STUDENTS IN PUBLIC HEALTH SURGE CAPACITY
Outbreaks of infectious disease can be resource-intensive and large outbreaks may require that public health agencies reassign staff to participate. Such reassignments disrupt other necessary work of the agency. The development of surge capacity can prevent such disruptions. Since 2000, when the Columbia University Center for Public Health Preparedness (CPHP) was founded, the New York City Department of Health and Mental Hygiene (DOHMH) and the Center have explored various possibilities for an academic school of public health to provide surge capacity for public health emergencies. Following the attacks of September 11, 2001, the CPHP collected and provided to DOHMH contact information for faculty and student volunteers, and began to consider ways to use the volunteers to assist in surge capacity.1,2
The CPHP is one of 26 such centers located in accredited schools of public health and funded by the Centers for Disease Control and Prevention (CDC). The specific mission of the academic CPHP program is to address the agency and workforce needs of state and local public health agencies associated with bioterrorism, infectious diseases, and other emergencies. It is part of a larger network of 50 centers in various academic settings and health departments. The network is coordinated by the CDC and the Association of Schools of Public Health (ASPH). The Columbia Center was founded in 2000, among the first four academic CPHP's in the country.
In 2004, DOHMH reached out to CPHP about the possibility of recruiting student volunteers to supplement regular DOHMH personnel during large infectious disease outbreaks. In the aftermath of the terrorist attacks of 9/11, DOHMH had recruited a small number of Columbia public health students to assist with data entry for syndromic surveillance, so DOHMH had experience utilizing students for surge capacity. Other volunteers presented themselves to DOHMH immediately following the attacks to offer assistance. However, in part because these volunteers lacked public health skills and training, it was not possible to use these volunteers at the time. A more formal student volunteer program that provided advance training and ongoing opportunities to use the training through routine infectious disease outbreaks seemed particularly appropriate, therefore, and began in the summer of 2004.
The program described in this article seeks to develop and maintain a pool of student volunteers that can be called upon to supplement regular DOHMH personnel during a large infectious disease outbreak. While the program in New York City was immediately inspired by the “Team Epi-Aid” program at the University of North Carolina Center for Public Health Preparedness,3,4 it also drew on the well-established connections between the DOHMH and the Columbia Center (and the Center's academic home, the Mailman School of Public Health).
The students serve in the Bureau of Communicable Disease, which is responsible for investigating more than 60 infectious diseases, as well as outbreaks of unknown disease if they appear to be of infectious etiology. The majority of the Bureau's outbreak investigations are small and involve foodborne disease or viral hepatitis. However, the Bureau has been involved in several large, high profile outbreak investigations, including the anthrax attacks of 2001,5 the initial introduction of West Nile virus into the United States in 1999,6 and the multi-state outbreak of cyclosporiasis due to contaminated imported raspberries in 1996.7 In addition, the Bureau has worked on other emergencies, including increased diarrheal illness after the blackout of August 2003,8 as well as having to be prepared for potential emergencies such as the possibility of imported SARS during the outbreaks in 2003.9,10
PROGRAM DESIGN
Design of the program centered around the functional role that the student volunteers would usually be called upon to fill: case interviewing. At the Mailman School of Public Health, students are educated in one of six departments that vary significantly in subject matter emphasis (biostatistics, environmental health, epidemiology, health policy and management, population and family health, and sociomedical sciences). However, students in the volunteer program were usually called upon to fill the functional role of case investigation interviewer, regardless of their specific educational interests. Therefore, we focused on competency-based training. Necessary steps include clarification of specific roles (emergency response), description of competencies, and design and evaluation of the training. This methodology is illustrated in the Competency to Curriculum Toolkit.11
For recruitment, faculty and staff in the Center reached potential volunteers through personal contacts, announcements in classes, flyers, and school-wide e-mails from the Dean of Students' office. Recruitment sessions were held at the school, but all training sessions were carried out at the DOHMH in order to start familiarizing the volunteers with the agency. All students were provided with a “Frequently Asked Questions” sheet (Figure 1), and additional questions were answered individually during the recruitment and training sessions.
