Abstract
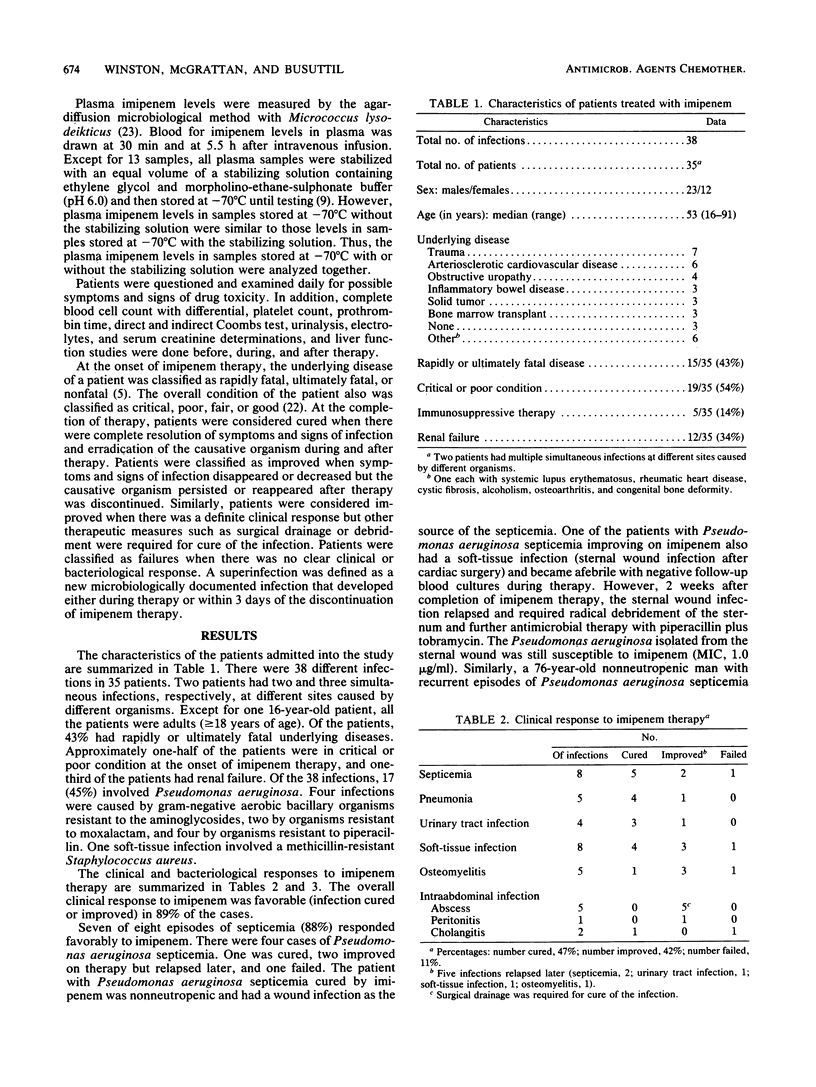
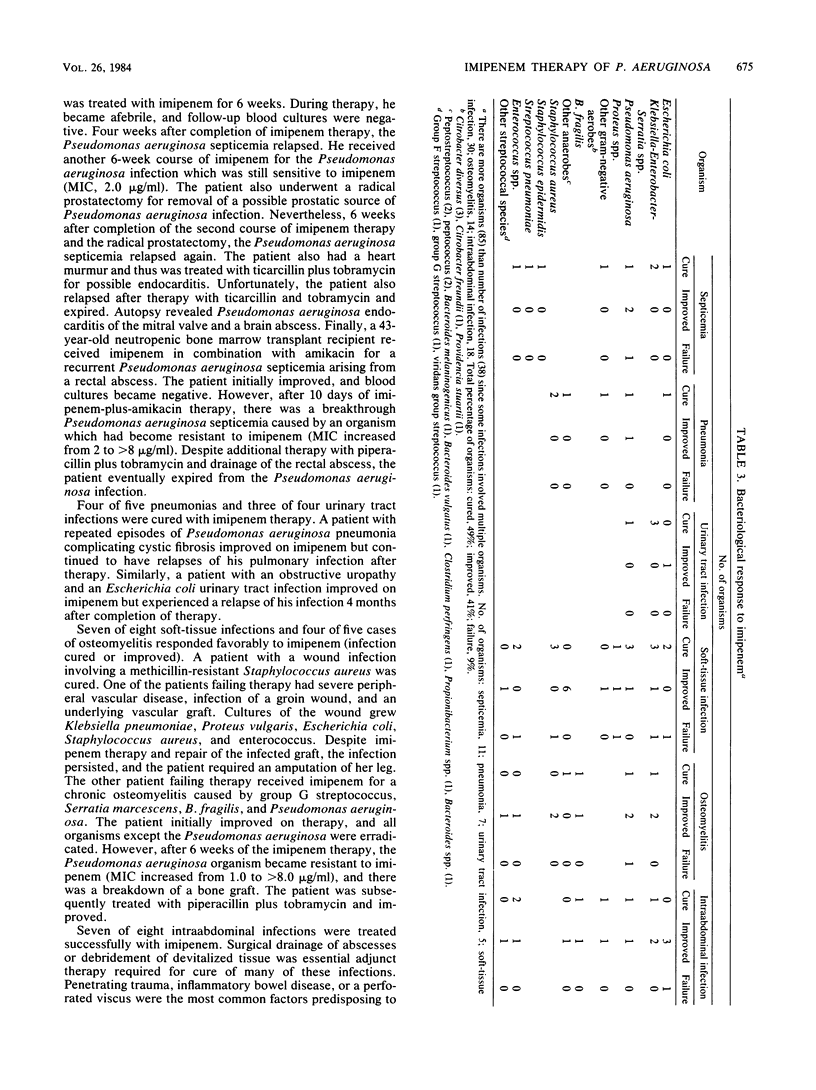
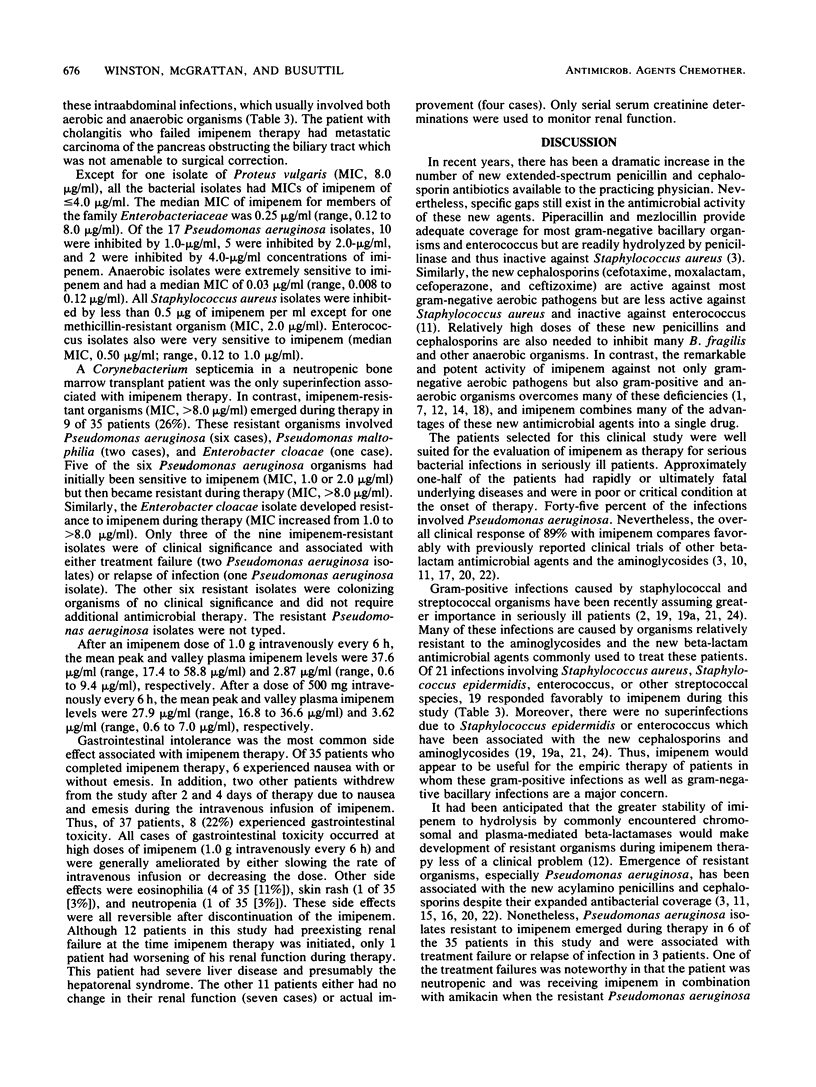
Imipenem is the first of a new class of beta-lactam antimicrobial agents with remarkable and extremely potent in vitro activity against most commonly isolated bacterial pathogens, including Staphylococcus aureus, enterococcus, members of the family Enterobacteriaceae, Pseudomonas aeruginosa, Bacteroides fragilis, and Hemophilus influenzae. The clinical efficacy and toxicity of imipenem were evaluated in 35 patients with 38 different infections. The overall clinical response was favorable (infections cured or improved) in 89% of the infections (34 of 38). Of the 17 infections with P. aeruginosa, 15 were cured or improved. However, P. aeruginosa isolates resistant to imipenem emerged during the therapy of six infections, and two cases of P. aeruginosa septicemia later relapsed after imipenem therapy. Gastrointestinal toxicity (nausea with or without emesis) occurred in 17% of the patients (6 of 35) but was ameliorated by slowing the rate of intravenous infusion or lowering the dose of imipenem. Except for certain severe P. aeruginosa infections, imipenem is effective and relatively safe therapy for infections caused by susceptible organisms.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cherubin C. E., Corrado M. L., Sierra M. F., Gombert M. E., Shulman M. Susceptibility of gram-positive cocci to various antibiotics, including cefotaxime, moxalactam, and N-formimidoyl thienamycin. Antimicrob Agents Chemother. 1981 Oct;20(4):553–555. doi: 10.1128/aac.20.4.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J., Donnelly J. P., Worsley A. M., Catovsky D., Goldman J. M., Galton D. A. Septicaemia caused by viridans streptococci in neutropenic patients with leukaemia. Lancet. 1983 Dec 24;2(8365-66):1452–1454. doi: 10.1016/s0140-6736(83)90799-7. [DOI] [PubMed] [Google Scholar]
