Abstract
Quackery (promotion of products that do not work or have not been proven to work) was once a commonly used term within the pharmacy and medical communities. However, an increasingly anti-scientific national climate culminated in passage of the 1994 Dietary Supplement Health and Education Act, which granted unprecedented legitimacy to “dietary supplements” that had not been scientifically proven to be effective and/or safe. In part, this was facilitated when professional pharmacy magazines and journals published advertisements and articles promoting these unproven medications. Gradually, pharmacy codes of ethics eliminated references to quackery, and some pharmacy organizations seemed to accept the unproven medications they once exhorted the pharmacist not to sell. The profession's shift in attitude toward unproven medications occurred as the medical community at large began to realize the value of evidence-based medicine. Academicians must resist pressure to present unproven therapies as realistic alternatives for medications with scientific proof of safety and efficacy. They must stress the value of evidence-based medicine and urge students and pharmacists to recommend only those medications with evidence-based proof of safety and efficacy.
Keywords: quackery, dietary supplements, nonprescription products, homeopathy, complementary and alternative medicine
INTRODUCTION
The “new age” and hippie movements of the late 1960s aimed to demolish or replace traditional institutions, such as the government, religion, and organized medicine. In the latter, they have succeeded beyond their wildest dreams. With the collusion of the US Congress, medicine has entered a new “dark age” where scientific reason is undervalued and dismissed and quackery appears to have gained the upper hand. Several factors drove this startling trend. First, the US Food and Drug Administration (FDA) was rendered virtually impotent to combat quackery through the Machiavellian machinations of a sympathetic Senator with a financial interest in its growth (manufacturers of unproven products contributed to his campaigns).1 Second, vast numbers of Americans embraced unproven or “quack” medicines that lack evidence of efficacy (unproven medications are defined below). Third, unproven medicines were hawked by a politically powerful and wealthy supplement industry that purports to be a legitimate alternative to physician-based and scientifically proven medications and products.
Quackery was once a widely understood medical term used by pharmacists and the public.2 In 1963, an entire issue of the Journal of the American Pharmaceutical Association, entitled, “Medical Quackery,”3 was published which defined quackery as: “When an untrue or misleading health claim is deliberately, fraudulently, or pretentiously made for a food, drug, device or cosmetic…”4 This issue featured such articles as “Enforcement of Antiquackery Laws,” “Broadcasting Code Against Quackery,” “Campaign Against Quackery,” and “Investigation of Medical Quackery.” In a 1990 brochure entitled, “Quackery…The Billion Dollar Miracle Business,” the FDA, Federal Trade Commission (FTC), US Postal Service, Department of Health and Human Services (DHHS), and Pharmaceutical Advertising Council jointly defined quackery as “…the promotion of a medical remedy that doesn't work or hasn't been proven to work.”5
The term quackery is no longer used by the American Pharmacists Association (APhA) and has fallen into general disuse in pharmacy within the past decade. This Statement will refer to products that once would have fallen into that category as unproven medications. Unproven medications are those for which supporting data proving safety and efficacy have not been submitted to the FDA, according to the rigorous standards of the scientific method. Thus, for the purpose of this Statement, the term unproven medications includes dietary supplements, herbal medicines, and homeopathic medications, but excludes legitimate pharmaceuticals under active investigation (eg, investigational medications). By extension, unproven therapies encompasses medical therapies outside the realm of evidence-based medicine, such as pseudomedical devices, therapeutic touch, reflexology, iridology, naturopathy, traditional Chinese medicine, etc.
“LEGITIMIZATION” OF UNPROVEN MEDICATIONS
In general, community pharmacies sell 2 groups of medications. Pharmacists dispense prescription medications and recommend nonprescription products for which there is evidence of safety and efficacy, but may also sell unproven medications that lack data proving their safety and efficacy. The explanation for this dichotomy lies partly in federal law.
