SYNOPSIS
Objective
The purpose of this study was to compare the burden of mental health disorders to the burden of other chronic care conditions as measured by emergency department (ED) visits by children with respect to prevalence rates, time trends, and hospital admission rates.
Methods
Data from the 1995–2001 National Hospital Ambulatory Medical Care Survey were used to assess the number of visits to emergency departments by children with a diagnosis of a mental health or chronic condition, a mental health-related reason for the visit, or a prescription or continuation of psychotropic medication.
Results
From 1995 to 2001, there was an increase in the proportion of visits by children with mental health problems. During the same period, the proportion of visits by children with chronic illness appeared stable. Overall, mental health diagnoses made up approximately 5% of all U.S. emergency department visits by children, similar to the percentage of total visits for other chronic conditions (5.2%). Approximately 15% of visits in both the mental health and chronic condition groups ended in hospital admission compared to less than 5% in the overall group of ED visits by children.
Conclusions
The burden of mental health related visits to U.S. EDs is growing at a faster rate than visits related to chronic conditions. Visit intensity, hospital admission, and medication utilization is just as intense as that for chronic conditions. Promoting provider mental health training and restructuring the ED visit to allow for rapid mental health assessment and immediate onsite or contiguous mental health care may be one way to improve outcomes for families and to position the ED as part of a larger integrated system of effective mental illness care.
Originally designed for the treatment of acute and life-threatening conditions, emergency departments are gradually addressing their role as a leading provider for chronic care services for patients. Individuals with chronic disorders constitute a large proportion of patients seen in emergency departments and represent a disproportionate share of visits and expenditures.1 To improve efficiency and effectiveness, emergency departments are adding case managers, patient motivation and education strategies, screening devices, and other interventions aimed at enhancing successful interventions for chronically ill children and their families. However, few of these interventions have been designed for children and adolescents with chronic mental disorders.
Childhood mental disorders are a large and growing threat to children and a major cause of chronic illness globally. According to the World Health Organization, four of the 10 most disabling diseases in the developed world are mental illnesses,2 with their initial onset generally occurring in childhood.3–5 Pediatric mental illness is estimated to occur in from 7% to 22% of all children.4–7 The identification of mental disorders in primary care settings increased rapidly in the past two decades,8–10 with parallel changes in prescriptions of psychotropic drugs for children and adolescents.11–13
Children with recognized mental health problems often have difficulty accessing mental health services due to inadequate numbers of providers, poor mental health service coverage, and inconvenient hours of service. Because U.S. emergency departments (EDs) have been mandated by both state and federal legislation to provide a medical screening examination for all patients who present themselves for care, the ED often is the only access point of care available 24 hours per day. Thus, the ED has increasingly become an important part of health services for children with mental disorders.
A recent study examining the rate of psychiatric visits to U.S. emergency departments showed a significant increase in the rate of pediatric mental health visits from 1993–1999.14 In addition, evidence is growing that patients and families with mental health problems have increasing rates of ED utilization.15 How mental health problems compare to the broader landscape of chronic diseases in the ED has not been studied, nor has any data on ED management of such patients been provided, particularly in children. We were interested in understanding the burden of mental health disorders in children presenting for care in the emergency department setting compared with other chronic care conditions with respect to visit rates, trends over time, and hospital admission rates. Using a nationally representative dataset of visits by children presenting with mental health problems to EDs over a six-year time period, we were specifically interested in comparing mental health conditions to all other chronic health conditions with respect to rates of hospital admissions, triage/acuity level, ED time, and medication use, and to see if these trends have changed over a seven-year period.
METHODS
Study design and dataset description
Using a cross-sectional study design, data from the 1995–2001 National Hospital Ambulatory Medical Care Surveys (NHAMCS) were analyzed. The NHAMCS, which is conducted annually by the National Center for Health Statistics (NCHS), is a nationally representative sample of visits to emergency departments of noninstitutional, general, short-stay, nonfederal hospitals in the United States, with data abstracted from the medical record.16 This study was exempted from approval by the Institutional Review Board because it was a secondary dataset not involving human subjects.
