C and then plated on Luria-Bertani agar plates containing ampicillin, isopropyl-β-d-thiogalactopyranoside, and 5-bromo-4-chloro-3-indolyl-β-d-galactopyranoside and incubated at 37°C overnight. Five to 10 transformed colonies were selected, and plasmid preparations were made by using a Qiagen plasmid DNA kit.
5′ nuclease PCR assay.
The 5′ nuclease PCR assay and amplifications conditions were optimized according to the standard protocols used in our laboratory by adjusting the primer, probe, and MgCl2 concentrations as well as the thermal cycling temperatures and duration. The reactions were carried out in 30-μl volumes for the Smart Cycler instrument and 20-μl volumes for the LightCycler instrument. Each reaction mixture contained PCR buffer (50 mM Tris [pH 8.3], 25 μg of bovine serum albumin per ml), 0.2 mM deoxynucleoside triphosphate mixture, 0.4 μM each primer, 5 mM MgCl2 for the Smart Cycler instrument or 7 mM MgCl2 for the LightCycler instrument, 170 nM TaqMan probe for the Smart Cycler instrument or 75 nM TaqMan probe for the LightCycler instrument, 1.35 U of Platinum TaqDNA polymerase (Invitrogen, Carlsbad, Calif.) for the Smart Cycler instrument or 0.8 U of Platinum TaqDNA polymerase for the LightCycler instrument, and 5 μl of template DNA. Thermal cycling for the Smart Cycler instrument was performed as follows: 1 cycle at 95°C for 2 min, followed by 45 cycles of 95°C for 10 s and 60°C for 45 s. For the Smart Cycler instrument, data acquisition and analysis were done by using Cepheid Smart Cycler software (version 1.2d). For the LightCycler instrument, thermal cycling was performed as follows: 2 min at 95°C, followed by 45 cycles of 95°C for 1 s and 60°C for 20 s. Each capillary reaction tube was read in channel 1 (F1) at a gain setting of 16, with a fluorescence reading taken at the end of each 60°C step. For the LightCycler instrument, data were analyzed by using the LightCycler Data Analysis software (version 1.1), and the results were reviewed and interpreted before a positive or a negative result was called. All reactions that were performed during testing of the coded samples included at least one positive control that contained 5 fg (about 25 copies) of purified variola virus Bangladesh 1975 genomic DNA and one no-template control. The positive control with 5 fg of virus DNA in each run established the threshold cycle (Ct) value for positivity. Samples yielding Ct values which marginally exceeded this threshold value were flagged for retesting. If the Ct value was confirmed to exceed the threshold value after retesting, such a sample was considered negative (i.e., the sample contained <25 gene copies). Calculations of sensitivity and specificity were determined as follows: percent sensitivity = [TP/(TP + FN)] × 100 and percent specificity = [TN/(TN + FP)] × 100, where TP is the number of true-positive samples, FN is the number of false-negative samples, TN is the number of true-negative samples, and FP is the number of false-positive samples.
RESULTS
The designs of the PCR primers and the TaqMan probe as well as the optimization of the TaqMan reactions and the cycling conditions were as described in Applied Biosystems protocol 04304449. Plasmid J7R was constructed to facilitate initial evaluation and optimization of the assay. The cloned J7R insert was sequenced by standard dye terminator cycle sequencing, and its sequence was 100% homologous to the published sequence of variola virus Bangladesh 1975 (GenBank accession no. L22579) over 942 nucleotides (data not shown).
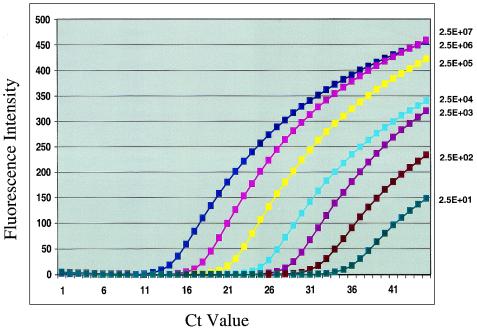
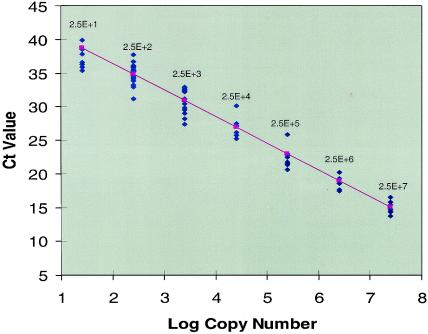
The limit of detection (LOD) of the assay on the SmartCycler instrument was determined from serial dilutions of plasmid J7R DNA as well as genomic DNA purified from variola virions. The assay reproducibly detected 0.05 fg of plasmid DNA and 5 fg of genomic DNA, which represents approximately 12 and 25 copies of the hemagglutinin genes from plasmid and genomic DNAs, respectively. The data from both plasmid and genomic DNA LOD experiments showed a linear correlation, with a dynamic range of 7 orders of magnitude representing approximately 25 to 25,000,000 copies. Figure 1 shows the assay's LOD, and Fig. 2 shows the dynamic range obtained with purified variola virus genomic DNA. Similar results were obtained on the LightCycler instrument (data not shown).
