Abstract
Objectives
To determine pharmacy faculty members' and students’ attitudes and perceptions regarding the use of complementary and alternative medicine (CAM).
Methods
A survey was used to obtain data on the following information concerning CAM: general attitudes, perceived barriers to use, training received and desired, personal use, and information sources used.
Results
In general, attitudes of pharmacy faculty members and students towards CAM were positive. Lack of evidence for CAM practices was considered the greatest barrier to the use of CAM by faculty members and students. Many CAM therapies were perceived to be effective. A high percentage of students desire more training in the areas of herbal medicine and nutritional supplements. Faculty members and students believe that CAM should be included in the curriculum.
Conclusions
General attitudes towards CAM are positive among pharmacy faculty members and students, and most believe that CAM should be taught in the pharmacy curriculum. More resources and training of faculty members may be necessary.
Keywords: complementary and alternative medicine, attitudes, students, faculty
INTRODUCTION
During the last 10 years, the use of various forms of integrative medicine by consumers has seen tremendous growth. Although nomenclature has continued to evolve, these alternative forms of healing have been collectively referred to as complementary and alternative medicine (CAM). Commensurate with the increase in consumer interest, the federal government has committed resources to study and address this area with the establishment of the National Institutes of Health (NIH) Center for Complementary and Alternative Medicine (NCCAM). The goal of this center is to “explore complementary and alternative healing practices in the context of rigorous science, training complementary and alternative medicine (CAM) researchers, and disseminating authoritative information to the public and professionals.”1
While consumer interest in CAM has continued to rise, mainstream schools of pharmacy, nursing, and medicine have been slow to embrace curriculum changes aimed at educating practitioners about alternative forms of healing. A number of factors may have contributed to the reluctance on the part of mainstream practitioners and academicians to either include CAM approaches in their practice or educate new practitioners about various CAM approaches that are gaining wide acceptance by consumers. Many practitioners cite “lack of scientific evidence” as a concern, while others simply admit that they are unfamiliar with many of the CAM approaches that their patients are using.2
As practicing clinicians and academicians have struggled with determining the emerging role of alternative therapies, students in mainstream academic centers have also recognized both the growth in and need for education related to CAM.2,3
Many schools of medicine and nursing have incorporated various components of CAM into their curricula, and schools of pharmacy are attempting to incorporate didactic coursework in their curricula related to CAM.3-7 In recent years, CAM education has improved in schools of pharmacy. Approximately 73%-86% of schools of pharmacy now offer some sort of CAM in the curriculum.6,7 However, they are primarily in elective courses, and generally focus on natural products rather than the full range of CAM-related practices.3,6,7 A very nice 5-part series on teaching evidence-based complementary and alternative medicine has been published, to which readers may want to refer.8-13
Since pharmacists are frequently cited as both accessible to patients and one of the most trusted healthcare professionals, patients routinely ask them for advice about a variety of CAM-related practices.14,15 For this reason, many believe that pharmacists must be better educated regarding CAM.14,15 Thus, determining pharmacists’ attitudes and perceptions toward the use of CAM plays an important role in how curriculum change could be accomplished. As part of an NCCAM curriculum development grant, the University of Minnesota College of Pharmacy participated in a college-wide survey to assess attitudes of both faculty members and students related to CAM.2 The goal of this study was to identify attitudes toward a full range of CAM practices so that strategies to adopt CAM-related curriculum change could be developed.
METHODS
Members of this NCCAM-funded curriculum development grant project created a 3-page survey instrument.2 The study was reviewed and approved by the Committee for Protection of Human Subjects of the Institutional Review Board (IRB) at the University of Minnesota.
Faculty members and students at the University of Minnesota College of Pharmacy were invited to participate in the study. Faculty members from all departments who were directly involved in the teaching mission of the College of Pharmacy were included. Students were fourth-year doctor of pharmacy students who were less than a month away from graduation. Self-report survey instruments, along with a cover letter and consent forms, were distributed to participants. The faculty members were made aware of the survey in department meetings and survey instruments were placed in mailboxes. The faculty members were asked to complete and return survey instruments and e-mail follow-up was made within 2 weeks of survey distribution to encourage participation. Survey instruments were distributed to students during a mandatory final class meeting and completed survey instruments were collected prior to the end of the class meeting.