Data presentation
Mental health and chronic condition visits
The analysis assessed the number of visits by children younger than 19 years of age with a mental health or chronic condition diagnosis, a mental health patient-reported reason for visit, or a psychotropic drug prescription at time of ED visit. Diagnoses are determined by diagnoses assigned by providers during the visit. Visits with mental health and chronic condition diagnoses are identified using ICD-9 codes in any of the three listed discharge diagnoses.17 While these categories are not mutually exclusive, less than 1% of visits had both a mental health and chronic condition reported. Chronic conditions are identified using the classification of Kulthau,18 with all mental health conditions removed. A list of ICD-9 codes used to identify visits for a chronic condition is available from the authors upon request.
Mental health conditions are all visits with a recorded mental disorder diagnosis of 290.xx–309.xx and 311–314.xx (excluding brain damage). Visits for a patient-reported mental health problem were identified using the reason for visit codes supplied with the NHAMCS. All visits with a reason for visit code of 2300–2349, 1100–1199, 5818, and 5820 were defined as a visit for a patient-related mental health problem. Psychotropic drug visits were defined as visits in which at least one psychotropic drug was prescribed, supplied, administered, ordered, or refilled. Drug codes included in the NHAMCS were used to identify psychotropic drugs. NHAMCS specific drug codes of 626–632 were used to identify psychotropic drugs. We further classified mental health visits as any visit with a mental health diagnosis, mental health reason for visit, or a visit where a psychotropic medication was prescribed, refilled, continued, or ordered.
Visit characteristics
Visits where any medication was prescribed, supplied, administered, ordered, or continued were also assessed. In addition, whether or not a visit resulted in a hospital admission, the triage assignment of the visit (defined as less than one hour vs. one hour or more) as well as the total waiting time in the emergency department were assessed.
Patient characteristics
Visits were classified by patient age, race, gender, and region. Age was classified into three categories: younger than 5 years of age, 5 to 9 years, and 10 to 18 years. Race was defined as white or not white. Region was classified as Northeast, Midwest, South, and West.
Primary data analysis
The goal of our analysis was to describe the frequency of visits to emergency departments for mental health and chronic conditions by children in the United States over time. The NCHS included weights in the NHAMCS to enable the sample to represent all emergency department visits in the U.S., and all estimates presented in this study utilize these weights. To account for the sampling strategy, the survey procedures in STATA were used to calculate the estimates and generate 99% confidence intervals for the estimates.19 Significant differences between groups were assessed by using linear hypotheses that are weighted to account for the complex sampling strategy of NHAMCS. Differences in rates between each study year were assessed using a test for trend, and pairwise comparison was used to evaluate differences between years 1995 and 2001.
RESULTS
The 1995–2001 NHAMCS samples contained 6,932 visits to emergency departments with a mental health diagnosis, 6,970 visits with a mental health reason for visit, 10,411 visits with a psychotropic drug, and 6,205 with a chronic condition diagnosis. There were 19,317 visits defined as a mental health visit (i.e., mental health diagnosis, mental health reason for visit, psychotropic drug prescription or continuation).