FIG. 1.
LOD of the assay expressed in copy numbers. Tenfold serial dilutions of purified variola virus genomic DNA (1 fg/μl to 1 ng/μl) were tested with TaqMan probe VARJ7R3P on the Smart Cycler instrument. Each curve represents the mean fluorescence value of five different runs. Since 5 μl was used for each concentration in each run, the numbers of copies are represented as 2.5 × 101 (2.5E + 01), 2.5 × 102, 2.5× 103, 2.5 × 104, 2.5 × 105, 2.5 × 106 and 2.5 × 107.
FIG. 2.
Dynamic range of the assay. Regression analysis was performed on the Ct against log copy numbers. A total of 83 samples contained purified variola virus genomic DNA ranging in concentrations from 1 fg/μl (25 copies) to 10 ng/μl (25 × 106 copies). The actual and predicted values are shown with the linearity coefficient (r2 = 0.95; significance F = 6.7E-56).
The assay was evaluated with a test panel that included 322 coded samples of genomic DNA from 48 different isolates of variola virus; 25 different strains and isolates of camelpox, cowpox, ectromelia, gerbilpox, herpes, monkeypox, myxoma, rabbitpox, raccoonpox, skunkpox, vaccinia, and varicella-zoster viruses; and two rickettsial species (Table 1). The concentrations of the DNAs used in the test panel ranged from 100 fg/μl to 1 ng/μl and included total viral and cellular DNAs from cell lysates and crust material as well as purified viral DNAs. Table 2 shows a summary of the results of the blinded study obtained with the SmartCycler instrument and DNA samples that contained 100 fg to 1 ng of nucleic acids per μl. Two samples (containing cowpox virus and Rickettsia conorii) with false-positive results were detected among the 116 samples not containing variola virus; i.e., the overall specificity of the assay was 98.3% with the SmartCycler instrument. Five samples (containing cowpox, racoonpox, and ectromelia Moscow virus) with false-positive results were detected with the LightCycler instrument, resulting in an overall specificity of 95.8%. Of the 206 samples which contained DNA extracted from variola viral cell lysates or purified variola virus ranging in concentrations from 100 fg/μl to 1 ng/μl, 8 samples were considered negative with the Smart Cycler instrument, while 1 sample was considered negative with the LightCycler instrument. Thus, the clinical sensitivities were 96.1% for the SmartCycler instrument and 99.5% for the LightCycler instrument at an LOD of 25 copies.
TABLE 2.
Summary of the results of identification of variola virus DNA extracted from 48 isolates by using the VARJ7R3P TaqMan probe on the Smart Cycler instrumenta
| Species | No. of isolates | No. of samples positive/no. of samples tested |
|---|---|---|
| Camelpox virus | 3 | 0/11 |
| Cowpox virus | 1 | 1/8 |
| Monkeypox virus | 3 | 0/10 |
| Ectromelia virus | 1 | 0/8 |
| Gerbilpox virus | 1 | 0/8 |
| Herpes virus | 3 | 0/13 |
| Human DNA | 1 | 0/3 |
| Monkey DNA | 1 | 0/3 |
| Myxoma virus | 1 | 0/3 |
| Rabbitpox virus | 1 | 0/3 |
| Raccoonpox virus | 1 | 0/5b |
| Rickettsia spp. | 2 | 1/8c |
| Skunkpox virus | 1 | 0/3 |
| Vaccinia virus | 5 | 0/17 |
| Varicella-zoster virus | 2 | 0/8 |
| Variola virus | 48 | 198/206d |
| Water | NAe | 0/5 |
The DNA concentrations ranged from 1 fg/μl to 1 ng/μl for variola virus DNA and 100 fg/μl to 1 ng/μl for all other DNAs.
