Abstract
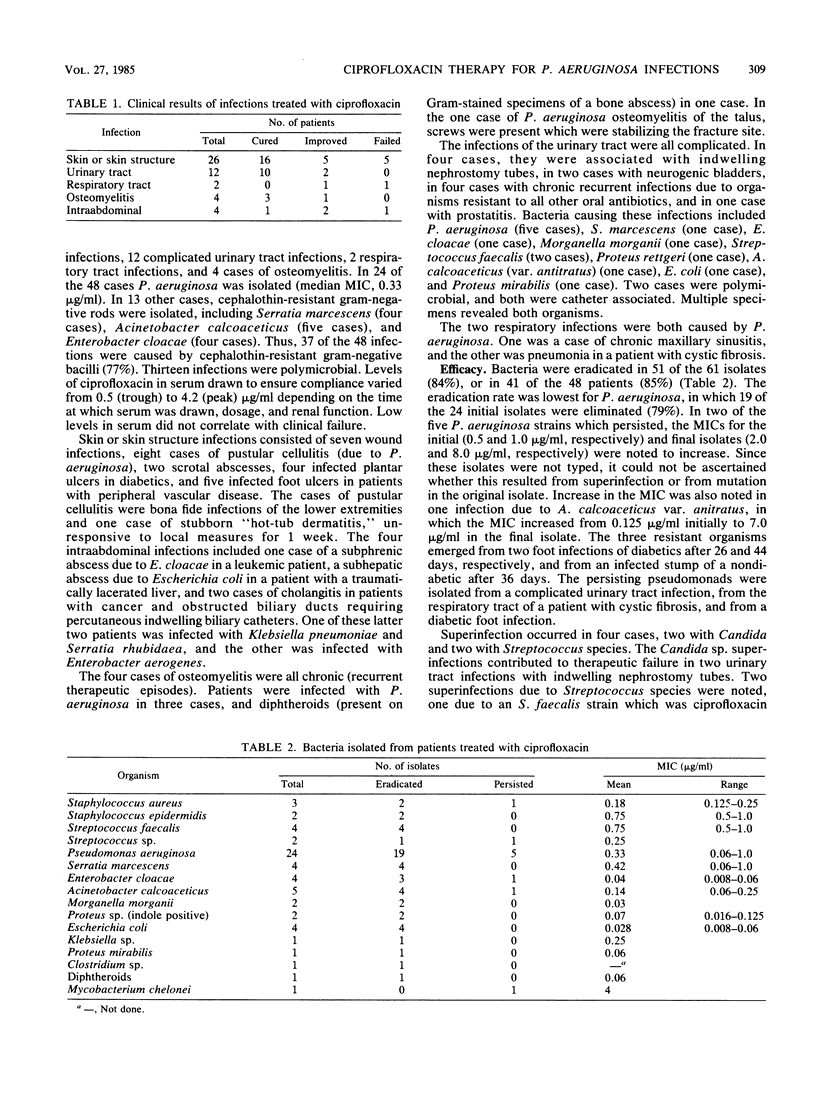
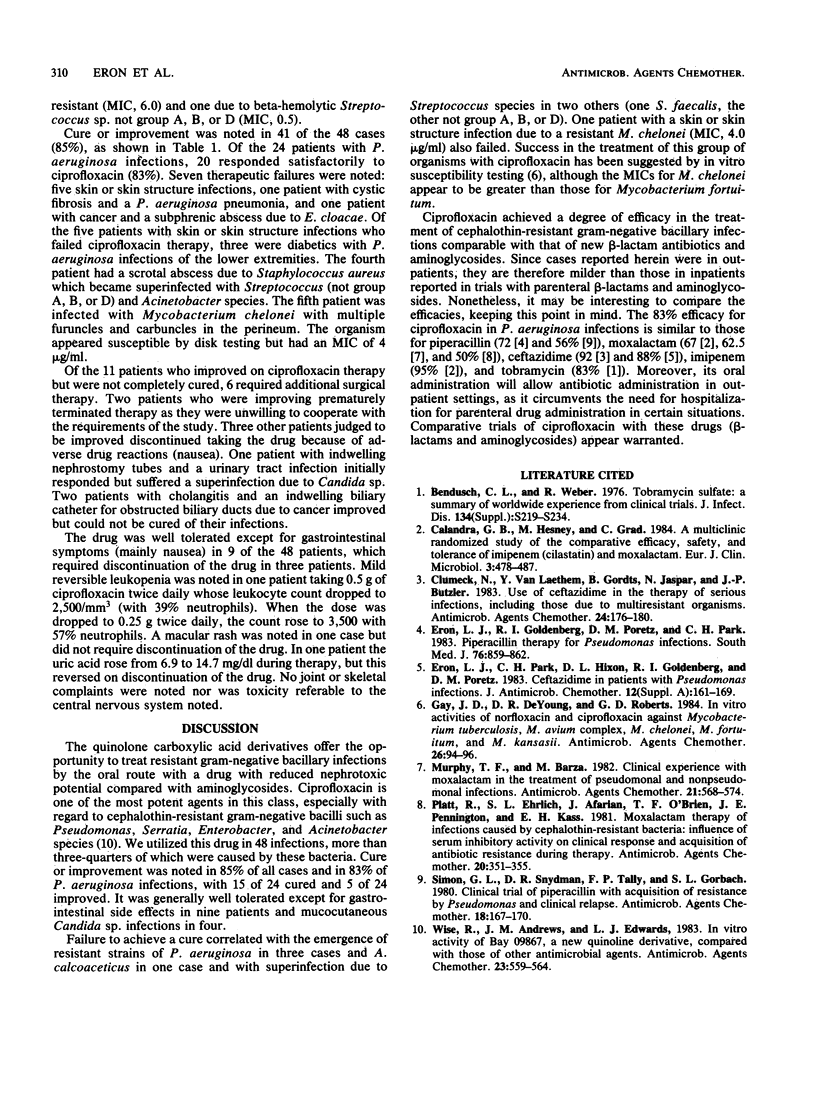
Ciprofloxacin was administered orally to 48 patients with 24 Pseudomonas aeruginosa infections and 13 other infections caused by cephalothin-resistant gram-negative bacilli. The types of infections treated included those of skin or skin structure, bone, urinary tract, and respiratory tract. In 83% of P. aeruginosa infections, a favorable clinical outcome occurred, compared with 85% for all infections. Failure to achieve a cure correlated with the emergence of resistant P. aeruginosa and Acinetobacter calcoaceticus strains in four instances and superinfection with Candida (two cases) and Streptococcus (two cases) species. Therapy was discontinued in three patients because of the development of nausea. Ciprofloxacin appears to be safe and effective in the therapy of infections caused by resistant gram-negative bacilli.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bendush C. L., Weber R. Tobramycin sulfate: a summary of worldwide experience from clinical trials. J Infect Dis. 1976 Aug;134 (Suppl):S219–S234. doi: 10.1093/infdis/134.supplement_1.s219. [DOI] [PubMed] [Google Scholar]
- Calandra G. B., Hesney M., Grad C. A multiclinic randomized study of the comparative efficacy, safety and tolerance of imipenem/cilastatin and moxalactam. Eur J Clin Microbiol. 1984 Oct;3(5):478–487. doi: 10.1007/BF02017380. [DOI] [PubMed] [Google Scholar]
- Clumeck N., Van Laethem Y., Gordts B., Jaspar N., Butzler J. P. Use of ceftazidime in the therapy of serious infections, including those due to multiresistant organisms. Antimicrob Agents Chemother. 1983 Aug;24(2):176–180. doi: 10.1128/aac.24.2.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eron L. J., Goldenberg R. I., Poretz D. M., Park C. H. Piperacillin therapy for Pseudomonas infections. South Med J. 1983 Jul;76(7):859–862. doi: 10.1097/00007611-198307000-00010. [DOI] [PubMed] [Google Scholar]