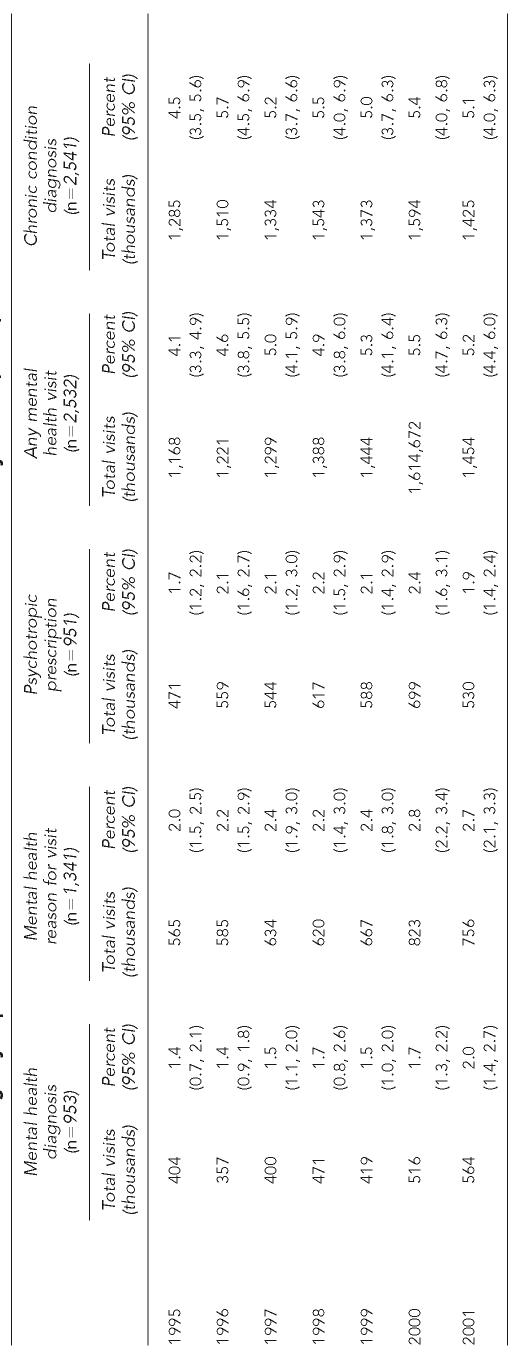
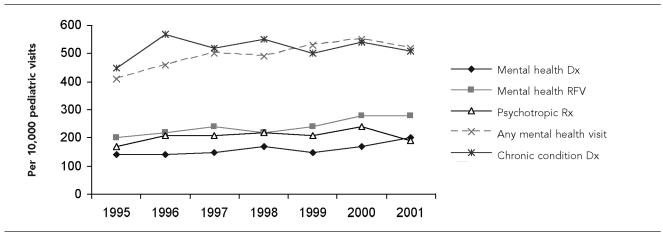
From 1995 to 2001 there was a modest increase in the proportion of visits by children to U.S. emergency departments (USEDs) for mental health problems, although the increase was not significant at the p<0.05 level (p<0.06)(Table 1). However, this modest increase was not evident when examining specific categories of mental health visits, only when all categories were combined. Neither mental health reasons for visits (p=0.21), visits with a psychotropic prescription (p=0.33), nor mental health diagnosis (p=0.09) showed a statistically significant time trend. While there was not an overall significant time trend (whether each year tested significantly different from another year), the pairwise comparisons were significantly different. For mental health visits, the proportion of emergency department visits for mental health problems was significantly greater in 2001 than in 1995 (p=0.013) (see Figure). During the same period the proportion of visits to USEDs by children with chronic conditions was stable (p=0.30), without a significant time trend by individual year or comparing 1995–2001.
Table 1.
Visits to U.S. emergency departments for mental health and chronic medical conditions by children, 1995, 2001
NOTES: Visits are weighted using weights provided by the National Center for Health Statistics to make estimates representative of all ED visits in the United States. Percent represents the proportion of all emergency department visits with the characteristics (e.g., percent of emergency department visits with a mental health diagnosis). Any mental health visit is any visit with a mental health diagnosis, mental health reason for visit, or psychotropic drug prescription.
Figure.
Trends in emergency department visits in children
NOTES: Data are from the 1996–2000 National Hospital Ambulatory Medical Care Surveys. Visit rates correspond to the rate per 10,000 hospital emergency department visits.
