Abstract
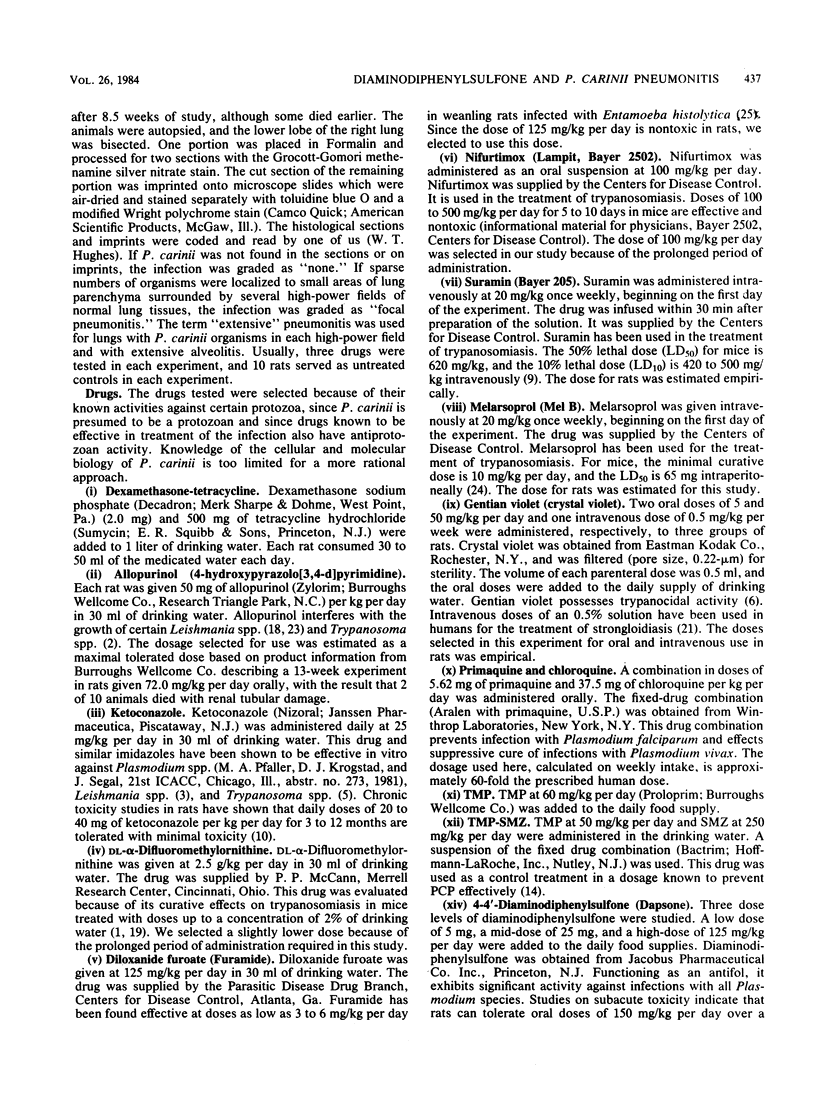
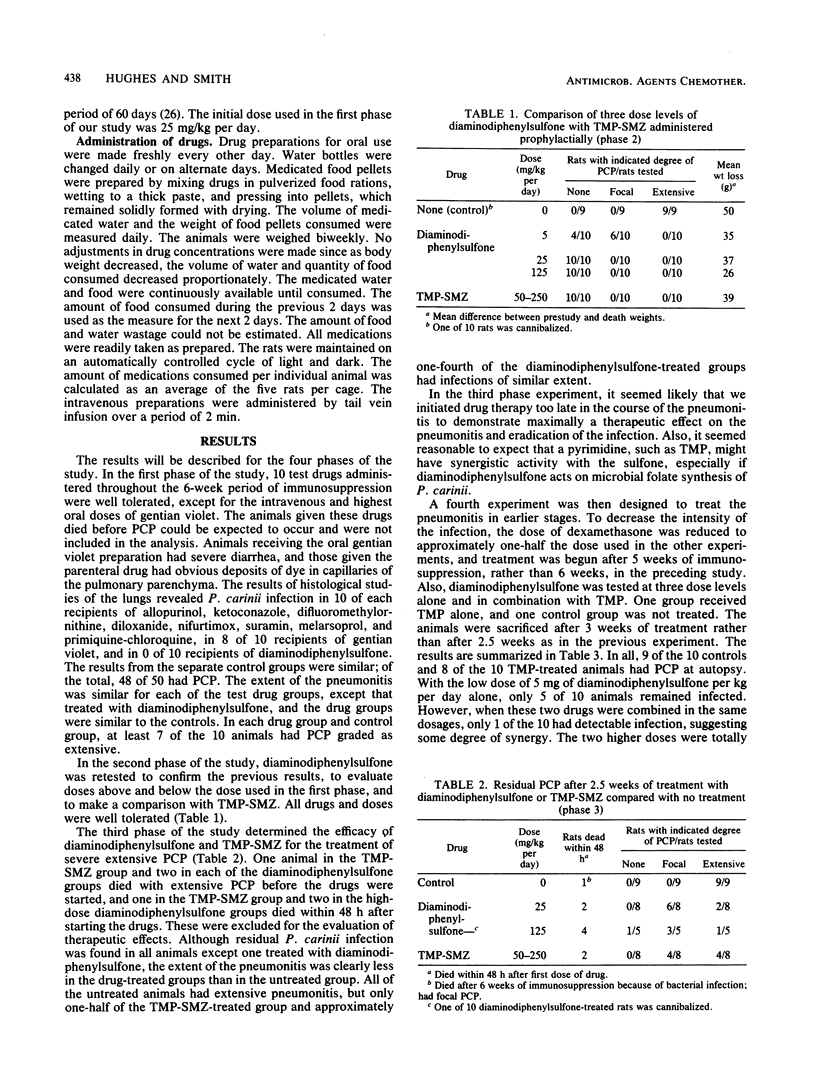
The purpose of this study was to identify new drugs for the prevention and treatment of Pneumocystis carinii pneumonitis (PCP) induced in rats by continuous daily dosage with dexamethasone. Initially, test drugs were administered prophylactically as a screen for efficacy. Drugs were selected because of their known activity against certain protozoa and their tolerance in human usage. Doses were based on previous studies in rats or estimated from usage in humans and lower animals. Allopurinol (50 mg/kg per day), ketoconazole (25 mg/kg per day), difluoromethylornithine (2.5 g/kg per day), diloxanide (125 mg/kg per day, nifurtimox (100 mg/kg per day), suramin (20 mg/kg per day), melarsoprol (20 mg/kg per day), gentian violet (0.5 mg/kg per week, 5 and 50 mg/kg per day), primaquine (5.6 mg/kg per day) and chloroquine (37.5 mg/kg per day) were ineffective, whereas diaminodiphenylsulfone (daspone) (25 mg/kg per day) was totally effective in preventing the infection. Diaminodiphenylsulfone was then evaluated at dose levels of 5, 25, and 125 mg/kg per day and compared with trimethoprim-sulfamethoxazole (TMP-SMZ), given at 50 per 250 mg/kg per day orally. The two highest dose levels of diaminodiphenylsulfone and TMP-SMZ prevented the infection in all of the animals, and the lowest dose of diaminodiphenylsulfone prevented it in 40% of the rats. All of the untreated controls developed PCP. To determine therapeutic efficacy, animals with extensive PCP were treated for 2.5 weeks with diaminodiphenylsulfone or TMP-SMZ. Based on residual extensive pneumonitis at the completion of treatment, the pneumonitis was reduced to 50% by TMP-SMZ and to 25% by diaminodiphenylsulfone, whereas 100% of untreated controls had extensive PCP. When treatment was begun earlier in the course of the pneumonitis, diaminodiphenylsulfone was totally effective in eradicating the infection. These results suggest that diaminodiphenylsulfone is an effective drug for the treatment and prevention of murine PCP and that it is at least as effective as TMP-SMZ.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bacchi C. J., Nathan H. C., Hutner S. H., McCann P. P., Sjoerdsma A. Polyamine metabolism: a potential therapeutic target in trypanosomes. Science. 1980 Oct 17;210(4467):332–334. doi: 10.1126/science.6775372. [DOI] [PubMed] [Google Scholar]