The highest concentration (1 ng/μl) was positive on the LightCycler instrument.
Rickettsiae spp. were negative on the LightCycler instrument.
The values on the LightCycler instrument were 205/206.
NA, not applicable.
DISCUSSION
Vaccination against smallpox was discontinued in the United States and elsewhere nearly two decades ago, after the disease was declared eradicated in 1979. Since then, there has been a significant increase in the world's population, with proportionally larger numbers of people now being fully or partially susceptible to smallpox virus infection. The fact that smallpox has been eradicated does not preclude the possibility of its recurrence as a natural or deliberate biological threat. Although smallpox eradication is considered among the greatest accomplishments in medical history, this achievement now renders the smallpox virus one of the most feared weapons in biological warfare or bioterrorism scenarios. Today, with the ever-growing sophistication of molecular microbiology and biotechnology, mass production of variola virus or genetically engineered analogs for use as biological weapons is not an inconceivable notion. It is therefore crucial that reliable diagnostic tests be developed for the early detection and confirmation of suspected smallpox disease as a first line of defense.
Several PCR-based methods for the identification of orthopoxviruses have been described (14, 17, 20, 21, 22, 23). Those methods relied on analysis of the sizes of the PCR products by agarose gel electrophoresis after restriction endonuclease digestion. Although those methods provided high degrees of specificity and allowed species differentiation and sometimes strain differentiation, they required laborious and time-consuming post-PCR processing. Newer approaches that use species-specific oligonucleotide hybridization on a microchip (12) and fluorescence resonance energy transfer probes on the LightCycler instrument (4) have also been described. Another approach, the 5′ nuclease PCR or the TaqMan assay, first developed by Holland et al. (9) and improved by Lee et al. (13), allows the simultaneous amplification and detection of nucleic acids in real time; and when the assay is combined with portable analytical platforms such as the Smart Cycler instrument or the LightCycler instrument, it can be readily deployed to field sites for use for rapid diagnostic testing. Previously, we reported on the implementation of the TaqMan assay and the fluorogenic PCR technology for the identification of orthopoxvirus as well as other biological threat agents (5, 6, 7, 8, 10, 11).
In this study, our assay's detection limit was evaluated with purified variola virus genomic DNA and plasmid J7R DNA. The detection limit with plasmid DNA was 0.05 fg, or approximately 12 gene copies. With variola virus genomic DNA, the detection limit was 5 fg, or approximately 25 genome copies.
When the assay was evaluated with 322 coded samples that included variola virus-infected cells and tissues, purified variola virus DNA, as well as the DNA of 25 other species and isolates of orthopoxviruses, herpes simplex virus, Rickettsia, myxoma virus, and varicella-zoster virus, the sensitivities of the assay were 96.1% with the Smart Cycler instrument and 99.5% with the LightCycler instrument. The specificities were 98.3% with the Smart Cycler instrument and 95.7% with the LightCycler instrument at an LOD of 25 copies. Only 2 of the 116 samples not containing variola virus were falsely positive with the Smart Cycler instrument, while 5 samples were false positive with the LightCycler instrument. Of the two samples with false-positive results with the Smart Cycler instrument, one contained cowpox virus and the other contained R. conorii. The samples with false-positive results with the LightCycler instrument contained cowpox, racoonpox, or ectromelia virus. Other samples, including samples containing vaccinia virus, herpes simplex virus type 1, and varicella-zoster virus, were initially found to be positive with the LightCycler Detector software program (Idaho Technologies). However, upon further inspection of the graphs for the samples, the Ct values for these samples were significantly higher than those for the positive control. When these samples were retested, they were clearly negative. We therefore concluded that these samples might have become contaminated during testing. None of these samples should cross-react with the VARJ7R3P probe, as the probe sequence is specific for variola virus under the conditions used, as evident from the lack of cross-reactivity with seven other samples containing cowpox virus, seven samples containing Rickettsia, and samples containing other ectromelia viruses. Moreover, the probe did not cross-react with any of the other 73 samples containing orthopoxviruses or 3 samples containing myxoma virus that were blindly tested, nor did it cross-react with any of the 13 samples containing herpes simplex virus or 8 samples containing varicella-zoster virus that were included. Furthermore, the primers and probe did not cross-react with any of 78 samples that contained the DNA of 54 different bacterial species (data not shown). It is therefore, possible that the false-positive reactions with these samples were due to sample contamination either during the independent preparation of the test panel or during the setup of the assay.
