Abstract
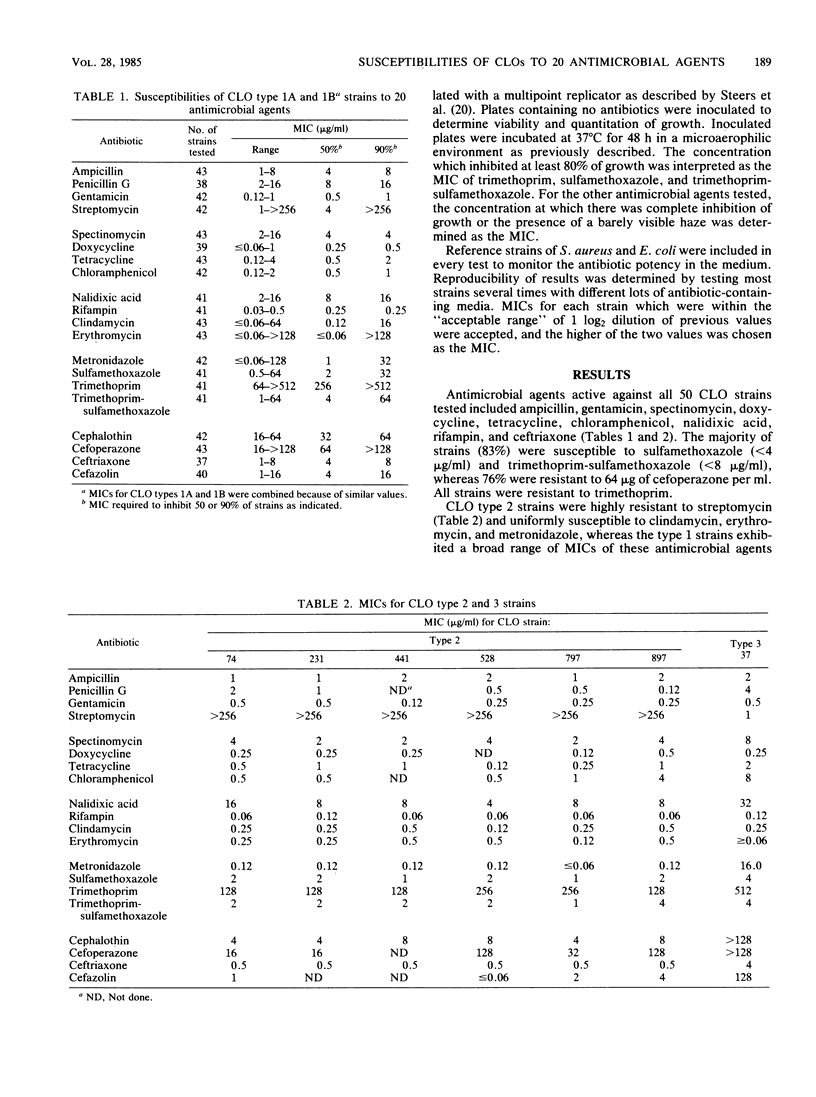
We determined MICs of 20 antimicrobial agents for 50 representative strains of four subgroups of Campylobacter-like organisms (CLOs) by agar dilution. Ampicillin, gentamicin, doxycycline, tetracycline, ceftriaxone, rifampin, spectinomycin, nalidixic acid, and chloramphenicol were active against all strains of CLOs. Most CLO strains (83%) were inhibited by 4 micrograms of sulfamethoxazole per ml and by 8 micrograms of trimethoprim-sulfamethoxazole per ml. Of type 1 strains, 28% were resistant to 8 micrograms of erythromycin per ml. In addition, cross resistance between erythromycin and clindamycin was always present. Type 1 strains exhibited a broad distribution of MICs of metronidazole and streptomycin, whereas all type 2 strains were uniformly susceptible to metronidazole and resistant to streptomycin. Unlike type 1 and 3 strains, type 2 CLOs were susceptible to cephalothin and penicillin G and highly resistant to streptomycin. The type 3 strain was uniquely resistant to cefazolin. The majority of strains were not inhibited by cefoperazone; and all were resistant to trimethoprim. In contrast to Campylobacter jejuni and Campylobacter fetus subsp. fetus, all CLOs tested were susceptible to 0.5 microgram of rifampin per ml.