The National Center for Complementary and Alternative Medicine (NCCAM)
Prior to the 1990s, unproven medications were not fully accepted by society. However, in 1991, the efforts of several people led to the establishment of an Office of Alternative Medicine within the National Institutes of Health. The prime movers behind this were the Honorable Senator Tom Harkin of Iowa, who believed bee pollen had helped his allergies, and a constituent, Berkley Bedell, a believer in the ability of colostrum from the milk of a Minnesota cow to cure Lyme disease.6 The office eventually morphed into the National Center for Complementary and Alternative Medicine (NCCAM).7,8 Critics have charged that this is little more than a government boondoggle from the New Agers, designed to divert money from legitimate medical research to unproven therapies.9–11
The Dietary Health Supplement Education Act
Few pharmacy references have fully explored the rise of unproven medication following the establishment of the NCCAM. However, this author described how the concerted efforts of the health food store industry and the Honorable Senator Orrin Hatch of Utah ensured through their backing of the 1994 Dietary Health Supplement Education Act that the FDA would be virtually powerless in many areas to control sales of unproven medications.12 This retrogressive legislation prevented the FDA from requiring proof of safety or efficacy for unproven medications, as long as each container carried the required “dietary supplement” disclaimer in small print. It gave a green light to unproven medications so that tens of thousands of products were rushed to market to join in the profits.13,14 Companion web sites often offered glowing recommendations and testimonials for the unproven medications, eg, Focus Tincture and BrightSpark Tablets for autism, Focus ADHD for attention-deficit/hyperactivity disorder, gender specific products for fertility (Fertile XX for women, Fertile XY for men), and Detox Drops to eliminate toxins from the body.15–18 Sales of unproven medications increasingly referred to as “dietary supplements” increased to the extent that reports of serious injury (eg, severe hepatic injury with kava) and well-controlled studies that demonstrated lack of efficacy (eg, St. John's wort for depression) were virtually ignored.19,20 In testimony before the Senate, a physician referring to the results of the Dietary Health Supplement Education Act (DHSEA) said, “Under current law, I could literally pack capsules full of grass clippings from my lawn and market them as just about anything I liked.”9
THE ROLE OF CHPA
The Proprietary Association was formed in 1881 to protect the interests of patent medicine hucksters.21,22 In the ensuing years, it has undergone several name changes. The latest name change to the Consumer Healthcare Products Association (CHPA) was chosen specifically to indicate the organization's focus toward the nutritional supplement industry. At the time of the change, the organization boasted a membership of 75 manufacturers, 20-25 of which also manufactured dietary supplements. The organization's senior vice president stated that it would become the “lead voice in the area of dietary supplements.” CHPA intended to confer legitimacy on unproven medications by representing their manufacturers before the FDA, the FTC, Congress, state legislatures, state regulatory bodies, and international commissions. With its final name change, CHPA became closely allied with the move to legitimize unproven medications as “dietary supplements.”
PHARMACY EDUCATION'S DILEMMA
The passage of DSHEA and the efforts of CHPA were felt in pharmacy as universities struggled with the best means to educate students about unproven medications and therapies. Should the education include uses for which evidence of efficacy is lacking and doses whose safety and efficacy is unknown? Should it be restricted to adverse reactions and drug interactions? In seeking guidance to solve this dilemma, educators should consider such factors as the long tradition of a science-based curriculum, various and evolving pharmacy codes of ethics, nonprescription textbooks, and information found in pharmacy journals.
Science-Based Curriculum
One element of pharmacy education should be the scientific method, developed by Roger Bacon over 700 years ago. Strict application of this rigorous method is the gold standard in yielding the most reliable evidence. Pharmacy students should also be taught that the FDA applies the considerable power of this method in its quest to prove safety and efficacy of prescription medications prior to their approval. Any course in the history of pharmacy should also include a discussion of quackery, especially its widespread existence in America before the advent of the 1906 Pure Food and Drug Act, which crippled the patent medicine industry.12 Finally, pharmacy students should gain an appreciation of the long struggle to require manufacturers to invest funds in appropriate research to prove medications safe (via the 1939 Food, Drug, and Cosmetic Act) and effective (through the 1962 Kefauver-Harris Amendments to the Food, Drug and Cosmetic Act). Incidentally, both of these laws were soundly criticized by the nonprescription product industry (eg, the Proprietary Association) as they were being considered by Congress.
In medicine, application of the scientific method results in carefully considered decisions regarding which therapy to choose for each patient. Physicians weigh the evidence for efficacy in certain conditions against the risk of adverse effects to choose the most appropriate treatment option. With unproven medications, this decision cannot be made. Proponents of unproven products assert that they need not prove efficacy for any number of reasons, including that the products are natural and proof of efficacy is not required by law. However, virtually all lack proof of efficacy, because the required trials to prove efficacy have never been submitted to the FDA through submission of New Drug Applications. When proof of efficacy is lacking, any risk, no matter how remote, is too much to bear. A science-based curriculum for nonprescription products must teach students to apply these precepts when patients request unproven nonprescription medications. A curriculum that fails to do so may lead students to recommend unproven medications.