It is noteworthy that that the vast majority of these samples were derived from cell cultures and variola virus-infected tissues; thus, the DNA material contained both viral and cellular DNAs. Of 43 coded samples that contained purified variola virus DNA ranging in concentration from 1 fg/μl to 1 ng/μl, the assays with both machines correctly detected the viral DNA in all 43 samples. These results indicate that with freshly prepared purified genomic DNA, the detection limit of the assay is 5 fg, or about 25 copies, and that the viral DNA in the cell lysate and crust preparations may represent about 1% of the total DNA in these preparations.
In conclusion, this report demonstrates for the first time the specific, real-time identification of the smallpox virus, including 48 different isolates of variola virus obtained from clinical samples as well as virus-infected cell cultures. We selected the hemagglutinin gene as a target for specific differentiation because it is included in the terminal region of the genome, which is known to be more variable than the central region (2, 14, 18, 19, 22, 23). Other terminal regions in the genome, including the tumor necrosis factor receptor homolog and the A-type inclusion protein, can also be used as targets for species-specific identification (2). Since the assay was able to correctly identify 48 different isolates of variola virus, we conclude that the sequence from which the probe was designed is conserved within variola virus isolates.
Acknowledgments
We thank Jamie Blow, Brian Moore, Erik Henchal, and Kathy Kenyon (USAMRIID, Fort Detrick, Md.) for reviewing the manuscript and the staff of the Frederick Biomedical Supercomputing Center (Frederick, Md.) for providing computing support. We thank Miriam Laker, Danielle Chekaraou, and Richard Kline for preparing the variola virus and orthopoxvirus DNA samples used in this study. The Rickettsia, varicella virus, and herpesvirus DNAs were provided by the Viral and Rickettsia Zoonoses Branch and the Varicella and Herpes Virus Sections of the Division of Viral and Rickettsial Diseases of the Centers for Disease Control and Prevention.
The views and opinions contained in this report are those of the authors and should not be construed as an official U.S. Department of Defense or U.S. Department of Health and Human Services position, policy, or decision.
REFERENCES
- 1.Cavallero, K. F., and J. J. Esposito. 1992. Sequences of the raccoon poxvirus hemagglutinin protein. Virology 190:434-449. [DOI] [PubMed] [Google Scholar]
- 2.Esposito, J., and F. Fenner. 2002. Poxviruses, p. 2885-2921. In D. M. Knipe, P. M. Howley, D. E. Griffin, R. A. Lamb, M. A. Martin, B. Roizman, and S. E. Straus (ed.), Fields' virology, 4th ed. Lippincott Williams & Wilkins, Philadelphia, Pa.
- 3.Esposito, J. J., and J. C. Knight. 1985. Orthopoxvirus DNA: a comparison of restriction profiles and maps. Virology 143:230-251. [DOI] [PubMed] [Google Scholar]
- 4.Espy, M. J., F. R. Cockerill III, R. F. Meyer, M. D. Bowen, G. A. Poland, T. L. Hadfield, and T. F. Smith. 2002. Detection of smallpox virus DNA by LightCycler PCR. J. Clin. Microbiol. 40:1985-1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Henchal, E. A., and M. S. Ibrahim. 2000. Evaluation of polymerase chain reaction assays for identifying biological agents, p. 239-249. In P. J. Stoppa and M. A. Bartoszcze (ed.), Rapid methods for analysis of biological materials in the environment. Kluwer Academic Publishers, Dordrecht, The Netherlands.