Full text
PDF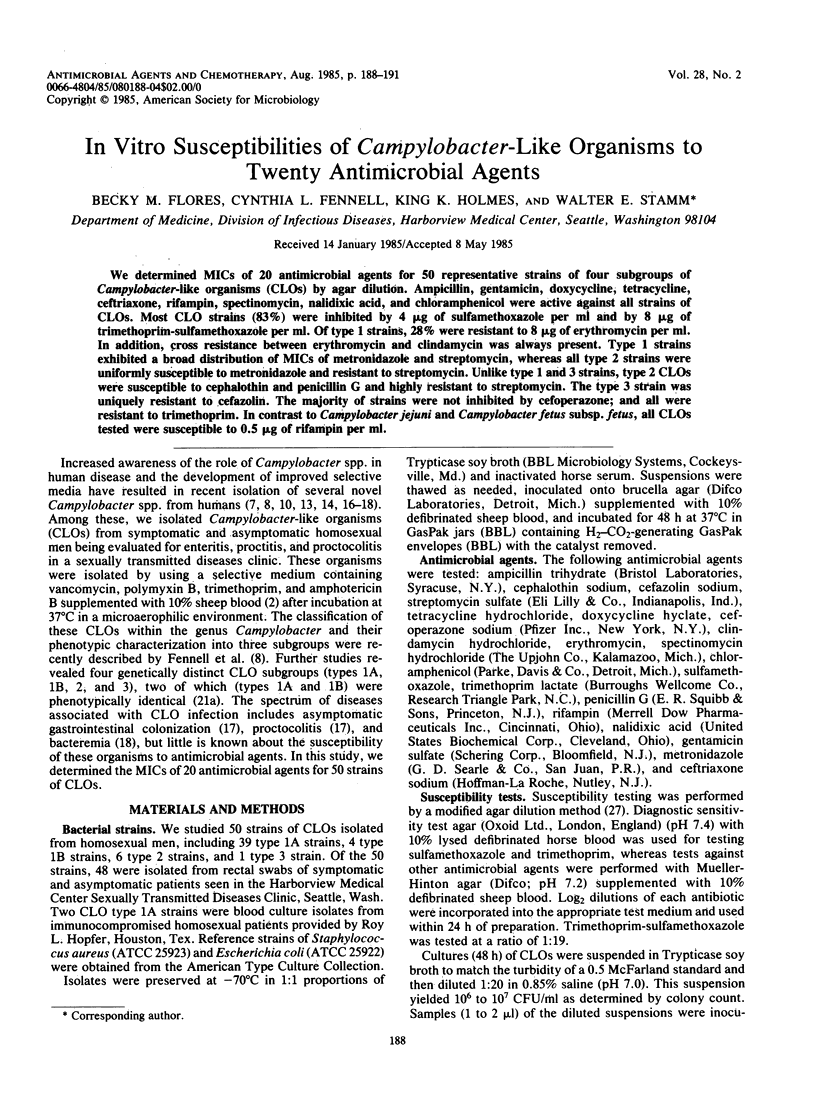

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ahonkhai V. I., Cherubin C. E., Sierra M. F., Bokkenheuser V. D., Shulman M. A., Mosenthal A. C. In vitro susceptibility of Campylobacter fetus subsp. jejuni to N-formimidoyl thienamycin, rosaramicin, cefoperazone, and other antimicrobial agents. Antimicrob Agents Chemother. 1981 Dec;20(6):850–851. doi: 10.1128/aac.20.6.850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaser M. J., Berkowitz I. D., LaForce F. M., Cravens J., Reller L. B., Wang W. L. Campylobacter enteritis: clinical and epidemiologic features. Ann Intern Med. 1979 Aug;91(2):179–185. doi: 10.7326/0003-4819-91-2-179. [DOI] [PubMed] [Google Scholar]
- Buck G. E., Kelly M. T. Susceptibility testing of Campylobacter fetus subsp. jejuni, using broth microdilution panels. Antimicrob Agents Chemother. 1982 Feb;21(2):274–277. doi: 10.1128/aac.21.2.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butzler J. P., Skirrow M. B. Campylobacter enteritis. Clin Gastroenterol. 1979 Sep;8(3):737–765. [PubMed] [Google Scholar]
- Chow A. W., Patten V., Bednorz D. Susceptibility of Campylobacter fetus to twenty-two antimicrobial agents. Antimicrob Agents Chemother. 1978 Mar;13(3):416–418. doi: 10.1128/aac.13.3.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devlin H. R., McIntyre L. Campylobacter fetus subsp. fetus in homosexual males. J Clin Microbiol. 1983 Oct;18(4):999–1000. doi: 10.1128/jcm.18.4.999-1000.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fennell C. L., Totten P. A., Quinn T. C., Patton D. L., Holmes K. K., Stamm W. E. Characterization of Campylobacter-like organisms isolated from homosexual men. J Infect Dis. 1984 Jan;149(1):58–66. doi: 10.1093/infdis/149.1.58. [DOI] [PubMed] [Google Scholar]
- Goossens H., De Boeck M., Butzler J. P. A new selective medium for the isolation of Campylobacter jejuni from human faeces. Eur J Clin Microbiol. 1983 Aug;2(4):389–393. doi: 10.1007/BF02019476. [DOI] [PubMed] [Google Scholar]
- Harvey S. M., Greenwood J. R. Probable Campylobacter fetus subsp. fetus gastroenteritis. J Clin Microbiol. 1983 Nov;18(5):1278–1279. doi: 10.1128/jcm.18.5.1278-1279.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karmali M. A., De Grandis S., Fleming P. C. Antimicrobial susceptibility of Campylobacter jejuni and Campylobacter fetus subsp. fetus to eight cephalosporins with special reference to species differentiation. Antimicrob Agents Chemother. 1980 Dec;18(6):948–951. doi: 10.1128/aac.18.6.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karmali M. A., De Grandis S., Fleming P. C. Antimicrobial susceptibility of Campylobacter jejuni with special reference to resistance patterns of Canadian isolates. Antimicrob Agents Chemother. 1981 Apr;19(4):593–597. doi: 10.1128/aac.19.4.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall B. J., Warren J. R. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet. 1984 Jun 16;1(8390):1311–1315. doi: 10.1016/s0140-6736(84)91816-6. [DOI] [PubMed] [Google Scholar]
- McNulty C. A., Watson D. M. Spiral bacteria of the gastric antrum. Lancet. 1984 May 12;1(8385):1068–1069. doi: 10.1016/s0140-6736(84)91469-7. [DOI] [PubMed] [Google Scholar]