Pharmacy Codes of Ethics
Various pharmacy codes of ethics suggest an interest in appealing to the consciences of pharmacists who engage in quackery or in unethical practices. In 1848, the Philadelphia College of Pharmacy stated in its principles for conduct: “Whilst the College does not at present feel authorized to require its members to abandon the sale of secret or quack medicines, they earnestly recommend the propriety of discouraging their employment, when called upon for an opinion as to their merits.”23
The 1852 Code of Ethics of APhA stated that its members have agreed to “discountenance quackery and dishonorable competition in their business.”23 It also urged the “discontinuance of secret formulae and the practices arising from a quackish spirit.” The 1922 code stated that members should “discourage the use of objectionable nostrums.”6 It also stated that “The Pharmacist should hold the health and safety of his patrons to be of first consideration; he should make no attempt to prescribe or treat diseases or strive to sell drugs or remedies of any kind simply for the sake of profit…He should not accept agencies for objectionable nostrums nor allow his name to be used in connection with advertisements or correspondence for furthering their sale.”23 The 1952 code included the clause about health, safety, and profit; however, in lieu of the second clause, it substituted, “The pharmacist does not lend his support or name to the promotion of objectionable or unworthy products.”23 The 1969 and 1981 codes each contained a virtually identical clause: “A pharmacist should never knowingly condone the dispensing, promoting or distributing of drugs or medical devices, or assist therein, which are not of good quality, which do not meet standards required by law or which lack therapeutic value for the patient.” The current code (last updated in 1994), lacks any reference to quackery, nostrums, unworthy medications, medication quality, or medications lacking therapeutic value for the patient, including instead only a vague reference to telling the truth and acting with conviction of conscience.24 However, the APhA adopted the following value statement: “Integrity. We act in an honest, ethical, and transparent manner, and accept responsibility for our actions.”25
APhA publications feature advertisements for unproven medications. Further, the organization's conventions have included booths spotlighting unproven medications, such as a booth by Boiron, a leading manufacturer of homeopathic products, at the 1995 Annual Meeting.26 Speakers at various APhA-sponsored meetings have also presented programs that cast unproven products in a flattering light, failing to examine their shortcomings, such as a talk on herbals and homeopathy sponsored by Boiron at the 1995 APhA Annual Meeting.26 Thus, a close look at evolving pharmacy codes of ethics and the practices of a major national pharmacy association may leave students with a slanted view about selling unproven products.
Textbooks
Pharmacy students have limited opportunity to learn about the existence and extent of unproven medications and therapies in America. Because the medications and devices are available without prescription, one logical place to discuss it is within the context of a nonprescription medicines course. One of the leading texts in this area, the APhA-sponsored Handbook of Nonprescription Drugs (HND), did not include any chapter on unproven medications (eg, herbals, homeopathy, or dietary supplements) in any edition through the 10th edition (1993). In the 11th edition (1996), the HND included a chapter on “Herbs and Phytomedicinal Products,” co-authored by a leading pharmacognocist, and included only 73 references.
The 12th edition of HND (2000) included a new chapter on homeopathy. It also included a chapter on herbal remedies, grouped with the new homeopathy chapter in Section XI titled, “Alternative Therapies.” The preface of this edition indicated that “Some pharmacists may label discussions of alternative remedies slightly heretical, but patients voluntarily take these products, making it essential that pharmacists understand the philosophies of these remedies and the issues involved with the use of the specific products.” Suffice to say, there is no difficulty in demonstrating what homeopathy is so that the pharmacist can make an intelligent decision about homeopathic products and provide meaningful information to the patient. Unfortunately, while the authors indicated that the “efficacy of homeopathy remains controversial, it represents an alternative for patients who are without serious or life-threatening illnesses.” The chapter reflected a positive bias of its authors and its reviewers toward this unproven set of medications. The 13th edition of HND (2002) included homeopathic and herbal chapters in a section titled, “Complementary Therapies.” The homeopathy chapter was co-authored by a nurse/homeopath and once again lacked a critical, balanced view. The 14th edition of HND (2004) contained a section titled “Complementary and Alternative Medicine,” with the herbal and homeopathy chapters, and a new chapter on nonbotanical natural medicines. It retained the previous authors and some of the same reviewers for the homeopathy chapter and their positive biases toward the non—evidence-based practice. Subsequently, one of the authors had become a professor at a naturopathic college; the other was director of a school of homeopathy.