Figure 1.
Frequently asked questions
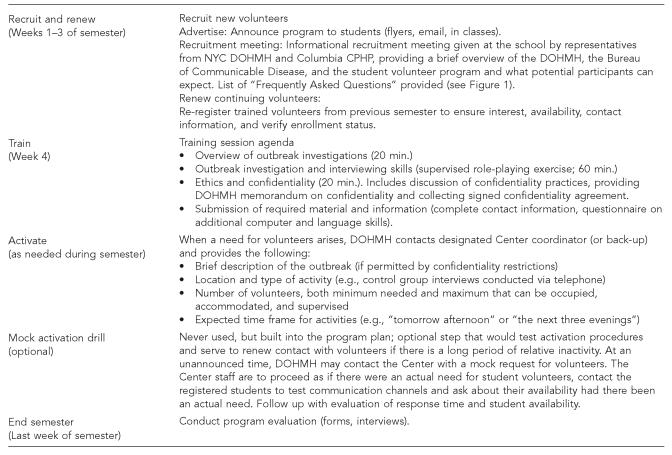
Training content and delivery were provided collaboratively by the DOHMH and the Center. The students in NYC received training in public health interviewing, confidentiality, and an orientation to the DOHMH operations and personnel as a supplement to their regular coursework. The case investigation and interviewing skills modules were based on materials that had originally been developed and used for cross-training staff in another partner health department of the Center. Training included brief lectures, but focused on scenario-based role-playing, with oversight and immediate evaluation by the instructor. The DOHMH provided an overview of their outbreak investigation process and the necessary confidentiality guidelines. Figure 2 shows the program cycle with operational details.
Figure 2.
Program cycle
After completing the short (roughly two- to three-hour) training, signing the confidentiality agreement, and providing phone and e-mail contact information, students were officially registered as members of the student volunteer team. A contact list of students was prepared, and whenever DOHMH needed their assistance they contacted students via e-mail with basic information on their immediate needs, including minimum and maximum number of students needed, preferred arrival time, and estimate of the amount of work to be done. This list was updated annually to remove students from the list who graduated or were no longer available to participate. Once the program was under way, experienced volunteers were given the opportunity to serve with the Bureau one or more afternoons a week. These students, or “Team Captains,” assisted in recruiting students for each new outbreak investigation, questionnaire development, and analysis of collected data, as well as in mentoring newer volunteers. Team Captains could also use this commitment to satisfy the School's practicum requirement.
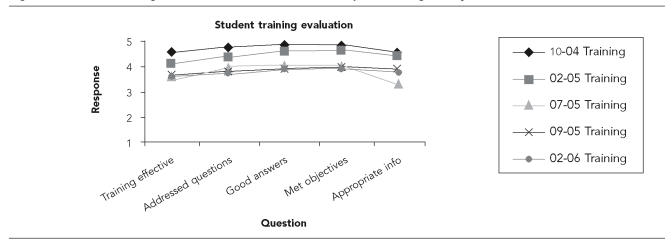
To evaluate the programmatic and training aspects, students completed questionnaires after the training (Figure 3) and at the end of each semester (Figure 4). These provided valuable feedback about instructor performance (some sessions had different instructors, with some relatively small differences in student feedback; Figure 3), relevance of training to actual duties, and barriers to serving. This information was used to improve the program the following semester. For example, in the fall 2004 survey, one student noted that there may be a delay between training and a volunteer's first activation. The lessons learned at the training, the student pointed out, may not be fresh in mind when assisting in an outbreak some weeks later. As a result, a set of slides based on transcripts of the training were created and made available on the web for download and review whenever a student needed them. [The slides are available at: http://www.ncdp.mailman.columbia.edu/video.htm, click on “Elements of an Outbreak Investigation (PPT)”.]
Figure 3.