- Eliopoulos G. M., Moellering R. C., Jr Azlocillin, mezlocillin, and piperacillin: new broad-spectrum penicillins. Ann Intern Med. 1982 Nov;97(5):755–760. doi: 10.7326/0003-4819-97-5-755. [DOI] [PubMed] [Google Scholar]
- Kesado T., Hashizume T., Asahi Y. Antibacterial activities of a new stabilized thienamycin, N-formimidoyl thienamycin, in comparison with other antibiotics. Antimicrob Agents Chemother. 1980 Jun;17(6):912–917. doi: 10.1128/aac.17.6.912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreger B. E., Craven D. E., Carling P. C., McCabe W. R. Gram-negative bacteremia. III. Reassessment of etiology, epidemiology and ecology in 612 patients. Am J Med. 1980 Mar;68(3):332–343. doi: 10.1016/0002-9343(80)90101-1. [DOI] [PubMed] [Google Scholar]
- Kropp H., Sundelof J. G., Hajdu R., Kahan F. M. Metabolism of thienamycin and related carbapenem antibiotics by the renal dipeptidase, dehydropeptidase. Antimicrob Agents Chemother. 1982 Jul;22(1):62–70. doi: 10.1128/aac.22.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kropp H., Sundelof J. G., Kahan J. S., Kahan F. M., Birnbaum J. MK0787 (N-formimidoyl thienamycin): evaluation of in vitro and in vivo activities. Antimicrob Agents Chemother. 1980 Jun;17(6):993–1000. doi: 10.1128/aac.17.6.993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neu H. C., Labthavikul P. Comparative in vitro activity of N-formimidoyl thienamycin against gram-positive and gram-negative aerobic and anaerobic species and its beta-lactamase stability. Antimicrob Agents Chemother. 1982 Jan;21(1):180–187. doi: 10.1128/aac.21.1.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neu H. C. The new beta-lactamase-stable cephalosporins. Ann Intern Med. 1982 Sep;97(3):408–419. doi: 10.7326/0003-4819-97-3-408. [DOI] [PubMed] [Google Scholar]
