SYNOPSIS
Reviews of state public health preparedness improvements have been primarily limited to measuring funds expenditures and achievement of cooperative agreement benchmarks. Such reviews fail to assess states' actual capacity for meeting the challenges they may face during an emergency, as evidenced by activities undertaken during the various phases of a disaster. This article examines North Carolina's public health preparedness and response performance during two hurricanes, Hurricane Floyd in 1999 and Hurricane Isabel in 2003, as well as capacity building activities in the intervening years. North Carolina created new infrastructures, enhanced laboratory capacity, and strengthened communications after Hurricane Floyd. These activities facilitated implementation of functional capabilities through effective centralized communication, command and control incident management, and a rapid needs assessment and medical surveillance during Hurricane Isabel. North Carolina continues to implement these capabilities in public health emergencies. Measuring and implementing functional capabilities during exercises or real events facilitates achievement of preparedness performance standards, goals, and objectives.
Since 1999, the U.S. Department of Health and Human Services, Centers for Disease Control and Prevention (CDC) has provided $4,575 million to state and local agencies to improve public health preparedness.1 This funding, as well as funding through the Health Resources and Services Administration (HRSA), is designed to improve public health infrastructure to respond to bioterrorism events, infectious disease outbreaks, and other public health emergencies.2 Several recent studies3–6 have examined the impact of the federal investment on preparedness infrastructure improvements.
The Association of State and Territorial Health Officials surveyed its membership in early 2003 to determine state progress toward achieving the CDC and HRSA preparedness cooperative agreement requirements.3 Survey results indicated that states had achieved a variety of short-term goals and activities including hiring staff, developing preparedness plans and protocols, and creating new organizational infrastructures.3
The U.S. Government Accounting Office reviewed state cooperative agreement progress reports for CDC and HRSA preparedness programs to determine the extent to which states had completed program requirements within the first year of funding.4 States had made improvements in aspects of preparedness including disease surveillance systems, laboratory capacity, communications, workforce, surge capacity, regional coordination, and capacity to use the Strategic National Stockpile, but no state had completely met all preparedness requirements.4
The Trust for America's Health examined states' performance in 10 public health emergency preparedness capabilities in 2003 and 2004.5,6 These capabilities are organized into funding, fundamental components of a comprehensive public health system, and “Oall hazards” categories, which reflect the impact of preparedness efforts on traditional public health functions. While the state preparedness scores improved from 2003 to 2004, states were struggling to meet basic preparedness requirements and did not have adequate resources to meet competing public health priorities.5,6
The above studies are limited to examining expenditures and achievement of cooperative agreement requirements or other check-off benchmarks such as the presence of a pandemic flu plan. This focus reflects the initial CDC supplemental grant guidance, which concentrated on building capacity and establishing preparedness infrastructures. Asch et al. identified and evaluated 27 instruments for planning or evaluating public health preparedness using the Essential Public Health Services framework.7 The instruments reviewed, including the Public Health Performance Standards, provided no clear definition of preparedness or ways it should be measured, relied on subjective or structural measures, and did not measure agency accountability.7
Furthermore, existing public health preparedness studies do not include measures from disaster management8 or public health disaster9,10 literature. This literature examines disaster response, including bioterrorism events, in phases and defines public health responsibilities and functions for these phases. Noji identified five phases of a disaster and outlined activities that public health agencies should conduct to meet the needs of a community.9 Learning from Experience presents a logic model for public health preparedness capabilities.11 In this model, agencies conduct capacity-building activities to prepare for an effective response and perform functional capabilities during emergency response. Preparedness objectives are early outbreak detection, effective response and recovery, and return to normal functioning; preparedness goals are to mitigate morbidity and mortality, stress, and social consequences. For states to achieve public health preparedness objectives and goals, they must be able to conduct all components of response through implementing capacity-building activities and functional capabilities.11
This article examines North Carolina's public health preparedness and response performance improvements in capacity-building activities and functional capabilities between two hurricanes, Hurricane Floyd in 1999 and Hurricane Isabel in 2003. Many of the response requirements for hurricanes are similar to those of bioterrorism or other emergency events, and require implementation of all the major components of public health emergency response.11 Thus, we were presented with a natural experiment through which we could compare the level of preparedness and response to major hurricanes as indicative of the impact of major investments in North Carolina emergency preparedness. The full report of this study is available online at http://www.sph.unc.edu/nccphp/hurricane.pdf.