The growing acceptance of unproven medications by pharmacists may be due to the nonprescription textbook that faculty members choose for their students' use. One of the leading nonprescription products textbooks chose a homeopath and a professor of naturopathy to inform students about homeopathy in chapters that were not evidence-based. Textbooks with a positive bias toward unproven medications risk imparting this bias to the students who are required to purchase and study them.
Pharmacy Journals
Slowly, pharmacy journals began to publish papers on unproven medications and therapies in the 1980s, and the number of articles increased greatly in the 1990s as the US Congress legalized the widespread and unsupervised sale of these products through DSHEA. As companies (eg, Boiron) began to spend unprecedented advertising dollars on unproven medications, the tenor of articles in the pages of pharmacy journals concerning them rapidly became more favorable.
The APhA has several publications (other than their flagship nonprescription products textbook) that seemed to provide clues to the organization's attitude toward quackery and unproven medications. As previously stated, the organization's attitude against unproven medications and therapies in 1963 was sufficiently adverse to result in an anti-quackery-themed issue of the Journal of the America Pharmaceutical Association. In 1975, an editorial in the same journal bemoaned the New York Times' acceptance of laetrile for cancer.27 Apparently, the newspaper stated that laetrile may be ineffective, but at least it would be harmless. The editorial forcibly disagreed with the sale of ineffective remedies, even though they might be harmless. A look at the organization's more recent publications demonstrates that APhA's attitude may now be different. Various issues of APhA's Pharmacy Today have featured advertisements touting homeopathic products such as zinc lozenges for colds; a contributing writer who is a naturopath writes a column entitled “Alternative Medicine.”28 In the August 2005 issue of Pharmacy Today, the “Product Showcase” featured the homeopathic product “Complete Flu Care 4 Kids.”29 The manufacturer was not required to include a list of the product's ingredients in the advertisement; however, a visit to the company's web site revealed that it contains herbs, potassium iodide, and duck heart/liver.30 According to the precepts of evidence-based medicine, none of the ingredients has been demonstrated to ameliorate the symptoms of influenza in adults or children, and especially not when highly diluted according to homeopathic principles. In featuring this supplement for children with influenza, the APhA appears to be endorsing its efficacy. In the September 2005 issue of Pharmacy Today, APhA touted black cohosh for menopause symptoms and published a naturopath-authored article on green tea's purported benefits in slowing the growth of bladder, breast, and rectal tumors, all actions not grounded in evidence-based medicine.31,32
American Druggist featured a column entitled “On Nutrition” from 1985-1988. The author, William H. Lee, was described as a “master herbalist.” The poorly referenced columns presented credulous discussions on such topics as valerian for stress, feverfew for migraine, ginkgo for the side effects of aging, and algae for infections. In 1996, American Druggist favorably profiled a pharmacist who had developed a partnership with an acupuncturist, an alliance that had helped his bottom line.33 A 1997 column described the efforts of RiteAid Pharmacies to become the “premier source for vitamins, minerals, and herbs…” by providing reference binders on each topic to its 15,000 pharmacists.34 In 1998, American Druggist published an article entitled, “Integrating Herbal Therapy Into Practice.”35 Before it ceased to exist, this journal provided helpful advice/guidance to the pharmacist in selling unproven medications and therapies.