- Neu H. C. Tobramycin: an overview. J Infect Dis. 1976 Aug;134 (Suppl):S3–19. doi: 10.1093/infdis/134.supplement_1.s3. [DOI] [PubMed] [Google Scholar]
- Norrby S. R., Alestig K., Björnegård B., Burman L. A., Ferber F., Huber J. L., Jones K. H., Kahan F. M., Kahan J. S., Kropp H. Urinary recovery of N-formimidoyl thienamycin (MK0787) as affected by coadministration of N-formimidoyl thienamycin dehydropeptidase inhibitors. Antimicrob Agents Chemother. 1983 Feb;23(2):300–307. doi: 10.1128/aac.23.2.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens W. E., Finegold S. M. Comparative in vitro susceptibilities of anaerobic bacteria to cefmenoxime, cefotetan, and N-formimidoyl thienamycin. Antimicrob Agents Chemother. 1983 Apr;23(4):626–629. doi: 10.1128/aac.23.4.626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platt R., Ehrlich S. L., Afarian J., O'Brien T. F., Pennington J. E., Kass E. H. Moxalactam therapy of infections caused by cephalothin-resistant bacteria: influence of serum inhibitory activity on clinical response and acquisition of antibiotic resistance during therapy. Antimicrob Agents Chemother. 1981 Sep;20(3):351–355. doi: 10.1128/aac.20.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon G. L., Snydman D. R., Tally F. P., Gorbach S. L. Clinical trial of piperacillin with acquisition of resistance by Pseudomonas and clinical relapse. Antimicrob Agents Chemother. 1980 Jul;18(1):167–170. doi: 10.1128/aac.18.1.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith C. R., Baughman K. L., Edwards C. Q., Rogers J. F., Lietman P. S. Controlled comparison of amikacin and gentamicin. N Engl J Med. 1977 Feb 17;296(7):349–353. doi: 10.1056/NEJM197702172960701. [DOI] [PubMed] [Google Scholar]