The survey instrument used a 6-point Likert rating scale on which 1 represented very strong agreement and 6 represented very strong disagreement. The demographic sections of the faculty member and student survey instruments were slightly different to reflect variations in practice and experience, but were otherwise identical. The survey instrument was developed to assess attitudes towards the most common CAM practices (acupuncture, aromatherapy, bioelectromagnetic therapies, biofeedback, chiropractic, herbal medicine, homeopathy, hypnosis/guided imagery, massage, music, nutritional supplements, prayer/spiritual healing, meditation, rolfing, and therapeutic/healing touch). Regarding these CAM therapies, the following were assessed: general attitudes, perceived barriers, place in health care, perceived effectiveness, training received and desired, personal use, and information sources used.
For the summary of the data, descriptive statistics were used (eg, frequencies, standard deviations, means, minimums, maximums, and proportions). For the Likert responses, all responses with any degree of agreement were grouped together as positive responses, and all responses with any degree of disagreement were grouped together as negative responses. T tests and chi-square tests were used to analyze differences between faculty members and students, as appropriate. Results were considered to be significant when the p value was less than 0.05 (the alpha was set at 0.05). If there were missing data for a question, the percentages did not total 100% for that question. In order to retain the accuracy of the denominator, the percentages used included data missing for that question (all survey instruments considered valid were counted in the percentages). SPSS 6.1 was used for the analyses.
RESULTS
Survey response rates were 44% (31/70) for faculty members and 63% (63/100) for students. For faculty members, the mean age was 46 years (range 28-73 years) and the mean number of years on the faculty was 15 (range 1-40). For pharmacy students, the mean age was 27 years (range 23-37 years).
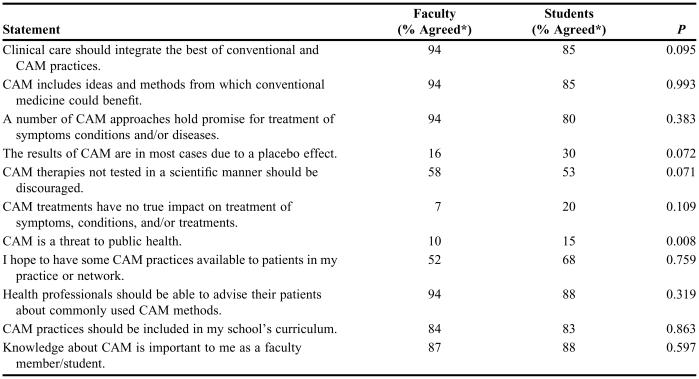
In general, attitudes of pharmacy faculty members and students towards CAM were positive (Table 1). A majority of faculty members and students indicated that CAM should be included in the curriculum (84% and 83%, respectively), that CAM knowledge is important to them (87% and 88%), and that health professionals should be able to advise their patients about common CAM methods (94% and 88%). Despite positive attitudes, 16% and 30% of faculty members and students, respectively, believed that the results of CAM were in most cases due to the placebo effect. Fifty-eight percent and 53% of the faculty members and students surveyed indicated a strong desire to see CAM therapies validated in a scientific manner.
Table 1.
General Attitudes Towards Complementary and Alternative Medicine Among Faculty Members and Senior Students in a Doctor of Pharmacy Program
*Percentages of agreed and strongly agreed responses were combined
CAM = complementary and alternative medicine
Significant differences were seen between faculty members and students for the belief that CAM is a threat to public health (10% vs. 15%; p = 0.008). Faculty members and students also differed in their belief that CAM treatments had no true impact on the treatment of symptoms, conditions, and/or treatments (7% vs. 20%), but this was not statistically significant.
The perceived barriers to the use of CAM are summarized in Table 2. The greatest perceived barrier was the lack of scientific evidence for the practices (faculty, 90%; students, 85%). Other barriers that ranked highly were lack of reimbursement (68% and 75%, respectively) and lack of staff training (81% and 75%, respectively).
Table 2.
Perceived Barriers to Use of Complementary and Alternative Medicine Reported by Faculty Members and Senior Students in a Doctor of Pharmacy Program
Significant differences between faculty members and students were seen for perceived barriers of CAM being too time consuming (19% vs. 28%; p = 0.022), and a lack of appropriate equipment (32% vs. 58%; p = 0.009). Perceived barriers that differed between faculty members and students but lacked significance were unavailability of credentialed providers (58% vs. 80%) and institutional concern about legal barriers (48% vs. 65%).