- 6.Higgins, J. A., J. W. Ezzell, B. J. Hinnebusch, M. Shipley, E. A. Henchal, and M. S. Ibrahim. 1998. A 5′ nuclease assay to detect Yersinia pestis. J. Clin. Microbiol. 6:2284-2288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Higgins, J. A., Z. Hubalek, J. Halouzka, K. L. Elkins, A. Sjostedt, M. Shipley, and M. S. Ibrahim. 2000. Detection of Francisella tularensis in infected mammals and vectors using a probe-based polymerase chain reaction. Am. J. Trop. Med. Hyg. 62:310-318. [DOI] [PubMed] [Google Scholar]
- 8.Higgins, J. A., M. S. Ibrahim, F. K. Knauert, G. V. Ludwig, T. M. Kijek, J. W. Ezzell, B. C. Courtney, and E. A. Henchal. 2000. Sensitive and rapid identification of biological threat agents. Ann. N. Y. Acad. Sci. 894:130-148. [DOI] [PubMed] [Google Scholar]
- 9.Holland, P. M., R. D. Abramson, R. Watson, and D. H. Gelfand. 1991. Detection of specific polymerase chain reaction product by utilizing the 5′-3′ exonuclease activity of Thermus aquaticus DNA polymerase. Proc. Natl. Acad. Sci. USA 88:7276-7280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ibrahim, M. S., J. J. Esposito, P. B. Jahrling, and R. S. Lofts. 1997. The potential of 5′ nuclease PCR for detecting a single-base polymorphism in orthopoxvirus. Mol. Cell. Probes 11:143-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ibrahim, M. S., R. S. Lofts, P. B. Jahrling, E. A. Henchal, V. W. Weedn, M. A. Northrup, and P. Belgrader. 1998. Real-time microchip PCR for detecting single base difference in viral and human DNA. Anal. Chem. 70:2013-2017. [DOI] [PubMed] [Google Scholar]
- 12.Lapa, S., M. Mikheev, S. Shchelkunov, V. Mikhailovich, A. Sobolev, V. Blinov, I. Babkin, A. Guskov, A. E. Sokunov, A. Zasedatelev, L. Sandakhchiev, and A. Mirzabekov. 2002. Species-level identification of orthopoxviruses with an oligonucleotide microchip. J. Clin. Microbiol. 40:753-757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee, L. G., C. R. Connell, and W. Bloch. 1993. Allelic discrimination by nick-translation PCR with fluorogenic probes. Nucleic Acids Res. 21:3761-3766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Loparev, V. N., R. F. Massung, J. J. Esposito, and H. Meyer. 2001. Detection and differentiation of Old World orthopoxviruses: restriction fragment length polymorphism of the crmB gene region. J. Clin. Microbiol. 39:94-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mackett, M., and L. C. Archard. 1979. Conservation and variation in orthopoxvirus genome structure. J. Gen. Virol. 45:683-701. [DOI] [PubMed] [Google Scholar]
- 16.Massung, R. F., L. I. Liu, J. Qi, J. C. Knight, T. E. Yuran, A. R. Kerlavage, J. M. Parsons, J. C. Venter, and J. J. Esposito. 1994. Analysis of the complete genome of smallpox variola major virus strain Bangladesh-1975. Virology 201:215-240. [DOI] [PubMed] [Google Scholar]
- 17.Meyer, H., M. Pfeffer, and H. J. Rziha. 1994. Sequence alterations within and downstream of the A-type inclusion protein genes allow differentiation of orthopoxvirus species by polymerase chain reaction. J. Gen. Virol. 75:1975-1981. [DOI] [PubMed] [Google Scholar]
- 18.Meyer, H., S. L. Ropp, and J. J. Esposito. 1997. Gene for A-type inclusion body protein is useful for a polymerase chain reaction assay to differentiate orthopoxviruses. J. Virol. Methods 64:217-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meyer, H., S. L. Ropp, and J. J. Esposito. 1998. Poxviruses, p. 199-211. In A. Warnes and J. Stephenson (ed.), Methods in molecular medicine: diagnostic virology protocols. Humana Press, Totowa, N.J.
- 20.Meyer, H., H. Neubauer, and M. Pfeffer. 2002. Amplification of Variola virus-specific sequences in German cowpox virus isolates. J. Vet. Med. Infect. Dis. Vet. Public Health 49:17-19. [DOI] [PubMed] [Google Scholar]
- 21.Neubauer, H., M. Pfeffer, and H. Meyer. 1997. Specific detection of mousepox virus by polymerase chain reaction. Lab. Anim. 31:201-205. [DOI] [PubMed] [Google Scholar]
- 22.Neubauer, H., U. Reischl, S. Ropp, J. J. Esposito, H. Wolf, and H. Meyer. 1998. Specific detection of monkeypox virus by polymerase chain reaction. J. Virol. Methods 74:201-207. [DOI] [PubMed] [Google Scholar]
- 23.Ropp, S. L., Q. Jin, J. C. Knight, R. Massung, and J. J. Esposito. 1995. PCR strategy for identification and differentiation of smallpox and other orthopoxviruses. J. Clin. Microbiol. 33:2069-2076. [DOI] [PMC free article] [PubMed] [Google Scholar]