- Tally F. P., Jacobus N. V., Gorbach S. L. In vitro activity of N-formimidoyl thienamycin (MK0787). Antimicrob Agents Chemother. 1980 Oct;18(4):642–644. doi: 10.1128/aac.18.4.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade J. C., Schimpff S. C., Newman K. A., Wiernik P. H. Staphylococcus epidermidis: an increasing cause of infection in patients with granulocytopenia. Ann Intern Med. 1982 Oct;97(4):503–508. doi: 10.7326/0003-4819-97-4-503. [DOI] [PubMed] [Google Scholar]
- Winston D. J., Barnes R. C., Ho W. G., Young L. S., Champlin R. E., Gale R. P. Moxalactam plus piperacillin versus moxalactam plus amikacin in febrile granulocytopenic patients. Am J Med. 1984 Sep;77(3):442–450. doi: 10.1016/0002-9343(84)90100-1. [DOI] [PubMed] [Google Scholar]
- Winston D. J., Busuttil R. W., Kurtz T. O., Young L. S. Moxalactam therapy for bacterial infections. Arch Intern Med. 1981 Nov;141(12):1607–1612. [PubMed] [Google Scholar]
- Winston D. J., Dudnick D. V., Chapin M., Ho W. G., Gale R. P., Martin W. J. Coagulase-negative staphylococcal bacteremia in patients receiving immunosuppressive therapy. Arch Intern Med. 1983 Jan;143(1):32–36. [PubMed] [Google Scholar]
- Winston D. J., Murphy W., Young L. S., Hewitt W. L. Piperacillin therapy for serious bacterial infections. Am J Med. 1980 Aug;69(2):255–261. doi: 10.1016/0002-9343(80)90386-1. [DOI] [PubMed] [Google Scholar]
- Winters R. E., Litwack K. D., Hewitt W. L. Relation between dose and levels of gentamicin in blood. J Infect Dis. 1971 Dec;124 (Suppl):S90–S95. doi: 10.1093/infdis/124.supplement_1.s90. [DOI] [PubMed] [Google Scholar]
- Yu V. L. Enterococcal superinfection and colonization after therapy with moxalactam, a new broad-spectrum antibiotic. Ann Intern Med. 1981 Jun;94(6):784–785. doi: 10.7326/0003-4819-94-6-784. [DOI] [PubMed] [Google Scholar]