Pharmacy Times has included numerous references to unproven therapies. A 1983 article was titled, “Why Many ‘Health Foods’ are Not Safe and Effective.”36 It explored the ethical dilemma pharmacists faced in recommending products lacking in scientific evidence of safety, such as herbs. However, in 1995, the magazine inaugurated a column entitled “Pharmacists & Natural Medicine,” written by Constance Grauds, described as president of the Association of Natural Medicine Pharmacists. The columns often featured the address and web site of the organization to facilitate readers' joining. Her columns appeared as late as 2000. The unreferenced or sparsely referenced articles were uncritical of unproven medications, endorsing feverfew for arthritis, milk thistle as a “potential life-saver,” selenium for prostate cancer, and aromatherapy (eg, lavender) for burns, sores, and ulcers.37–40 In 1997, a Pharmacy Times article recommended natural medicines as a “rare opportunity for pharmacists.”41 A 1998 article asked, “Modern and Traditional Medicines: Can They Coexist?”42 The article answered its own question in the affirmative. Adversarial letters from readers in 1997 and 1999 equated the use of unproven herbs to playing chemical Russian roulette and also bemoaned that the trust of pharmacists was being sacrificed to the sales of unproven snake oils.43,44 The latter author asked the magazine's readers rhetorically, “Do you really have your customers' best interests at heart?” The August 2005 issue of Pharmacy Times offered coverage of a potpourri of unproven medications and therapies: an article featuring homeopathic antisnoring tablets and sprays, “news” about a $64.99 product for hair loss containing squash seed oil and other unproven ingredients, an advertisement for an unproven supplement containing biotin, alleged to help grow healthy nails, and an informative article about unproven therapies for diabetes.45–48
U.S. Pharmacist published an article critical of quackery in 1991.49 It also published a series of articles on alternative medicines from 1998-2003. The series had no regular author, although several wrote more than one monograph. The articles presented a more critically balanced examination of herbs (eg, evening primrose, kava-kava, hawthorn) than many others, attempting to find evidence of safety and efficacy. However, 2 articles published in 2002 and 2003 presented uncritical, non—evidence-based views of traditional Chinese medicine, authored by a “Practitioner of Oriental Medicine.”50,51
Drug Store News claimed to reach 70,000 chain drug pharmacists with articles that frequently covered unproven medications, including one by a homeopath recommending unproven supplements such as borage oil and flax oil for menstrual cramping and menopausal complaints.52,53 Another commended such “OTC giants” as Warner-Lambert, SmithKlineBeecham, and American Home Products for jumping on the herbal bandwagon with such products as herbal teas and supplements.54 A 1998 advertisement recommended “Blood Tonic Syrup,” which it described as “a Chinese herbal supplemen (sic) liquid composed of nine herbs and honey that promised to promote production of all 3 types of blood cells, naturally relieving anemia without side-effects.”55 It is interesting that Asian patient medicines have been implicated in recent years as contaminated with undeclared pharmaceuticals such as ephedrine, chlorpheniramine, methyltestosterone, sildenafil, and digoxin, and may also be contaminated by heavy metals (eg, mercury, lead, arsenic), the amounts of which exceed USP limits.
Drug Topics coverage of unproven medications and therapies also increased in the mid-1990s. A 1996 article aimed to prepare pharmacists for “CAM” counseling by providing guidance to continuing education (CE) courses and web sites and advised pharmacists about obtaining credentials for homeopathy, acupuncture, and naturopathy.56 A 1997 continuing education (CE) article exhorted pharmacists to “get their heads out of the sand and learn more about these alternative treatments.”57 The same year, an article favorably highlighted unproven homeopathic lozenges for colds that were said to be “taking the nation by storm.”58 In 1998, a 12-page supplement explored the role of glucosamine and chondroitin for arthritis, sponsored by a “nutraceutical company.”59 In a 1998 cover story, the magazine asked, “Alternative Medicine? How Bountiful is the Harvest? Where Does It Fit in the Pharmacy?”60 In the conclusion, its author asked whether pharmacists should “cash in on this very ancient, yet very new, dimension of medicine?” The author answered the question with an unequivocal, “You bet.” She cited data confirming that 84% of survey respondents agreed that the business should not be lost to other outlets. The appeal was mainly that, “It's a highly profitable arena that may cover financial deficits felt in the prescription department.” The article clearly presented the attraction of unproven medications to scientifically trained pharmacists: when a pharmacy is in financial trouble, it makes sense to begin selling unproven medications, stealing patients from such outlets as health food stores and supermarkets. The journal confirmed that viewpoint in a 1998 profile of a pharmacist with “stunning success” in promoting alternative medicine who stated, “I make more money off the acidophilus than I do off managed care third-party payments.”61