Mental health Dx = any mental health diagnosis
Mental health RFV = any patient mental health complaint as the reason for the visit
Psychotropic Rx = any psychotropic prescription provided during the visit
Any mental health visit = either a mental health diagnosis, mental health reason for visit, or psychotropic prescription indicated for the visit
Chronic condition Dx = a diagnosis for any chronic medical condition
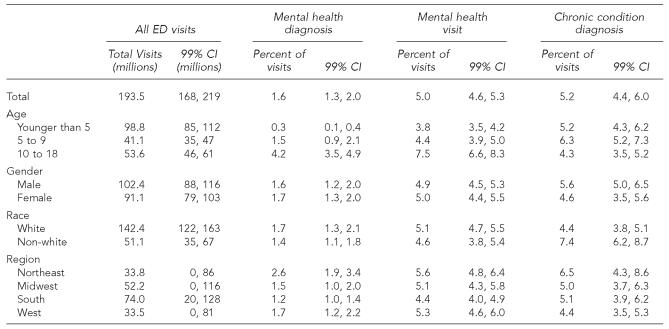
Overall, mental health visits made up approximately 5% of all U.S. ED visits, similar to the percentage of total visits for other chronic conditions (5.2%) (Table 2). The proportion of visits by children presenting with mental health conditions increased with age (3.8% in the younger than age 5 group, 4.4% in the 5–9 age group, 7.5% in the 10–18 age group; p=0.006), whereas the proportion of visits due to children with other chronic conditions did not increase with age but did significantly differ by age group (p=0.004). The proportion of visits by children presenting to the ED with other chronic illnesses was significantly different by race (p<0.001), while no difference in rates was observed for mental health visits (p=0.23). A higher proportion of visits by children with mental health conditions and other chronic conditions were seen in the Northeast compared to other parts of the country (p<0.01 for all regional differences from Northeast) (Table 2).
Table 2.
Children's visits to U.S. emergency departments for mental health and chronic medical conditions by patient characteristics, 1995–2001
NOTES: Visits are weighted using weights provided by the National Center for Health Statistics to make estimates representative of all ED visits in the United States.
Percent of visits = percentage of total ED visits with the diagnosis, reason for visit, etc. (e.g., percent of emergency department visits with a mental health diagnosis)
Mental health visit = a visit with either a mental health diagnosis, mental health reason for visit, or visit where a psychotropic prescription was provided
DISCUSSION
The frequency of visits for mental health problems in children presenting to emergency departments is large and growing. Unlike general chronic care visits, which remained stable throughout the study period, mental health visits increased. Mental health visits are as likely as chronic care visits to end in hospital admission, with most patients requiring medication before discharge from the ED. Moreover, most mental health visits require a consult from a mental health provider to assess safety issues and emergency treatment options.20
Understanding why this burden is growing is important. The NHAMCS database represents all nonmilitary U.S. hospitals, not just tertiary care centers. EDs across the country—rural, suburban and urban—are seeing increases in their mental health related visits. This increase may be related to declines in the supply of mental health services resulting from declining public mental health dollars and shortages of child mental health specialists. It may also be due to increased demand and growth in child and adolescent mental disorders, as has been noted in primary care and educational settings.8,9
Similar to services already offered for chronic conditions, the burden of pediatric mental health services may require comprehensive planning such as standardized assessments, available specialty evaluations, case managers, and linkages with outpatient and residential services. Restructuring the ED visit to allow for rapid mental health assessment and immediate onsite or contiguous mental health care may be one way to improve outcomes for families and to position the ED as part of a larger integrated system of effective chronic illness care.
Limitations
As with any secondary dataset analysis, this study is limited by the variables available in the dataset. It would have been interesting to look at severity of illness and measures of intensity of ED utilization such as intravenous fluids, laboratory tests, and the need for monitoring or restraints. In addition, using ICD-9 codes to identify mental illness is underrepresentative of the true prevalence of mental illness. However, the authors have increased mental health case finding by using the mental health visit, which includes visits with a combination of either a mental health ICD-9 code, a chief complaint of a mental health problem, and/or a visit resulting in a psychotropic medication prescription, order or continuation.
In summary, the visit, medication, and hospital admission intensity of mental health disorders in children presenting to U.S. emergency departments is as burdensome as that for children with chronic disorders. In the context of a lack of mental health care capacity in the community, it appears that the demand for ED-based mental health services will continue to increase. To respond to this need even while advocating for increased funding, services, and availability of traditional services for those with mental health issues, EDs should (1) re-examine how they respond to this need, (2) shore up and streamline the internal process by which they assess and meet the need, and (3) focus on the physician/nursing educational and training component to insure that these needs are met.