Event chronology
In 1999, North Carolina experienced catastrophic flooding as part of the aftermath of Hurricane Floyd, a Category II hurricane. Rainfall amounts of 15 to 20 inches were reported, surpassing historical records for flooding in the state. Storm surges reached 9 to 10 feet, and several tornadoes were reported in eastern North Carolina.12 Fifty-seven deaths were directly attributed to Floyd, with 35 of these deaths occurring in North Carolina. By March 2000, the Federal Emergency Management Agency (FEMA) had reported $1.08 billion in claims from North Carolina. Moreover, FEMA designated 66 counties and their residents as eligible to apply for disaster assistance.13
In 2003, another Category II storm, Hurricane Isabel, caused considerable wind damage to a number of North Carolina communities. Sustained winds of 64 to 84 knots were reported. Storm surges of six to eight feet were reported along the Atlantic coast, with a maximum surge of 10.5 feet reported on the Neuse River. Rainfall amounts averaged four to seven inches in eastern North Carolina.14 Isabel was directly responsible for 16 deaths, including one in North Carolina.14 In December 2003, FEMA reported $155.2 million in claims for assistance in North Carolina. FEMA designated 47 counties and their residents as eligible to apply for disaster assistance.15
METHODS
The North Carolina Division of Public Health (DPH) partnered with the North Carolina Center for Public Health Preparedness (NCCPHP) to conduct this study. NCCPHP is one of 52 preparedness centers in the country and is a program of the North Carolina Institute for Public Health, the service and outreach arm of the University of North Carolina, School of Public Health (UNC SPH).
The purposes of this study were to compare North Carolina's public health preparation, planning, and response between Hurricanes Floyd and Isabel, analyze the benefits of federal supplemental funding in intervening years, and assess improvements in public health capacity and functional capabilities to respond to two hurricanes. To capitalize on the natural experiment, we conducted two case studies with embedded units. Each hurricane event was a case study, and the separate phases of planning, preparing, and responding to the hurricane event were the embedded units.16
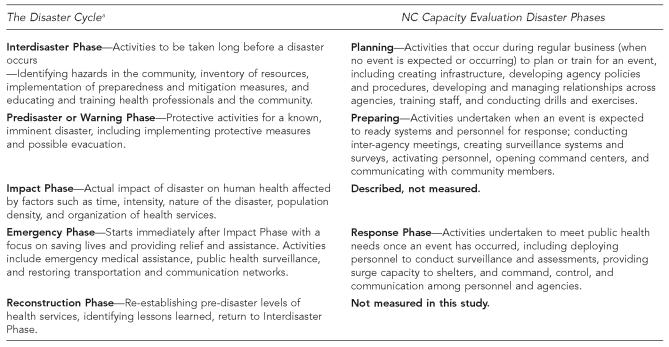
For the purposes of this study, we adapted Noji's9 disaster phases framework into planning, preparation, and response phases. Definitions of the phases used in this study and those developed by Noji can be found in Figure 1. The planning phase includes creating infrastructure, policies, and protocols; developing and managing relationships across agencies; training staff; and conducting drills and exercises. The preparing phase includes activities an agency undertakes when an event is expected, such as deploying personnel, implementing protocols, and communicating with other agencies and community members. Finally, the response phase includes activities related to implementing functional capabilities, such as conducting surveillance and assessment, coordinating the response through command and control incident management, and communicating with agencies and the public.
Figure 1.
Definitions of disaster phases and public health activities
a Noji EK. The public health consequences of disasters. New York: Oxford University Press; 1997.
We examined DPH performance of public health emergency operations within the three phases of the disasters. These operations are specified as surveillance, disease investigation, public information, and command, control, and communications functional capabilities. Evaluation questions for this study are presented in Figure 2.
Figure 2.
Questions for the evaluation of NC DPH planning, preparation, and response to Hurricanes Floyd and Isabel
NC DPH = North Carolina Division of Public Health
UNC SPH = University of North Carolina School of Public Health
Data collection methods included key informant interviews and document reviews. Interview participants were chosen because of their roles in planning, preparation, or response to Hurricanes Floyd and/or Isabel. An interview protocol was derived from the evaluation questions. Documents were state and federal protocols and records from the two hurricanes and general state emergency planning documents. The evaluation plan and case study protocols were submitted to and approved by the UNC SPH Institutional Review Board. Interview transcripts and documents were analyzed, and the data were used to answer the evaluation questions within the disaster phases framework.