In response to an editorial disapproving of alternative medicine in the New England Journal of Medicine (NEJM), Drug Topics gave ample space to the vice president of the America Herbal Product Association, allowing him to refute the NEJM physician authors' viewpoints.62,63 In 1998, Drug Topics also featured a pharmacist with such “degrees” as DHM, DHPh, and NMD.64 He asserted that “…the medical community is starting to look at supplements as a ‘first line of defense’…The challenge becomes being able to increase sales by educating the consumer…” Three 1999 articles furthered the magazine's growing trend to embrace unproven products. One discussed continuing one's education by featuring unproven products and favorably discussing several organizations devoted to them (eg, American Botanical Council, American Association of Homeopathic Pharmacists).65 In a cover story, the journal also urged pharmacists, “Don't miss this boat,” an apparent metaphor for the marketing opportunity presented by unproven therapies.66 This article quoted a faculty member who described the revamping of a university course in order to “…(bridge) the gap between mainstream Western medicine and some of the products currently being recommended and used by people in the herbal product area.” The course apparently intended to help students view unproven medications and therapies in the same light as medications and therapies proven to be safe and effective, thereby blurring the line between evidence-based medicine and mere anecdote. A third 1999 article profiled a pharmacist/pharmacy owner whose recommendations of complementary products for such serious conditions as Epstein-Barr virus and chronic fatigue syndrome had moved from skeptical to confident, reporting that his profits had doubled since he introduced these unproven therapies.67 This practitioner also hired a massage therapist who practiced 2 unproven therapies (ie, therapeutic touch and reflexology), and promoted his pharmacy as “The Bridge Between Traditional and Holistic Remedies.” In a fourth 1999 article, Drug Topics revealed that RiteAid had formed a partnership with General Nutrition Companies (GNC) that would result in the chain opening full-line GNC health food stores inside 1,500 RiteAid stores.68 One CE article critical of unproven medications and therapies did appear in Drug Topics in 2001.69 However, the magazine quickly published 2 letters critical of that article. One reader (who did not reveal his dual roles as a coeditor of the Journal of the American Nutraceutical Association and homeopathic medicine manufacturer) complained that the article critical of unproven medications was “biased.” But in a refutation, the original author responded that he relied on current scientific data.65,70,71 Another reader (who described herself as a PharmD with a postdoctoral degree in traditional Chinese medicine) attempted to confer legitimacy on the unproven medical system known as traditional Chinese medicine.”72
The National Community Pharmacists Association has also included unproven medications in its publications. In 1989, it published an advertisement from Boericke and Tafel, Inc, for “Alpha CF,” an unproven homeopathic remedy that promised to aid in preventing cold and flu by stimulating “the body's own natural defense system--the immune system--to help ward off the attack.”73
Publishing is expensive and advertisements help underwrite the cost of publication. However, the nation's leading pharmacy journals have a duty to their readership to present a balanced and critical look at the content of their articles. When the duty to its readers and the duty to its sponsors are in conflict, advertisement-supported journals may be defaulting on their professional responsibility and presenting articles and other materials that offer uncritical coverage of the unproven medications and therapies advertised in its pages, thereby undermining the national push toward evidence-based medicine.
LICENSURE/ACCREDITATION ISSUES
The North American Pharmacist Licensure Examination (NAPLEX) has been accepted by the pharmacy boards in all 50 US states, 4 US territories (ie, Guam, Puerto Rico, the Virgin Islands, and the District of Columbia), 8 Canadian provinces, New Zealand, 2 Australian states, and South Africa as a unique tool to determine whether a pharmacy graduate is competent to enter the practice of pharmacy. The National Association of Boards of Pharmacy (NABP) expressed concern about lack of safety and efficacy data on herbal supplements in 1999.74 This concern culminated in NABP's decision to survey colleges of pharmacy to determine the extent to which dietary supplements were taught; as of 2000, 41 colleges included instruction on herbal products.75 As a result, NABP included herbal-based questions on NAPLEX, beginning in April of 2003.75,76 The questions were to be limited to efficacy, adverse effects, toxicities, and drug interactions. NABP stated it would use the United States Pharmacopoeia (USP) and National Foundry (NF) and professional journals as sources. Yet, as indicated previously, pharmacy journals may be biased in their presentations of dietary supplements and other unproven medications and therapies by advertising revenue.