Table 3.
Characteristics of visits to the ED by children for mental health and chronic illness diagnoses, 1995–2001
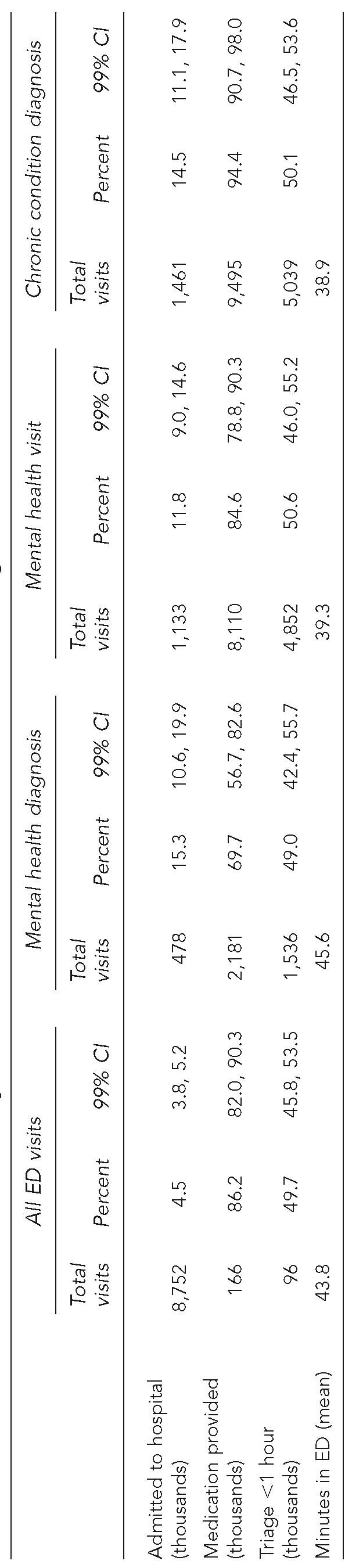
NOTES: Visits are weighted using weights provided by the National Center for Health Statistics to make estimates representative of all ED visits by children in the United States.
Percent = proportion of all emergency department visits with the characteristics (e.g., 4.5% of all emergency department visits by children resulted in a hospital admission)
ED = emergency department
CI = confidence interval
REFERENCES
- 1.Newacheck PW, Kim SE. A national profile of health care utilization and expenditures for children with special health care needs. Arch Pediatr Adolesc Med. 2005;159:10–7. doi: 10.1001/archpedi.159.1.10. [DOI] [PubMed] [Google Scholar]
- 2.Jenkins R. Reducing the burden of mental illness. Lancet. 1997;349:1340. doi: 10.1016/S0140-6736(05)63200-X. [DOI] [PubMed] [Google Scholar]
- 3.Christie KA, Burke JD, Jr, Regier DA, Rae DS, Boyd JH, Locke BZ. Epidemiologic evidence for early onset of mental disorders and higher risk of drug abuse in young adults. Am J Psychiatry. 1988;145:971–5. doi: 10.1176/ajp.145.8.971. [DOI] [PubMed] [Google Scholar]
- 4.Offord DR, Boyle MH, Szatmari P, Rae-Grant NI, Links PS, Cadman DT, et al. Ontario Child Health Study II. Six-month prevalence of disorder and rates of service utilization. Arch Gen Psychiatry. 1987;44:832–6. doi: 10.1001/archpsyc.1987.01800210084013. [DOI] [PubMed] [Google Scholar]
- 5.Bland RC. Psychiatry and the burden of mental illness. Can J Psychiatry. 1998;43:801–10. doi: 10.1177/070674379804300804. [DOI] [PubMed] [Google Scholar]
- 6.Fergusson DM, Horwood LJ, Lynskey MT. Prevalence and comorbidity of DSM-III-R diagnoses in a birth cohort of 15 year olds. J Am Acad Child Adolesc Psychiatry. 1993;32:1127–34. doi: 10.1097/00004583-199311000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Breton JJ, Bergeron L, Valla JP, Berthiaume C, Gaudet N. Quebec child mental health survey: prevalence of DSM-III-R mental health disorders. J Child Psychol Psychiatry. 1999;40:375–84. [PubMed] [Google Scholar]
- 8.Kelleher KT, McInerny TK, Gardner WP, Childs GE, Wasserman RC. Increasing identification of psychosocial problems: 1979–1996. Pediatrics. 2000;105:1313–21. doi: 10.1542/peds.105.6.1313. [DOI] [PubMed] [Google Scholar]