Student training evaluation: selected results from post-training surveys
- Overall, how would you rate today's presentation? (1=Poor; 5=Excellent)
- The presenter allotted enough time to address questions. (1=Strongly disagree; 5=Strongly agree)
- The presenter answered questions competently. (1=Strongly disagree; 5=Strongly agree)
- The objectives of the session were met. (1=Strongly disagree; 5=Strongly agree)
- The information provided was useful to your work. (1=Strongly disagree; 5=Strongly agree)
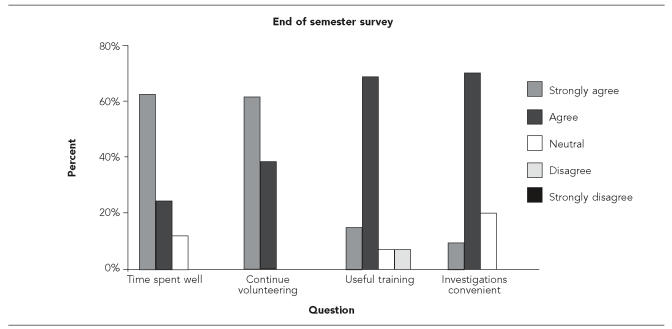
Figure 4.
Evaluation results, end of semester survey
- Once you reported to the site, your time was used well.
- Willing to continue in this program on a regular basis.
- The training at the start of the semester was useful.
- The timing of your field assignments was convenient.
PROGRAM OPERATION
After the training, students were immediately eligible to be involved in actual events, and they could apply the lessons learned in training. In particular, students came to understand some of the difficulties in acquiring epidemiologic information, and in cases where controls were necessary, the particular difficulties of locating appropriate controls. Some enrichment opportunities were also provided including the opportunity to work with DOHMH personnel on a study in a live poultry market in the city. Many of the students had heard of the live animal markets in Asia, and some were surprised to learn that live poultry markets could be found in the United States as well.
Students were most commonly asked to conduct interviews of either case-patients and/or controls. Most investigations were short, requiring just a few hours of assistance over one to three days. Although some investigations continued for several days or weeks, students committed the time they had available, which was usually a few hours. The program was flexible to allow for the other obligations and interests of the participants, most of whom were enrolled in full-time degree programs with a full course load, practicum, and possibly part-time paid work. Despite these concerns, timing of an outbreak did not prove a significant barrier or concern, although students were generally not available during exams and holidays. At the outset of the program, there was concern that disease outbreaks and other potential community emergencies occurring toward the end of the week or on weekends would prevent students from being available to assist when most needed. In practice, however, the pool of volunteers proved motivated and willing to conduct interviews from the DOHMH offices or from home regardless of when the emergency occurred. In fact, several students expressed an interest in volunteering more often as the number of volunteers exceeded the number of emergencies during a given semester, so it was not possible to call in all the volunteers who were registered each semester.
From the summer of 2004 when the program began through the spring semester 2006 after twenty months of operations, 124 students had been trained to participate in outbreak investigations. Currently 72 students are on the list of students who have indicated they are still active. Most of these students are at the Mailman School of Public Health; however, during the summer semester, students at a variety of schools who are participating in the New York City Department of Health and Mental Hygiene summer work study internship program (the Health Research Training Program or HRTP) are also eligible to participate. On average, requests for students have been made five times a semester, with a total number of 18 activations. These activations have included phone interviews of cases in foodborne outbreaks, face-to-face interviews of secondary school students, and individuals visiting live chicken markets to do pre- and post-intervention.
End of semester surveys showed that students found the program worthwhile and gratifying (Figure 4). In fall 2004 one student commented, “I think that there are a large number of Epi students who are interested in this type of work and I would be surprised if I were the only one who is considering making a career out of it.” Another student stated that, “After working on four investigations, I've learned about disease surveillance and how the health department keeps a watch over these things.” Typical of several students, one stated specifically that she joined since, “I am seeking to learn about surveillance and this is a useful first step.”
CONCLUSIONS
Local and state public health departments often require surge capacity during emergencies or unusually large outbreaks. Although staff and students at academic public health programs could serve as a potential source for surge capacity, many students in schools of public health do not have the opportunity to participate in public health emergency response or learn firsthand about many of the everyday aspects of public health practice. A program using student or faculty volunteers provides surge capacity for the health department at low cost, while providing the volunteers an opportunity to obtain experience in public health practice at a local health department.