- Michel J., Rogol M., Dickman D. Susceptibility of clinical isolates of Campylobacter jejuni to sixteen antimicrobial agents. Antimicrob Agents Chemother. 1983 May;23(5):796–797. doi: 10.1128/aac.23.5.796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nachamkin I., Stowell C., Skalina D., Jones A. M., Hoop R. M., 2nd, Smibert R. M. Campylobacter laridis causing bacteremia in an immunosuppressed patient. Ann Intern Med. 1984 Jul;101(1):55–57. doi: 10.7326/0003-4819-101-1-55. [DOI] [PubMed] [Google Scholar]
- Pasternak J., Bolivar R., Hopfer R. L., Fainstein V., Mills K., Rios A., Bodey G. P., Fennell C. L., Totten P. A., Stamm W. E. Bacteremia caused by Campylobacter-like organisms in two male homosexuals. Ann Intern Med. 1984 Sep;101(3):339–341. doi: 10.7326/0003-4819-101-3-339. [DOI] [PubMed] [Google Scholar]
- Quinn T. C., Goodell S. E., Fennell C., Wang S. P., Schuffler M. D., Holmes K. K., Stamm W. E. Infections with Campylobacter jejuni and Campylobacter-like organisms in homosexual men. Ann Intern Med. 1984 Aug;101(2):187–192. doi: 10.7326/0003-4819-101-2-187. [DOI] [PubMed] [Google Scholar]
- Shanker S., Sorrell T. C. Susceptibility of Campylobacter jejuni to twenty-three antimicrobial agents. Pathology. 1983 Jan;15(1):61–63. doi: 10.3109/00313028309061403. [DOI] [PubMed] [Google Scholar]
- Svedhem A., Kaijser B., Sjögren E. Antimicrobial susceptibility of Campylobacter jejuni isolated from humans with diarrhoea and from healthy chickens. J Antimicrob Chemother. 1981 Mar;7(3):301–305. doi: 10.1093/jac/7.3.301. [DOI] [PubMed] [Google Scholar]
- Totten P. A., Fennell C. L., Tenover F. C., Wezenberg J. M., Perine P. L., Stamm W. E., Holmes K. K. Campylobacter cinaedi (sp. nov.) and Campylobacter fennelliae (sp. nov.): two new Campylobacter species associated with enteric disease in homosexual men. J Infect Dis. 1985 Jan;151(1):131–139. doi: 10.1093/infdis/151.1.131. [DOI] [PubMed] [Google Scholar]
- Vanhoof R., Goossens H., Coignau H., Stas G., Butzler J. P. Susceptibility pattern of Campylobacter jejuni from human and animal origins to different antimicrobial agents. Antimicrob Agents Chemother. 1982 Jun;21(6):990–992. doi: 10.1128/aac.21.6.990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanhoof R., Gordts B., Dierickx R., Coignau H., Butzler J. P. Bacteriostatic and bactericidal activities of 24 antimicrobial agents against Campylobacter fetus subsp. jejuni. Antimicrob Agents Chemother. 1980 Jul;18(1):118–121. doi: 10.1128/aac.18.1.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanhoof R., Vanderlinden M. P., Dierickx R., Lauwers S., Yourassowsky E., Butzler J. P. Susceptibility of Campylobacter fetus subsp. jejuni to twenty-nine antimicrobial agents. Antimicrob Agents Chemother. 1978 Oct;14(4):553–556. doi: 10.1128/aac.14.4.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walder M. Susceptibility of Campylobacter fetus subsp. jejuni to twenty antimicrobiol agents. Antimicrob Agents Chemother. 1979 Jul;16(1):37–39. doi: 10.1128/aac.16.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]