When comparing opinions about the place different CAM modalities have in healthcare, only chiropractic was clearly considered mainstream with more than 50% of the faculty members and students agreeing that it is considered a mainstream practice in healthcare (74% and 53%, respectively; Table 3). Other categories perceived as mainstream were nutritional supplements (48% and 53%) and massage (45% and 38%). Interestingly, only 13% and 28% of faculty members and students considered herbal medicine to be mainstream. CAM modalities that more than 50% of both faculty members and students agreed were clearly alternative medicine were aromatherapy and bioelectromagnetic therapies. Significant differences of opinion were observed between faculty members and students regarding their perceptions that the CAM practices of biofeedback (48% vs. 18%; p = 0.001), hypnosis/guided imagery (29% vs. 13%; p = 0.023), and meditation (23% vs. 8%; p = 0.01) were mainstream.
Table 3.
Opinions Regarding Place in Health Care for Common Complementary and Alternative Medicine Therapies Among Faculty Members and Senior Students in a Doctor of Pharmacy Program
*Significant difference (p < 0.05) between faculty and student perceptions
CAM = complementary and alternative medicine
CAM therapies that more than 50% of the faculty members identified as moderately or highly effective included acupuncture, biofeedback, chiropractic, herbal medicine, hypnosis/guided imagery, massage, nutritional supplements, and prayer/spiritual healing (Table 4). CAM therapies that more than 50% of the students thought were moderately or highly effective were acupuncture, chiropractic, herbal medicine, massage, nutritional supplements, and prayer/spiritual healing. Those therapies most frequently perceived by faculty members as being ineffective were aromatherapy (19%), bioelectromagnetic therapies (26%), and homeopathy (26%). In contrast, the percentage of students believing that a therapy was ineffective was less than 10% for all categories. The only area where the difference in perceived effectiveness was significant between faculty members and students was for chiropractic care (p = 0.009), which 90% of faculty members thought was moderately or highly effective compared with 63% of students.
Table 4.
Perceived Effectiveness of Complementary and Alternative Medicine Among Faculty Members and Senior Students in a Doctor of Pharmacy Program
F = faculty; S = student
*Significant difference (p < 0.05) between faculty and student perceptions
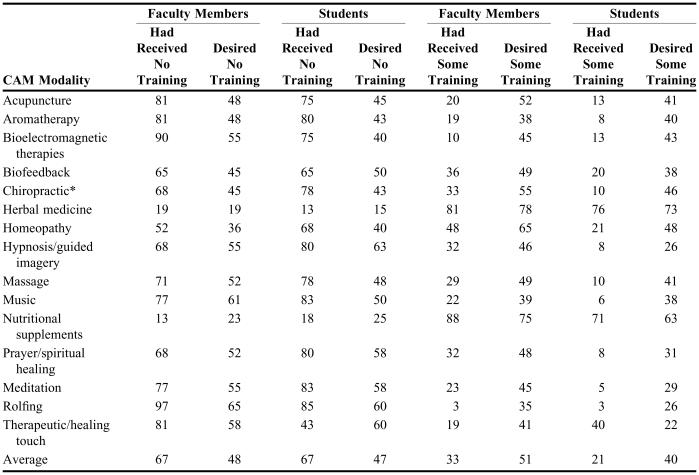
A summary of the CAM training that faculty members and students had received and future training they desired is presented in Table 5. Surprisingly, only about half of faculty members and a third of students were likely to have received training sufficient to personally provide or advise patients in herbal medicine (55% and 36%, respectively) and nutritional supplements (46% and 36%). The lack of CAM training in colleges of pharmacy is further evidenced by an average of 67 % of faculty members (range 13%-97%) and 67% of students (range 13%-85%) reporting no CAM training in all listed modalities. The only significant difference between faculty members and students in this area was in the percentage who had received training in chiropractic care (33% vs. 10%; p = 0.026).
Table 5.
Percentages of Faculty Members and Students Who Had Received and/or Desired Training in Complementary and Alternative Medicine
*Significant difference (p < 0.05) between faculty and student perceptions
The desire for further training was highest for herbal medicines (78% of faculty members and 73% of students) and nutritional supplements (75% and 63%). For the other categories, the desire for further training was less than 65% among both faculty members and students. Overall, 48% of faculty members and 47% of students indicated that they did not desire further training.
Table 6 summarizes personal use of CAM by faculty members and students. The CAM modalities with the highest percentage of positive outcomes experienced were chiropractic (26% for faculty members and 18% for students), herbal medicine (29% and 20%), massage (39% and 38%), nutritional supplements (32% and 35%), and prayer/spiritual healing (39% and 25%). Fairly high percentages of faculty members and students would consider using almost all CAM modalities (faculty members average, 45%, range 26%-68%; student average, 43%, range 30%-53%). Faculty members and students were most likely not to consider using bioelectromagnetic therapies (58% and 50%), homeopathy (61% and 43%), and rolfing (68% and 50%). The only significant difference between faculty members and students for personal use of CAM was for meditation. More faculty members than students would consider using meditation (61% vs. 48%) and more have used it with positive outcomes (19% vs. 5%) (p = 0.037).