RESULTS
Interviews and document review
We conducted a total of 32 interviews, 20 with individuals employed by the following agencies: 10 DPH, nine other North Carolina state agencies, one federal agency, and interviews with five local health department directors, four Public Health Regional Surveillance Team members, and three UNC SPH employees. All intended interviews occurred as planned. Eighty-nine documents, 23 for Hurricane Floyd and 66 for Hurricane Isabel, were documented, catalogued, and reviewed, representing nearly all documents requested. In some cases, documents for Hurricane Floyd were not available.
Hurricane Floyd planning
Prior to Hurricane Floyd, DPH had no specific policies for preparing for public health emergencies other than responsibilities outlined in the state Emergency Operations Plan. Although the state health director was a member of the State Emergency Response Team, DPH did not actively coordinate, plan, or prepare for events with the state Emergency Operations Center or Division of Emergency Management. The only preparedness training conducted was in counties with nuclear power plants (as required). DPH conducted no preparedness exercises in the year prior to Hurricane Floyd.
Hurricane Floyd preparation and response
Communication.
Preparation for the hurricane began with internal DPH meetings held 24 hours before landfall. DPH issued press releases with advice for citizens and communicated with local health departments to provide information on requesting assistance.
Command and control.
DPH used the existing management team structure to organize response activities. Within 48 hours of landfall, DPH deployed more than 20 professional staff from the environmental epidemiology and occupational and environmental health units.
In response to the enormous impact of Floyd, which affected 66 of North Carolina's 100 counties, DPH changed strategies within the first days of the response period. DPH organized the 13 counties most affected into seven public health zones. A coordinator was assigned to each zone to work directly with local health departments to establish plans to address priority concerns and acquire assistance. A public health zone manager was responsible for coordinating the efforts of the zone coordinators with DPH.
Surveillance and assessment.
A CDC Epidemic Intelligence Service officer created and implemented hospital medical surveillance protocols.17 Initially, public health workers were deployed to conduct community health assessments in teams. Assessment was later shifted to the zone coordinators to identify priority areas of health concerns within each county. Zone coordinators conducted health and illness assessments in their assigned counties with assistance from faculty and students at universities located in the central part of the state.
Despite the lack of infrastructure and systems, DPH “Ogot the job done” under extraordinary and long-lasting circumstances due to the tireless work of its employees. Employee dedication and the creation of an ad hoc zone coordinator system facilitated DPH response and met the needs of local public health agencies. Two factors that undermined DPH effectiveness were the lack of an underlying preparedness and response structure and a faulty emergency management environment. The accomplishments were remarkable, but the system and infrastructure shortcomings were a hindrance.
Capacity-building activities
Agency partnerships.
In 1999, North Carolina received a CDC Bioterrorism Planning and Assessment grant, continued the work of the Bioterrorism Steering Committee (the primary vehicle through which North Carolina's preparedness plan was developed and continues to be implemented), and created the Bioterrorism Team. This team comprises a broad group of stakeholders representing state and local agencies, community-based organizations, healthcare facilities, and professional associations involved with public health preparedness efforts. In fall 2001, DPH began meeting with other state agencies, specifically the Division of Emergency Management, to discuss bioterrorism response planning.
Infrastructure improvements.
In 2002, North Carolina created the Office of Public Health Preparedness and Response (PHP&R) within DPH. PHP&R coordinates all functions of the state response to public health emergencies. In turn, PHP&R created seven Public Health Regional Surveillance Teams (PHRSTs) to provide support to local health agencies across the state. The PHRST infrastructure was a direct outgrowth of the of the zone coordinator system used during the Hurricane Floyd response. The PHRST regions overlap with state hazardous material, or HAZMAT, regions.
By summer 2003, DPH had hired 34 full-time-equivalent staff, including 28 PHRST members, and surge capacity staff through the Department of Agriculture and Consumer Services (crisis center-affiliated veterinarians) and the Department of Environment and Natural Resources. Twelve new public health epidemiologists had also been hired statewide.
