Anatomy
The pituitary gland, or hypophysis, is located in the hypophyseal fossa, which is an oval depression in the basisphenoid bone located ventral to the hypothalamus (1). A stalk-like structure composed of nerves and vessels connects the pituitary gland with the hypothalamus (Figure 1). The pituitary gland is in close proximity to the optic, oculomotor, and trochlear nerves, and to the ophthalmic branch of the trigeminal nerve. The complex of bony structures around the pituitary gland has a saddle-like shape, and is called the “sella turcica,” or Turkish saddle (Figure 2). The normal adult canine pituitary gland is contained within the sella turcica and is visible on magnetic resonance images (Figure 3a–d).
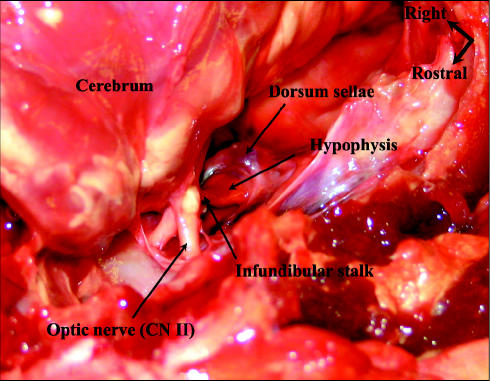
Figure 1.
An oblique rostrodorsal view of the normal canine pituitary gland (hypophysis) in situ with the cerebrum raised.
Figure 2.
A dorsal view of the cranial cavity with the brain and the pituitary gland removed.
Figure 3.
A contrast-enhanced (ProHance; Bracco Diagnostics, Princeton, New Jersey, USA) T1-weighted magnetic resonance image of a normal canine pituitary gland (hypophysis) in a dorsal view (3a), sagittal view (3b), and transverse view (3c). The dorsum sellae is visible just caudal to the hypophysis (3d) (the fatty bone marrow within the dorsum sellae appears white on a T1-weighted MR image).
Larger tumors of the pituitary gland may compress the hypothalamus, or invade the parenchyma of the hypothalamus and thalamus, causing hemorrhage and necrosis. Pituitary tumors may cause visual loss and other focal neurological signs due to the proximity of the gland to several cranial nerves. Large tumors may also result in an increase in intracranial pressure, and neurologic signs such as seizures and abnormal behavior are common.
Diagnostic Evaluation
Pituitary tumors may be endocrine-active or endocrine-inactive. In dogs with endocrine-active pituitary tumors, the most common endocrine abnormality is hypersecretion of adrenocorticotropic hormone (ACTH), resulting in Cushing’s disease. In cats, hypersecretion of growth hormone resulting in acromegaly also occurs. Diagnostic evaluation of a patient with a pituitary tumor includes a neurologic and ophthalmologic examination, endocrine evaluation, complete blood (cell) count (CBC), serum chemical analysis, urinalysis, and chest radiography. If neurologic abnormalities are present, computed tomographic or magnetic resonance imaging of the brain is indicated. Acromegalic cats, with or without neurological signs, should also have neuroimaging performed. Large pituitary masses are easily visualized with both imaging modalities (Figure 4a,b).
Figure 4.
A contrast-enhanced (Omnipaque 240; Amersham Health, Oakville, Ontario) computed tomographic (4a) and T1-weighted magnetic resonance (ProHance; Bracco Diagnostics, Princeton, New Jersey, USA) (4b) transverse image of a canine pituitary gland tumor (X).
Radiation Therapy
Radiation therapy reduces tumor size and produces an improvement in neurological signs in dogs and cats with pituitary tumors (2–5). Median overall survival after irradiation of pituitary tumors in dogs has been reported at 11.7 to 24.8 mo (2,3,6). In a recent study, 13 dogs with neurologic disease as a result of pituitary tumors that died due to worsening of their neurologic signs had a median survival of 43.6 mo. Dogs that were still alive or died from other causes were censored from the survival analysis (3).
The severity of neurological signs at presentation may influence the prognosis. In a study of 24 dogs with neurologic abnormalities as a result of a pituitary tumor, dogs that were presented with stupor or were nonambulatory had a 6.6 times higher risk of death due to their pituitary tumor than did dogs that were presented with seizures or mild neurological signs (6). This finding supports the importance of early diagnosis and treatment. Radiation therapy does not result in rapid control of hormone hypersecretion in dogs, and clinical signs of Cushing’s disease and high blood ACTH levels have been reported to persist for at least 1 y after completion of radiotherapy (2,7). Continued medical management of Cushing’s disease and serial endocrinologic evaluations are necessary for dogs that receive radiation treatment for a pituitary tumor.
Median survival times of 15 mo and 17.4 mo have been reported for a small number of cats treated with full course irradiation for pituitary tumors (4,5). Cats with Cushing’s disease require surgical treatment or continued medical management of their endocrine disease, together with radiation therapy. Medical management of acromegaly is ineffective in cats, and radiation therapy is indicated as the primary treatment (8). Diabetes mellitus is common in cats with hyperadrenocorticism and acromegaly, and cats may become clinically more responsive to insulin after radiotherapy (5).