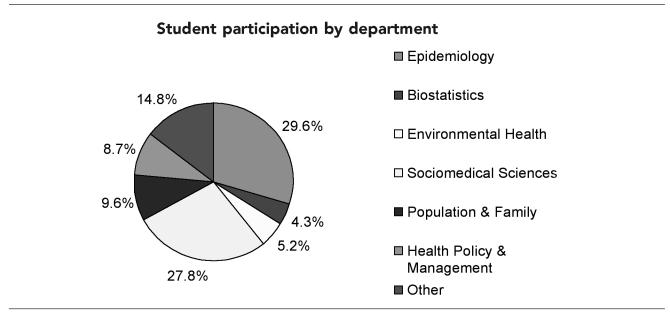
The program also provided a valuable supplement to the regular curriculum. All students of the Mailman School of Public Health are required to take at least two courses on epidemiology: an introductory level class and a methods class. Close to 30% of the student volunteers come from the epidemiology department (Figure 5), so all volunteers either have or are receiving significant education on the subject. However, there is a difference in studying outbreaks and investigating them. A research institution like the Mailman School typically involves students in research that can last several years. But the work volunteers perform with the Bureau of Communicable Disease is more immediate. Rather than studying large populations to find general health trends, volunteers deal with those directly affected by acute outbreaks. The work is done under a greater time pressure, with a need to apply the epidemiologic findings to guide public health interventions. These aspects of the work at the DOHMH expose students to lessons that cannot be taught in classrooms or via more academic research projects.
Figure 5.
Breakdown of student volunteers by academic department
Recently, the Institute of Medicine's Committee on Educating Public Health Professionals for the 21st Century recommended an expansion of supervised, practical, community-based experiences for students in the agencies in which they are training to function.12 By means of this program's integrative teaching techniques and the opportunity to assist with actual disease outbreak investigations, students gain on-the-ground knowledge of how a local public health agency functions. Participating in this program has enriched the students' educational experience, provided them with an opportunity for community service, suggested possible opportunities for other academic projects, and informed them of career options at a local or state public health agency. One student gained an internship position through the program and another gained both a summer job and employment during the winter and has since gone on to start a job in another health department.
While the student volunteer program did not overtly address bioterrorism preparedness, students were trained in very basic public health functions and given confidentiality training that is the basis of being able to respond to any public health emergency, whether a small foodborne outbreak or a larger crisis such as pandemic influenza or a bioterrorist attack. The surveillance and epidemiologic response to a bioterrorist event is similar to other infectious disease outbreaks with respect to case finding, interviews to ascertain risk exposures and clinical symptoms, and contact tracing to prevent further spread or to identify those in need of preventive measures.13 Although most of the work involved patient interviews (usually by telephone) and limited data entry, there have been discussions about expanded roles in the future, especially for the more experienced students or those with clinical experience. Potential roles include developing databases and questionnaires and possibly, in the case of large outbreaks like West Nile virus in 1999, assisting with some of the logistical aspects of the outbreak investigation. Other roles and tasks under consideration include chart abstraction (for clinical students), questionnaire design, data editing and analysis, and preparation of summary reports. In addition to outbreaks and other public health emergencies, students may assist in other public health projects such as field exercises on emergency preparedness, point of distribution exercises, or staffing public hotlines. The program is relatively labor-intensive in the initial stages, and then requires some staff time to maintain in terms of recruitment, maintaining up-to-date contact lists, and training students three times a year. Having the volunteers serve in more advanced roles would require additional oversight by DOHMH personnel.
The model described here involves training developed and delivered jointly with the health department, and has similarities (such as intensive faculty involvement) with the program developed at the University of North Carolina.3,4 The University of Texas has also recently developed a student volunteer program, S.E.I.S. (the Student Epidemic Intelligence Society), that is run as a formal student organization with dedicated resources including office space, telephone, and computers.14 Although a student volunteer program can take significant time for preparation and training, such programs could add significantly to developing both useful surge capacity for the health department and valuable experience for the students.