During 2002 and 2003, PHP&R created preparedness protocols and updated the state Emergency Operations Plan to address bioterrorism events, disease outbreaks, and other public health emergencies. A critical accomplishment was the creation of an Operations Plan, which outlines actions and establishes activation and coordination procedures to be carried out during a public health emergency. Additional infrastructure improvements included enhancing Biosafety Level-3 and Level-2 laboratories, purchasing vehicles and equipment, and implementing the emergency department database.
Communication.
In 2003, PHP&R established a Public Health Command Center in Raleigh to serve as a base for public health operations during an emergency as an extension of the state Emergency Operations Center. DPH also established and implemented the Health Alert Network for immediate statewide notification of public health events.
Training, exercises, and drills.
PHRST members and local public health staff received training in core public health competencies and bioterrorism and emergency preparedness competencies. PHP&R conducted state, local, and regional drills and exercises, and opened the Public Health Command Center twice to coordinate responses to public health emergencies, including a confirmed case of SARS.
Hurricane Isabel preparation
PHP&R began preparation for Isabel six days prior to landfall and intensified preparation efforts in the three days before landfall. These activities included deploying PHRSTs, opening the Public Health Command Center, and organizing logistics to implement functional capabilities. DPH staff communicated with Emergency Operations Center staff, other state agencies such as Emergency Management and the Department of Environmental and Natural Resources, the CDC, and UNC SPH faculty to meet surge capacity needs. Figure 3 presents a selected, but not exhaustive, list of PHP&R activities three days in advance of hurricane landfall.
Figure 3.
Selected North Carolina Division of Public Health, Office of Public Health Preparedness and Response Hurricane Isabel preparation activities
PHRST = Public Health Regional Surveillance Team
UNCSPH = University of North Carolina School of Public Health
Hurricane Isabel response
DPH and PHP&R implemented the following functional capabilities to meet public health needs after Hurricane Isabel landfall: epidemiology functions, including a rapid needs assessment and medical surveillance; communications; and command and control infrastructure.
Rapid needs assessment.
Prior to Hurricane Isabel's landfall, PHP&R staff and CDC quickly developed a rapid needs assessment instrument based on previous assessment instruments.18 PHP&R deployed 10 rapid needs assessment teams within 36 hours of landfall. Data from the rapid needs assessment indicated that minimal damage had occurred in the counties initially surveyed. Through communications with other counties, the coastal PHRST team, and data from FEMA and National Oceanic and Atmospheric Administration reports, it became clear that more substantial damage had occurred in other areas of the state. Public Health Command Center staff and the rapid needs assessment teams conducted a conference call to determine the next plan of action. The staff consensus was to complete remaining assessments in the initial counties and conduct a second round of assessments in counties more affected by the hurricane.
DPH and Division of Emergency Management personnel considered the data from the rapid needs assessment to be very useful in managing response needs. These were the first objective data to confirm that the initial counties surveyed had experienced minimal damage, thus allowing DPH and other agencies to redirect the response emphasis to more affected counties.
Medical surveillance.
DPH surveyed emergency departments in 33 North Carolina hospitals, two Veterans Affairs hospitals, and two referral hospitals to measure hurricane-related morbidity and mortality. The network of hospitals and systems included in the surveillance was based on the Hurricane Floyd surveillance activities, and the medical surveillance instrument was updated to collect data on injuries.
Communication.
The Public Health Command Center operations plan was tested and fully functional during Hurricane Isabel. All positions were staffed 24 hours a day, seven days a week, in three shifts. DPH and PHP&R leadership attended daily Emergency Operations Center briefings and then provided key information to the Public Health Command Center positions during daily briefings.
The Public Health Command Center standard operating procedures require a list of current contact information for all health directors and backup personnel, including work, home, and pager numbers. DPH personnel indicated that the ability to access this information quickly facilitated response communications between Command Center personnel and health directors. Communication with citizens occurred primarily through information packets provided directly by rapid needs assessment teams.
Study participants were positive about PHP&R's operation of the Public Health Command Center and the staff's ability to meet communication needs. For example, PHRST members contacted the Public Health Command Center to facilitate local health director requests for the Emergency Operations Center to relocate the National Guard deployment. Communications were not flawless, as there were delays in communication when Public Health Command Center or DPH managers could not be reached; nevertheless, the Public Health Command Center provided a single point of contact for public health needs and a structured process for tracking and answering questions.