Table 6.
Personal Use of Complementary and Alternative Medicine Therapies Reported by Faculty Members and Senior Students in a Doctor of Pharmacy Program
F = Faculty, S = Students
*Significant difference (p < 0.05) between faculty and student perceptions
Currently, pharmacy faculty members and students use a variety of sources to obtain information about CAM (Table 7). The sources most commonly used are pharmacy and other professional journals (90% and 70%, respectively) and peer professionals (87% and 65%). Other healthcare professionals, mass media, and the Internet were also ranked highly. Coursework or formal training was used by only 32% of faculty members and 38% of students. There was no significant difference in the information sources used by faculty members and students.
Table 7.
Sources of Information About Complementary and Alternative Medicine Used by Faculty Members and Senior Students in a Doctor of Pharmacy Program
*None of the differences between faculty and students were significantly different
DISCUSSION
This study suggests that students and faculty members consider it important for CAM to be included in the curriculum. They also agree that clinical care should integrate conventional and CAM practices and that CAM has methods from which conventional medicine could benefit. The small percentage that believe that CAM modalities have no true impact on the treatment of conditions or symptoms or that the results are due to placebo effect could be due to lack of information about current CAM evidence-based research. Students as well as faculty members agreed that any testing should be carried out in a scientific manner. Unfortunately, this study also showed that some faculty members and students still believe that CAM has a potential to harm. Nevertheless, a majority of faculty members and students believed that health professionals should be able to advise their patients about commonly used CAM methods. To do this successfully, knowledge about CAM practices should be included in the pharmacy curriculum. Both faculty members and students believe that lack of training is a potential barrier to use of CAM. In addition, they believe that the greatest barrier is the lack of scientific evidence. Therefore, training is needed in these areas, and curricula in colleges and schools of pharmacy should include this information. The training should include the evidence that is available. This would help faculty members and students to better advise their patients and to be more involved with other practitioners.
When considering whether CAM treatments were “mainstream” or “alternative” treatments, chiropractic care was ranked as mainstream by more faculty members and students than any other CAM practice. This could be due to health professionals being more familiar with chiropractic care as it has rapidly gained acceptance within the heath care system and is routinely reimbursed by government and third party programs. Use of nutritional supplements was also considered “mainstream.” Given the number of people who are currently using nutritional supplements as part of their health care, this was not surprising. More faculty members than students rated biofeedback as mainstream (48% vs 18%). This may be because faculty members are more familiar with this therapy and are aware that it is used in clinical practice.
The majority of faculty members and students perceived herbal medicine and nutritional supplements as highly effective or moderately effective. These findings could be due to a greater familiarity with these 2 topics than any of the others. Conversely, the very small percentage of faculty members and students who perceived rolfing as moderately or highly effective (7% and 11%, respectively) may have been due to their lack of familiarity with this treatment.
The training of health practitioners in CAM is a rapidly evolving area. However, due to the nature of pharmacy practice, many CAM modalities are not included in the training or curriculum. When study participants were asked to express their desire for training or further training in the use of a treatment, herbals and nutritional supplements received the highest percentage of positive responses. This indicates that more CAM content needs to be included in the education of pharmacists. The results of this study could lead the efforts of the College during their evaluation of the curriculum using these areas of interest from the perspective of faculty members and students.
Regarding personal use of CAM, both faculty members and students were open-minded about using different CAM modalities. Several CAM therapies had been used personally by the respondents with positive outcomes. This is important because personal beliefs or disbeliefs in a therapy may affect a health professional's advice to a patient, especially concerning CAM. For those therapies that faculty members and students would not consider, further education in these areas may affect their beliefs. They may not know enough about the therapy to use it.
This study also showed that coursework or formal training is the source of CAM information for only a small percentage of faculty members and students. This confirms that a majority of students feel that they are currently not obtaining CAM information from their coursework and the need for increased education on CAM therapies in the curriculum.
However, faculty members in colleges of pharmacy still may not feel comfortable with some content areas in CAM. The faculty members need to be well prepared to teach these topics. Perhaps if resources and training were made available to faculty members in schools of pharmacy, CAM could be more easily incorporated into the curriculum.
CONCLUSION
This study revealed that faculty members and students at the University of Minnesota College of Pharmacy acknowledge that CAM therapies can be beneficial and should be taught in the curriculum.