The Accreditation Council for Pharmacy Education (ACPE)
ACPE is the organization that accredits pharmacy degree programs.77 It develops accreditation standards and guidelines for professional pharmacy programs. The latest Accreditation Standards and Guidelines were adopted on January 15, 2006.78
In a preamble to the document, ACPE stated that the newly revised standards focus on the development of the highest level of ethical behavior. Further, in the “Standards for Curriculum” the document stated, “As recommended by the Institute of Medicine for all health care professionals, pharmacists must be educated to deliver patient-centered care as members of an interprofessional team, emphasizing evidence-based practice……” A reader could justifiably conclude that the organization wishes for pharmacy to be an ethical profession in which medications and therapies are recommended by pharmacists based on scientific evidence of safety and efficacy.
The above conclusion is difficult to reconcile with certain aspects of the document. Appendix 2 provides “elements of the science foundation that…(are)…essential to the development of pharmacists” in a list of “areas critical to the foundation and delivery of effective patient care.” It includes a section entitled “Pharmacognosy and Alternative and Complementary Treatments.” Suggested topics include dietary supplements (eg, vitamins, minerals, herbals), alternative medical treatments, herbal-drug interactions, and the DSHEA and its impact on regulation of dietary supplements and herbal products. ACPE does not suggest that degree programs adopt either a positive or a negative stance with regard to unproven medications and therapies. Some might argue, however, that teaching students to adopt a positive stance about products not known to be safe or effective would be construed as unethical behavior, violating a primary focus area for the new standards, and would also violate the elementary precepts of adherence to evidence-based medicine.
How might degree programs attempt to meet the draft standards without proscriptive requirements or more clearly elucidated guidance regarding teaching of unproven medications and therapies? In a 1998 survey, investigators determined that a sizeable number of pharmacy schools used alternative practitioners themselves as supplemental instructors.79 This approach is not recommended, as it is virtually guaranteed to give students a biased attitude, unless it is counterbalanced by an authoritative professor or authority able to discuss each topic in the context of evidence-based medicine. This author was once asked to review a paper submitted for publication in a leading pharmacy journal describing the development of a course in alternative/complementary medicine. The course opened with a ceremony conducted in a “shamanic” tradition (a shaman is a “medicine man” or “priest or priestess”) to set the mood for exploration into unknown territories. Further, it invited alternative practitioners engaging in unproven medical systems (eg, Ayurveda, Reiki, tai chi, qi gong, chakras, aromatherapy, homeopathy, Chinese medicine, herbals, naturopathy, chiropractic) as lecturers to “reinforce the importance of integrative medicine,” and closed with a shamanic medicine ceremony. The course was seemingly void of lecture time discussing lack of evidence for unproven medications and therapies and the ramifications for patients.
PHARMACIST JUSTIFICATIONS
Pharmacists who recommend unproven medications and therapies have developed many self-justifications for doing so, such as consumer demand, profits, and seeming endorsement by national pharmacy organizations and pharmacy journals. However, each presents specific challenges to professionalism.
Justification 1: Pharmacists Should Sell Unproven Products to Satisfy Consumer Demand
Pharmacists who stock and recommend unproven medications and therapies may have justified this as meeting a consumer need. In a 1999 article in Drug Topics, this argument was used to good effect. It stated, “A nationwide survey of 2,039 US households found that 85% of the population is using some form of alternative medication.”65 These statistics provided justification for the article's recommendations to pharmacists to read alternative medicine journals and take CE courses offered by alternative medicine supporters.
In light of this argument, some pharmacists are convinced that consumers will gain access to unproven medications and therapies whether they stock them or not. So, the thinking goes, “I might as well make the profit as the health food stores.” However, pharmacists may not fully understand the liability issues they assume when selling unproven products. Merely having them on the shelves of a pharmacy is an implied warranty of safety and efficacy, a difficult position to defend legally given that the manufacturers of these products have proven neither to the FDA. Making any verbal claim as to their action (eg, “Milk thistle is good for toxic liver damage”) constitutes an express warranty. Both types of warranties open the pharmacist to liability, although the latter is more serious. When the liability aspect is considered, it makes less sense to stock unproven medications to keep profits high.
Other pharmacists state, “I will be able to advise my patients about the use of unproven medications and therapies better than any health food store employee.” Undoubtedly, that is true. However, should the pharmacist present a credulous defense of the product or recommend it, the liability issue arises again. Further, many patients select and purchase nonprescription items without speaking to the pharmacist, so there is no opportunity to advise the patient.