Command and control.
Hurricane Isabel allowed PHP&R to thoroughly test the Operations Plan by implementing and testing protocols and systems. Employees in the Public Health Command Center managed critical activities, such as the rapid needs assessment and medical surveillance, and centralized communications with local health directors; they used the center as an extension of the State Emergency Operations Center. Hurricane Isabel also provided a critical opportunity to test command, control, and communication functions through the implementation of the rapid needs assessment.
DISCUSSION
This evaluation study demonstrated two primary findings: first, that DPH used federal bioterrorism cooperative agreement funding to implement capacity-building activities and functional capabilities that improved public health preparedness planning, preparation, and response to Hurricane Isabel as compared to the preparation and response to Hurricane Floyd. Second, that evaluating such activities and capabilities within the phases of disasters framework advances our understanding of preparedness beyond that obtained by methods that do not test capabilities in real-time, emergency conditions.
The capacity-building activities11 undertaken after Hurricane Floyd resulted in new staff, implementing the Health Alert Network and the NC Emergency Department Database, enhancing laboratory capacity, purchasing equipment, strengthening communication with other agencies, and providing staff training that included exercises and drills. These actions led to the demonstration of public health preparedness functional capabilities during Hurricane Isabel.11 Capabilities included effective, centralized communication through the Public Health Command Center and command and control incident management. Command and control incident management implements operational and functional plans and facilitates the performance of epidemiology and surveillance functions in emergency conditions (Figure 4). These capabilities were not present during the Hurricane Floyd response.
Figure 4.
North Carolina Division of Public Health Preparedness capacity-building activities and functional capability improvements
An important capacity-building activity undertaken was the strengthening of communication between state agencies, specifically between DPH and the State Division of Emergency Management. One person interviewed for this study remarked, “OEmergency Management considers DPH ′full players' and they work together throughout the crises and we all solve problems together.”
Findings of this study must be considered in light of some limitations. First, this project was designed to answer specific questions of interest identified by DPH; other questions regarding preparedness (e.g., how much of DPH's funds have been expended) were not considered. Such questions would be necessary to make a clear comparison of evaluation methods (real-time vs. hypothetical evaluation of preparedness). Second, DPH provided most documents and identified most interview participants, which may have positively biased evaluation results. Third, no attempts were made to verify document quality or accuracy.
The evaluation design, case studies within a natural experiment, was chosen because it is particularly useful to understand a situation or phenomenon in depth, particularly when cases rich in needed information are available.19 Further, information gleaned from the cases studied can provide insights into other similar situations.20 This design, however, has limited generalizeability and does not control for many threats to external validity.
Further improvements in preparedness capabilities
Review of DPH planning, preparation, and response to Hurricane Isabel revealed that protocols needed further improvement. Recommended protocol improvements included creating formal mechanisms to deploy PHRST members, finalizing mechanisms to reimburse PHRST members and volunteers for expenses incurred while deployed, and implementing a full incident command structure during a rapid needs assessment. In addition, study participants recommended further training for all DPH staff. DPH has addressed many of these improvements and continues to improve its capacity-building activities and functional capabilities. In 2004, DPH and PHP&R implemented a rapid needs assessment18 to investigate a Legionnaire's disease outbreak21 and opened the Public Health Command Center as part of a Shiga toxin-producing E. coli infections outbreak investigation.22
A RAND Corporation 2005 study identified the DPH PHRST infrastructure as an exemplary practice for public health preparedness. PHRSTs act as an innovative infrastructure for on-call consulting that enhances local outbreak readiness with specific team compositions that can be easily replicated. These teams build surveillance capacity by coordinating regional epidemiologic response activities and providing resources to local health departments.23
CDC's 2005 Cooperative Agreement Guidance emphasizes public health system performance parameters that require the implementation of capacities to achieve standards.24 Exercises and drills have also been used to identify gaps in preparedness plans, test functional capacities, and strengthen agency and community relationships partners.11 Such efforts identify problems in planning and functional capability; however, few evaluation studies of outcomes and cost-effectiveness of this approach have been conducted. Moreover, these efforts do not test capacity-building activities and functional capabilities in real-time, emergency conditions. In this evaluation study, the Hurricane Isabel rapid needs assessment revealed DPH capacity to make decisions in the field regarding the timing and organization of a second rapid needs assessment and identified a need for further protocol development. An exercise scenario may not identify these challenges or fully test command and control problem-solving capabilities between field personnel and incident commanders. Drills and exercises tend to have rote protocols that are not affected by changing information that occurs in real conditions. When possible, a real-time test of preparedness activities and capabilities would seem to further our understanding more than would simulated activities.