- Berman J. D. Activity of imidazoles against Leishmania tropica in human macrophage cultures. Am J Trop Med Hyg. 1981 May;30(3):566–569. doi: 10.4269/ajtmh.1981.30.566. [DOI] [PubMed] [Google Scholar]
- DeGowin R. L. A review of therapeutic and hemolytic effects of dapsone. Arch Intern Med. 1967 Aug;120(2):242–248. [PubMed] [Google Scholar]
- Docampo R., Moreno S. N., Muniz R. P., Cruz F. S., Mason R. P. Light-enhanced free radical formation and trypanocidal action of gentian violet (crystal violet). Science. 1983 Jun 17;220(4603):1292–1295. doi: 10.1126/science.6304876. [DOI] [PubMed] [Google Scholar]
- Docampo R., Moreno S. N., Turrens J. F., Katzin A. M., Gonzalez-Cappa S. M., Stoppani A. O. Biochemical and ultrastructural alterations produced by miconazole and econazole in Trypanosoma cruzi. Mol Biochem Parasitol. 1981 Jul;3(3):169–180. doi: 10.1016/0166-6851(81)90047-5. [DOI] [PubMed] [Google Scholar]
- Frenkel J. K., Good J. T., Shultz J. A. Latent Pneumocystis infection of rats, relapse, and chemotherapy. Lab Invest. 1966 Oct;15(10):1559–1577. [PubMed] [Google Scholar]
- Graham W. R., Jr Adverse effects of dapsone. Int J Dermatol. 1975 Sep;14(7):494–500. doi: 10.1111/j.1365-4362.1975.tb04283.x. [DOI] [PubMed] [Google Scholar]
- Heel R. C., Brogden R. N., Carmine A., Morley P. A., Speight T. M., Avery G. S. Ketoconazole: a review of its therapeutic efficacy in superficial and systemic fungal infections. Drugs. 1982 Jan-Feb;23(1-2):1–36. doi: 10.2165/00003495-198223010-00001. [DOI] [PubMed] [Google Scholar]
- Hughes W. T., Feldman S., Chaudhary S. C., Ossi M. J., Cox F., Sanyal S. K. Comparison of pentamidine isethionate and trimethoprim-sulfamethoxazole in the treatment of Pneumocystis carinii pneumonia. J Pediatr. 1978 Feb;92(2):285–291. doi: 10.1016/s0022-3476(78)80028-6. [DOI] [PubMed] [Google Scholar]
- Hughes W. T., Kuhn S., Chaudhary S., Feldman S., Verzosa M., Aur R. J., Pratt C., George S. L. Successful chemoprophylaxis for Pneumocystis carinii pneumonitis. N Engl J Med. 1977 Dec 29;297(26):1419–1426. doi: 10.1056/NEJM197712292972602. [DOI] [PubMed] [Google Scholar]