- Eron L. J., Park C. H., Hixon D. L., Goldenberg R. I., Poretz D. M. Ceftazidime in patients with Pseudomonas infections. J Antimicrob Chemother. 1983 Jul;12 (Suppl A):161–169. doi: 10.1093/jac/12.suppl_a.161. [DOI] [PubMed] [Google Scholar]
- Gay J. D., DeYoung D. R., Roberts G. D. In vitro activities of norfloxacin and ciprofloxacin against Mycobacterium tuberculosis, M. avium complex, M. chelonei, M. fortuitum, and M. kansasii. Antimicrob Agents Chemother. 1984 Jul;26(1):94–96. doi: 10.1128/aac.26.1.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy T. F., Barza M. Clinical experience with Moxalactam in the treatment of pseudomonal and nonpseudomonal infections. Antimicrob Agents Chemother. 1982 Apr;21(4):568–574. doi: 10.1128/aac.21.4.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platt R., Ehrlich S. L., Afarian J., O'Brien T. F., Pennington J. E., Kass E. H. Moxalactam therapy of infections caused by cephalothin-resistant bacteria: influence of serum inhibitory activity on clinical response and acquisition of antibiotic resistance during therapy. Antimicrob Agents Chemother. 1981 Sep;20(3):351–355. doi: 10.1128/aac.20.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon G. L., Snydman D. R., Tally F. P., Gorbach S. L. Clinical trial of piperacillin with acquisition of resistance by Pseudomonas and clinical relapse. Antimicrob Agents Chemother. 1980 Jul;18(1):167–170. doi: 10.1128/aac.18.1.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wise R., Andrews J. M., Edwards L. J. In vitro activity of Bay 09867, a new quinoline derivative, compared with those of other antimicrobial agents. Antimicrob Agents Chemother. 1983 Apr;23(4):559–564. doi: 10.1128/aac.23.4.559. [DOI] [PMC free article] [PubMed] [Google Scholar]