In summary, radiation therapy is indicated for dogs and cats with a pituitary tumor causing neurological abnormalities, and for cats with acromegaly, with or without neurological abnormalities.
Side Effects of Radiation Treatment
Acute side effects of radiation therapy occur during or shortly after treatment; they are reversible and occur in rapidly dividing tissues that are located within the treatment fields. For treatment of a pituitary mass, early responding tissues within the treatment fields include those of skin, the pharyngeal mucosa, and the external auditory canal. The dose of radiation to skin is low with the treatment of pituitary tumors, and side effects are generally limited to mild erythema and some hair loss. Injection and mucositis affecting a limited portion of the pharynx may be seen after the 2nd wk of treatment, and medication for mild to moderate pain may be indicated, as well as the softening of a patient’s food. Depending on the arrangement of the treatment beams, a mild otitis externa may develop in one or both ears during the 3rd wk of treatment. A topical ear medication containing a corticosteroid can be used to decrease the inflammation. The acute side effects of radiation treatment have usually healed 2 to 3 wk after treatment has been completed. Due to the location of the pituitary gland, adjacent brain tissue will receive some radiation. Transient lethargy and somnolence may be seen in some patients as an acute side effect during radiation treatment of brain tissue (9).
Infrequently, neurological signs similar to those the animal exhibited prior to treatment may appear from 2 wk to 3 mo after radiation treatment of nervous (brain) tissue has concluded (10). These acute, delayed side effects of radiation treatment are usually temporary in nature, and generally resolve on their own. Steroids may be used in some patients that develop these signs.
The total dose of radiation that can be administered to a pituitary tumor is limited by the dose that normal tissues surrounding the tumor can tolerate without an unacceptable risk of late side effects. Late side effects of radiation therapy occur months to years after treatment; they are irreversible and occur in slowly dividing tissues that are located within the treatment fields. One or both cochlear ducts may receive radiation, and hearing impairment is a possible late side effect following pituitary irradiation. The brain is the dose-limiting structure in the treatment of pituitary tumors, and late side effects include changes such as necrosis and fibrosis. In general, a 3% to 5% risk of late complications is accepted for the treatment of pituitary tumors. The risk of late side effects depends on the volume of normal tissue treated, and the daily and total dose of radiation administered. Computerized radiation planning based on computed tomographic images is available to develop treatment beam arrangements that maximize the dose to the tumor, while minimizing the dose to normal tissues.
Acknowledgments
The authors thank Dr. Susan Kraft and Dr. Lisa Klopp for their assistance and for providing MR images.
References
- 1.Hullinger RL. The endocrine system. In: Evans HE, ed. Miller’s Anatomy of the Dog. Philadelphia: WB Saunders, 1993:559–585.
- 2.Dow SW, Lecouteur RA, Rosychuk RA, Powers BE, Kemppainen RJ, Gillette EL. Response of dogs with functional pituitary macroadenomas and macrocarcinomas to radiation. J Small Anim Pract. 1990;31:287–294. [Google Scholar]
- 3.Bley CR, Sumova A, Roos M, Kaser-Hotz B. Irradiation of brain tumors in dogs with neurologic disease. J Vet Intern Med. 2005;19:849–854. doi: 10.1892/0891-6640(2005)19[849:iobtid]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 4.Kaser-Hotz B, Rohrer CR, Stankeova S, Wergin M, Fidel J, Reusch C. Radiotherapy of pituitary tumours in five cats. J Small Anim Pract. 2002;43:303–307. doi: 10.1111/j.1748-5827.2002.tb00078.x. [DOI] [PubMed] [Google Scholar]
- 5.Mayer MN, Greco DS, LaRue SM. Outcomes of pituitary tumor irradiation in cats. J Vet Intern Med. 2006;20:1151–1154. doi: 10.1892/0891-6640(2006)20[1151:ooptii]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 6.Theon AP, Feldman EC. Megavoltage irradiation of pituitary macrotumors in dogs with neurologic signs. J Am Vet Med Assoc. 1998;213:225–231. [PubMed] [Google Scholar]
- 7.Goossens MM, Feldman EC, Theon AP, Koblik PD. Efficacy of cobalt 60 radiotherapy in dogs with pituitary-dependent hyperadrenocorticism. J Am Vet Med Assoc. 1998;212:374–376. [PubMed] [Google Scholar]
- 8.Feldman EC, Nelson RW. Acromegaly and hyperadrenocorticism in cats: A clinical perspective. J Feline Med Surg. 2000;2:153–158. doi: 10.1053/jfms.2000.0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fajardo L-G LF, Berthrong M, Anderson RE. Nervous system. In: Radiation Pathology. New York: Oxford Univ Pr, 2001:351–363.
- 10.Gillette EL, LaRue SM, Gillette SM. Normal tissue tolerance and management of radiation injury. Sem Vet Med Surg (Small Anim) 1995;10:209–213. [PubMed] [Google Scholar]