- Hughes W. T. Limited effect of trimethoprim-sulfamethoxazole prophylaxis on Pneumocystis carinii. Antimicrob Agents Chemother. 1979 Sep;16(3):333–335. doi: 10.1128/aac.16.3.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes W. T., McNabb P. C., Makres T. D., Feldman S. Efficacy of trimethoprim and sulfamethoxazole in the prevention and treatment of Pneumocystis carinii pneumonitis. Antimicrob Agents Chemother. 1974 Mar;5(3):289–293. doi: 10.1128/aac.5.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ismail G., Boxer L. A., Allen J. M., Baehner R. L. Improvement of polymorphonuclear leucocyte oxidative and bactericidal functions in chronic granulomatous disease with 4-amino-4'-hydroxylaminodiphenyl sulphone. Br J Haematol. 1978 Oct;40(2):219–229. doi: 10.1111/j.1365-2141.1978.tb03659.x. [DOI] [PubMed] [Google Scholar]
- Jaffe H. S., Abrams D. I., Ammann A. J., Lewis B. J., Golden J. A. Complications of co-trimoxazole in treatment of AIDS-associated Pneumocystis carinii pneumonia in homosexual men. Lancet. 1983 Nov 12;2(8359):1109–1111. doi: 10.1016/s0140-6736(83)90627-x. [DOI] [PubMed] [Google Scholar]
- Kluge R. M., Spaulding D. M., Spain A. J. Combination of pentamidine and trimethoprim-sulfamethoxazole in therapy of Pneumocystis carinii pneumonia in rats. Antimicrob Agents Chemother. 1978 Jun;13(6):975–978. doi: 10.1128/aac.13.6.975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marr J. J., Berens R. L. Antileishmanial effect of allopurinol. II. Relationship of adenine metabolism in Leishmania species to the action of allopurinol. J Infect Dis. 1977 Dec;136(6):724–732. doi: 10.1093/infdis/136.6.724. [DOI] [PubMed] [Google Scholar]
- PALMER E. D. A note on the treatment of strongyloidiasis with intravenous gentian violet. Am J Trop Med Hyg. 1950 Jan;30(1):91–91. doi: 10.4269/ajtmh.1950.s1-30.91. [DOI] [PubMed] [Google Scholar]
- Peters J. H., Gordon G. R., Ghoul D. C., Tolentino J. G., Walsh G. P., Levy L. The diposition of the antileprotic drug dapsone (DDS) in Philippine subjects. Am J Trop Med Hyg. 1972 Jul;21(4):450–457. doi: 10.4269/ajtmh.1972.21.450. [DOI] [PubMed] [Google Scholar]
- Pfaller M. A., Marr J. J. Antileishmanial effect of allopurinol. Antimicrob Agents Chemother. 1974 May;5(5):469–472. doi: 10.1128/aac.5.5.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WOOLFE G. IV. The search for new amoebicidal drugs. Trans R Soc Trop Med Hyg. 1957 Jul;51(4):320–326. doi: 10.1016/0035-9203(57)90122-0. [DOI] [PubMed] [Google Scholar]
- Wu D. L., DuBois K. P. Studies on the mechanism of the toxic action of diaminodiphenylsulfone (DDS) to mammals. Arch Int Pharmacodyn Ther. 1970 Jan;183(1):36–45. [PubMed] [Google Scholar]