Acknowledgments
The authors thank Dr. Ngina Lythcott (Dean of Students, Mailman School of Public Health) and Mr. Brian Paquette (Assistant Dean) for indispensable help in planning and student recruitment; and Heather Cook and Dan Brown for their invaluable work in the program as student leaders. Heartfelt thanks to Dr. Marcelle Layton (Assistant Commissioner, NYC DOHMH).
REFERENCES
- 1.Morse SS. Building academic-practice partnerships: the Center for Public Health Preparedness at the Columbia University Mailman School of Public Health, before and after 9/11. J Public Health Manag Pract. 2003;9:427–32. doi: 10.1097/00124784-200309000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Morse SS, Qureshi K, Gebbie EN. Development of a public health surge capacity system from a pool of university health science campus employees. APHA 131st Annual Meeting. 2003 Nov 15–19; San Francisco, CA. Abstract 69496. [Google Scholar]
- 3.University of North Carolina, Center for Public Health Preparedness [cited 2006 Jul 12]. Team Epi-Aid. Available from: URL: http://www.sph.unc.edu/nccphp/teamepiaid.htm.
- 4.MacDonald P. Team Epi-Aid: graduate student assistance with urgent public health response. Public Health Rep. 2005;120(Suppl 1):35–41. doi: 10.1177/00333549051200S108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Update: investigation of anthrax associated with intentional exposure and interim public health guidelines, October 2001. MMWR Morb Mortal Wkly Rep. 2001;50(41):889–93. [PubMed] [Google Scholar]
- 6.Nash D, Mostashari F, Fine A, Miller J, O'Leary D, Murray K, et al. The outbreak of West Nile virus infection in the New York City area in 1999. N Engl J Med. 2001;344:1807–14. doi: 10.1056/NEJM200106143442401. [DOI] [PubMed] [Google Scholar]
- 7.Herwaldt BL, Ackers ML. An outbreak in 1996 of cyclosporiasis associated with imported raspberries. The Cyclospora Working Group. N Eng J Med. 1997;336:1548–56. doi: 10.1056/NEJM199705293362202. [DOI] [PubMed] [Google Scholar]
- 8.Marx MA, Rodriguez C, Greenko J, Das D, Heffernan R, Karpati A, et al. Diarrheal illness detected through syndromic surveillance after a massive power outage: New York City, August 2003. Am J Public Health. 2006;96:547–53. doi: 10.2105/AJPH.2004.061358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsang KW, Ho PL, Ooi GC, Yee WK, Wang T, Chan-Yeung M, et al. A cluster of cases of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348:1977–85. doi: 10.1056/NEJMoa030666. [DOI] [PubMed] [Google Scholar]
- 10.Poutanen SM, Low DE, Henry B, Finkelstein S, Rose D, Green K, et al. Identification of severe acute respiratory syndrome in Canada. N Engl J Med. 2003;348:1995–2005. doi: 10.1056/NEJMoa030634. [DOI] [PubMed] [Google Scholar]
- 11.Gebbie KM Competency-to-curriculum toolkit: developing curricula for public health workers. New York: Columbia University School of Nursing Center for Health Policy and Association of Teachers of Preventive Medicine; 2004. [cited 2006 Jul 12]. Available from: URL: http://cpmcnet.columbia.edu/dept/nursing/institutes-centers/chphsr/toolkit.pdf. [Google Scholar]
- 12.Gebbie KM, Rosenstock L, Hernandez LM, editors. Educating public health professionals for the 21st century. Washington: National Academy Press; 2003. Who will keep the public healthy? [PubMed] [Google Scholar]
- 13.Morse SS. The vigilance defense. Sci Am. 2002;287(4):88–9. doi: 10.1038/scientificamerican1002-88. [DOI] [PubMed] [Google Scholar]
- 14.University of Texas, Center for Public Health Preparedness. Student Epidemic Intelligence Society (SEIS) [cited 2006 Oct 1]. Available from: URL: http://www.sph.uth.tmc.edu/seis/