- 9.Lavigne JV, Binns HJ, Christoffel KK, Rosenbaum D, Arend R, Smith K, et al. Behavioral and emotional problems among preschool children in pediatric primary care: prevalence and pediatricians' recognition. Pediatric Practice Research Group. Pediatrics. 1993;91:649–55. [PubMed] [Google Scholar]
- 10.Costello EJ, Edelbrock C, Costello AJ, Dulcan MK, Burns BJ, Brent D. Psychopathology in pediatric primary care: the new hidden morbidity. Pediatrics. 1988;82:415–24. [PubMed] [Google Scholar]
- 11.Olfson M, Gameroff MJ, Marcus SC, Waslick BD. Outpatient treatment of child and adolescent depression in the United States. Arch Gen Psychiatry. 2003;60:1236–42. doi: 10.1001/archpsyc.60.12.1236. [DOI] [PubMed] [Google Scholar]
- 12.Olfson M, Marcus SC, Weissman MM, Jensen PS. National trends in the use of psychotropic medications by children. J Am Acad Child Adolesc Psychiatry. 2002;41:514–21. doi: 10.1097/00004583-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Zito JM, Safer DJ, DosReis S, Gardner JF, Magder L, Soeken K, et al. Psychotropic practice patterns for youth: a 10-year perspective. Arch Pediatr Adolesc Med. 2003;157:17–25. doi: 10.1001/archpedi.157.1.17. [DOI] [PubMed] [Google Scholar]
- 14.Sills M, Bland S. Summary statistics for pediatric psychiatric visits to US emergency departments, 1993-1999. Pediatrics. 2002;110:e40. doi: 10.1542/peds.110.4.e40. [DOI] [PubMed] [Google Scholar]
- 15.Byrne M, Murphy AW, Plunkett PK, McGee HM, Murray A, Bury G. Frequent attenders to an emergency department: a study of primary health care use, medical profile, and psychosocial characteristics. Ann Emerg Med. 2003;41:309–18. doi: 10.1067/mem.2003.68. [DOI] [PubMed] [Google Scholar]
- 16.McCaig LF, Ly N. National Hospital Ambulatory Medical Care Survey: 2000 emergency department summary. Adv Data. 2002 Jun;4(327):1–27. [PubMed] [Google Scholar]
- 17.Washington: U.S. Department of Health and Human Services; 1989. International Classification of Diseases, 9th Revision, Clinical Modification, 3rd ed. [Google Scholar]
- 18.Kuhlthau K, Walker DK, Perrin JM, Bauman L, Gortmaker SL, Newacheck PW, Stein RE. Assessing managed care for children with chronic conditions. Health Aff (Millwood) 1998;17(4):42–52. doi: 10.1377/hlthaff.17.4.42. [DOI] [PubMed] [Google Scholar]
- 19.StataCorp. College Station (TX): Stata Corporation; 2002. Stata Statistical Software: Release 7.0 Special Edition. [Google Scholar]
- 20.Korn CS, Currier GW, Henderson SO. “Medical clearance” of psychiatric patients without medical complaints in the emergency department. J Emerg Med. 2000;18:173–6. doi: 10.1016/s0736-4679(99)00191-2. [DOI] [PubMed] [Google Scholar]