Other health departments have tested capacity-building activities and functional capabilities in outbreak investigations. Learning from Experience examined seven state responses to West Nile virus, SARS, monkeypox, and hepatitis A outbreaks.11 The Thurston County Health Department created a public health incident response plan and implemented incident command structure to conduct an investigation of HIV/AIDS transmission in the community, including triaging phone calls from the public and conducting contact tracing.25 These types of tests fulfill the current CDC Cooperative Agreement Guidance, which calls for data from drills and exercises, suggesting that data from real events could be one way of demonstrating achievement of performance standards.24
Public health systems must be able to respond to natural disasters, bioterrorism attacks, emerging infectious disease, and other public health emergencies. While these emergencies differ in their response requirements, public health systems that invest in a variety of capacity-building activities and test functional capabilities in real-time, emergency conditions will be better able to achieve the preparedness goals to mitigate mortality, morbidity, and the social consequences of the disaster.11,8 How states perform in real situations should be a major focus of evaluating public health preparedness. While agencies can create a number of plans and protocols through capacity-building activities during the planning phase of a public health emergency, agencies should be prepared to create just-in-time policies during the preparation and response phases of a public health emergency.
The considerable federal investment in public health preparedness capacity has yielded improvements in how state and local agencies achieve federal preparedness benchmarks, capacity-building activities, and functional capabilities. Yet, this funding occurs in cycles that often include periods of considerable neglect.26 Public health systems have competing priorities; bioterrorism and emergency preparedness are seen as an add-on function that detracts from funding for chronic public health challenges such as obesity.27 The capacity improvements and functional capabilities, however, will support public health systems in addressing public health emergencies, including avian influenza and natural disasters, which can affect much of the population. Future federal funding efforts could further improve public health preparedness by providing clear requirements for conducting public health capacity-building activities and demonstrating public health functional capabilities to meet public health preparedness objectives and goals.
REFERENCES
- 1.Johnson A. CDC's bioterrorism preparedness cooperative agreement. [cited 2005 Oct 21]. Presented at the Centers for Public Health Preparedness Annual Meeting; Boston, MA; 2005 Jul 11. Available from: URL: http://www.asph.org/acphp/CPHP_Meeting_2005.cfm.
- 2.Department of Health and Human Services (US). HHS Announces $1.1 billion in funding to states for bioterrorism preparedness. [cited 2006 Oct 3]. January 31, 2002. Available from: URL: http://www.hhs.gov/news/press/2002pres/20020131b.html.
- 3.Association of State and Territorial Health Officials. Washington: Association of State and Territorial Health Officials; 2003. Public health preparedness: a progress report—the first six months. [Google Scholar]
- 4.General Accounting Office (US) Washington: US General Accounting Office; 2004. Public health preparedness: response capacity improving, but much remains to be accomplished. [Google Scholar]
- 5.Trust for America's Health. Ready or not? 2003. Washington: Trust for America's Health; 2003. [cited 2004 Apr]. Protecting the public's health in the age of bioterrorism. Available from: URL: http://healthyamericans.org/state/bioterror/ [Google Scholar]
- 6.Trust for America's Health. 2nd ed. Washington: Trust for America's Health; 2004. [cited 2005 Jan 4]. Ready or not? Protecting the public's health in the age of bioterrorism. Available from: URL: http://healthyamericans.org/reports/bioterror04/BioTerror04Report.pdf. [Google Scholar]
- 7.Asch SM, Stoto M, Mendes M, Valdez RB, Gallagher ME, Halverson P, Lurie N. A review of instruments assessing public health preparedness. Public Health Rep. 2005;120:532–42. doi: 10.1177/003335490512000508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Quarantelli EL. Ten criteria for evaluating the management of community disasters. Disasters. 1997;21:39–56. doi: 10.1111/1467-7717.00043. [DOI] [PubMed] [Google Scholar]
- 9.Noji EK. New York: Oxford University Press; 1997. The public health consequences of disasters. [Google Scholar]
- 10.Landesman LY. Public health management of disasters: the practice guide. Washington: American Public Health Association; 2001. [Google Scholar]
- 11.RAND Corporation. RAND Health. Santa Monica: RAND Corporation; 2005. Learning from experience: the public health response to West Nile virus, SARS, monkeypox, and hepatitis A outbreaks in the United States. [Google Scholar]
- 12.Pasch RJ, Kimberlain TB, Stewart S. National Hurricane Center, National Oceanic and Atmospheric Administration. Preliminary report: Hurricane Floyd 7–17 September 1999. [cited 2004 Mar 15]. Available from: URL: http://www.nhc.noaa.gov/1999floyd.html.