ACKNOWLEDGEMENTS
This work was supported by grant no. R25-AT00556 from the National Institutes of Health, National Center for Complementary and Alternative Medicine.
REFERENCES
- 1. National Center for Complementary and Alternative Medicine, National Institutes of Health. Available at: http://nccam.nih.gov/about/aboutnccam/index.htm. Accessed May 10, 2006.
- 2.Kreitzer MJ, Mitten D, Harris I, Shandeling J. Attitudes toward CAM among medical, nursing, and pharmacy faculty and students: a comparative analysis. Alternative Ther Health Med. 2002;8:44–53. [PubMed] [Google Scholar]
- 3.Mackowaik ED, Parikh A, Freely J. Herbal product education in United States pharmacy schools: core or elective program? Am J Pharm Educ. 2001;65:1–6. [Google Scholar]
- 4.Wetzek MS, Eisenberg DM, Kaptchuk TJ. Courses involving complementary and alternative medicine at US medical schools. JAMA. 1998;280:784–7. doi: 10.1001/jama.280.9.784. [DOI] [PubMed] [Google Scholar]
- 5.Reed FC, Petigrew AC, King MO. Alternative and complementary therapies in nursing curricula. J Nursing Educ. 2000;39:133–9. doi: 10.3928/0148-4834-20000301-08. [DOI] [PubMed] [Google Scholar]
- 6.Shields KM, McQueen CE, Bryant PJ. Natural product education in schools of pharmacy in the United States. Am J Pharm Educ. 2003;67:43–8. [Google Scholar]
- 7.Dutta AP, Daftary MN, Edba PA, Kang H. State of CAM education in U.S. schools of pharmacy: results of a national survey. J Am Pharm Assoc. 2003;43:81–3. [PubMed] [Google Scholar]
- 8.Mills EJ, Hollyer T, Guyatt G, Ross CP, Saranchuk R, Wilson K. Evidence-based Complementary and Alternative Medicine Working Group. Teaching evidence-based complementary and alternative medicine: 1. A learning structure for clinical decision changes. J Alternative Complementary Med. 2002;8:207–14. doi: 10.1089/107555302317371514. [DOI] [PubMed] [Google Scholar]
- 9.Wilson K, Mills EJ, Hollyer T, Vohra S, Guyatt G. Evidence-based Complementary and Alternative Medicine Working Group. Teaching evidence-based complementary and alternative medicine: 2. A conceptual approach to causation – Part 1. J Alternative Complementary Med. 2002;8:379–83. doi: 10.1089/10755530260128078. [DOI] [PubMed] [Google Scholar]
- 10.Wilson K, Mills EJ, Hollyer T, Vohra S, Guyatt G. Evidence-based Complementary and Alternative Medicine Working Group. Teaching evidence-based complementary and alternative medicine: 2. A conceptual approach to causation – Part 2. J Alternative Complementary Med. 2002;8:385–9. doi: 10.1089/10755530260128087. [DOI] [PubMed] [Google Scholar]
- 11.Wilson K, McGowan J, Guyatt, Mills EJ. Evidence-based Complementary and Alternative Medicine Working Group. Teaching evidence-based complementary and alternative medicine: 3. Asking the questions and identifying the information. J Alternative Complementary Med. 2002;8:499–506. doi: 10.1089/107555302760253702. [DOI] [PubMed] [Google Scholar]
- 12.Wilson K, Mills EJ, Ross C, Guyatt G. Evidence-based Complementary and Alternative Medicine Working Group. Teaching evidence-based complementary and alternative medicine: 4. Appraising the evidence for papers on therapy. J Alternative Complementary Med. 2002;8:673–9. doi: 10.1089/107555302320825192. [DOI] [PubMed] [Google Scholar]
- 13.Wilson K, Mills EJ, McGowan J, Guyatt G. Evidence-based Complementary and Alternative Medicine Working Group. Teaching evidence-based complementary and alternative medicine: 5. Interpreting the results of a study on therapy and applying them to a patient. J Alternative Complementary Med. 2002;8:867–73. doi: 10.1089/10755530260511856. [DOI] [PubMed] [Google Scholar]
- 14.Chang ZG, Kennedy DT, Holdford DA, Small RE. Pharmacists’ knowledge and attitudes toward herbal medicine. Ann Pharmacother. 2000;34:710–5. doi: 10.1345/aph.19263. [DOI] [PubMed] [Google Scholar]
- 15.Miller LG, Hume A, Harris IM, et al. White paper on herbal products. Pharmacotherapy. 2000;20:877–91. doi: 10.1592/phco.20.9.877.35200. [DOI] [PubMed] [Google Scholar]