- 13.Federal Emergency Management Agency (US) Six months after Floyd, recovery effort reaches $1.08 billion. March 10, 2000. [cited 2004 Mar 15]. Available from: URL: http://www.fema.gov/news/newsrelease_print.fema?id=9093.
- 14.Beven J, Cobb H. National Hurricane Center, National Oceanic and Atmospheric Administration. Tropical cyclone report: Hurricane Isabel, 6–19 September 2003. 2003. Dec 19, [cited 2004 Mar 15]. Available from: URL: http://www.nhc.noaa.gov/2003isabel.shtml.
- 15.Federal Emergency Management Agency (US) State/federal disaster aid tops $155 million. 2003. Dec 10, [cited 2004 Mar 15]. Available from: URL: http://www.fema.gov/news/newsrelease.fema?id=9029.
- 16.Yin RK. 2nd ed. Thousand Oaks (CA): Sage Publications; 1994. Case study research design and methods. [Google Scholar]
- 17.Morbidity and mortality associated with Hurricane Floyd---North Carolina September-October 1999. MMWR Morb Mortal Wkly Rep. 2000;49(17):369–72. [PubMed] [Google Scholar]
- 18.Rapid community health and needs assessment after hurricanes Isabel and Charley—North Carolina, 2003–2004. MMWR Morb Mortal Wkly Rep. 2004;53(36):840–2. [PubMed] [Google Scholar]
- 19.Patton MQ. 3rd ed. Thousand Oaks (CA): Sage Publications; 1997. Utilization-focused evaluation. [Google Scholar]
- 20.Yin RK. Case study research: design and methods. Newbury Park (CA): Sage Publications, Inc.; 1989. [Google Scholar]
- 21.North Carolina DHHS. Cherokee Legionnaires' update: another Legionnaires' case confirmed; public health continues to look for additional sources. [cited 2005 Oct 12]. [Press release, 2004 Oct 24.] Available from: URL: http://www.dhhs.state.nc.us/presrel/10-20-04.htm.
- 22.Goode B, O'Reilly C. Outbreak of Shiga toxin producing E. coli (STEC) infections associated with a petting zoo at the North Carolina State Fair—Raleigh, North Carolina, November 2004. [cited 2005 Oct 12]; Final report Available from: URL: http://www.epi.state.nc.us/epi/gcdc/ecoli/EColiReportFinal062905.pdf. [Google Scholar]
- 23.RAND Corporation. Center for Domestic and International Health Security. Technical report. Santa Monica: RAND Corporation; 2005. Exemplary practices in public health preparedness. [Google Scholar]
- 24.Centers for Disease Contol and Prevention (US). Cooperative agreement guidance for public health emergency preparedness. 2005. Jul 1, [cited 2005 Nov 1]. Available from: URL: http://www.bt.cdc.gov/planning/guidance05/
- 25.McDonald S, Swadener S. CA: Torrence; 2004. May 17, The process of preparing a public health department: bridging practice and academia. Presented at the Third UCLA Conference on Public Health and Disasters. [Google Scholar]
- 26.Turnock B. Public health preparedness at a price. New York: The Century Foundation; 2004. [Google Scholar]
- 27.Dowling KC, Lipton RI. Bioterrorism preparedness expenditures may compromise public health. Am J Public Health. 2005;95:1672. doi: 10.2105/AJPH.2005.070102. [Letter to the Editor] [DOI] [PMC free article] [PubMed] [Google Scholar]