Justification 2: Unproven Medications Are Profitable
For pharmacist and pharmacies, as previously mentioned, this may be the only argument that is necessary to mentally justify sales of unproven medications and provide recommendations for unproven therapies. However, it strikes at the core issue at which this manuscript is directed: Are pharmacists businesspeople or healthcare professionals? If pharmacists are strictly one or the other, our respective courses are clear. Nonprofessional businesspeople sell products, but healthcare professionals should always hold as their primary obligation a duty to the patient to be above reproach. Pharmacies with serious survival issues may choose to submerge their professionalism to recommend unproven medications and therapies for financial gain. Their payoff is survival of the pharmacy and possible recognition in Community Pharmacist or in Drug Topics' annual issue devoted to to pharmacists who have achieved success through promoting unproven therapies.80,81 On the other hand, pharmacists who view themselves first and foremost as professionals should refuse to sell unproven medications and recommend unproven therapies, no matter what the ramifications might be.
Justification 3: Endorsement by National Organizations and Magazines Confers Legitimacy on Unproven Products
Pharmacists may believe that the presence of booths touting unproven medications at conventions for national professional organizations and the inclusion of advertisements for unproven medications in professional magazines gives these products a degree of legitimacy. Popular pharmacy magazines are critically dependent on advertisers and organizations are critically dependent on sponsor funding to survive. Manufacturers of unproven medications and therapies are potent sources of revenue. Thus, it is instructive to look at the advertising pages of pharmacy magazines for the presence of advertisements for unproven medications. Further, when one attends the national conventions of pharmacy organizations, it is helpful to visit the booths in the exhibit halls to determine whether the organization has a monetary relationship with the unproven medication manufacturers through their purchases of exhibitor space. There often appears to be little attempt to restrict advertisers and sponsors to those whose products conform to evidence-based medicine. For instance, attendees at the 2005 APhA Annual Meeting and Exposition were able to visit exhibitor booths offering a product made from fermented soy and pine bark extract that promised to provide benefit for deep vein thrombosis; a “probiotic” promising efficacy in pediatric gastrointestinal disorders (mixed with baby food); a supplement claiming to be clinically proven to benefit mood, joints, and liver; homeopathic products and zinc lozenges promoted for the common cold; and dozens of similar herbs and dietary supplements whose claims were not evidence-based but were nevertheless promoted for treatment of a variety of serious medical conditions.82–87 APhA does not require prominent posting of the legal disclaimer required on labels of dietary supplements in the booths of those exhibitors selling unproven medications, and does not include such a disclaimer in the “Exposition Highlights” section of the Final Program. By not doing so, APhA appears to endorse each exhibitor's products, whether or not they are proven safe and effective.
As another example, the 2005 National Community Pharmacists Association Annual Convention and Trade Expo Exhibitor Prospectus explained that the cost of a booth could be as high as $90,200, making it a valuable revenue source for the organization.88 A list of prior exhibitors demonstrated the purchase of booth space by companies selling non—evidence-based products such as homeopathics, herbals, and dietary supplements.88
Justification 4: The Federal Trade Commission (FTC) Prevents Deceptive Advertisements
This is a common misconception among professionals and the lay public. Further, those who publish pharmacy magazines and journals may justify including advertisements for unproven products with the excuse that the FTC polices the advertisements prior to their placement in the magazine. The self-stated mission of the Bureau of Consumer Protection of the FTC is to protect consumers against unfair, deceptive, or fraudulent advertising practices.89 However, while the agency has engaged in many laudable activities, it is overwhelmed by the task remaining before it. The Deputy Director testified before the House in 2006 regarding dietary supplements. The FTC had only filed a few dozen complaints (see testimony in the separate sidebar) in only the most egregious cases. Clearly, in light of the hundreds of thousands of cases of unfair, deceptive, and fraudulent advertising practices that can be found in the media and readily accessed in Internet searches, the FTC poses only a minor threat to the manufacturer of unproven products and provides little defense for the consumer. Further, the FTC appears to react only after the unfair, deceptive, and fraudulent advertising practices have occurred. Filing an online complaint on the FTC's website leads to a form reply and a form letter. Thus, the pharmacist who justifies selling unproven products by trusting the regulatory role of the FTC in ensuring that all advertisements for them are truthful is profoundly mistaken.
OTHER PROFESSIONS
While space limitations preclude a thorough examination of the use, endorsement, and/or acceptance of unproven therapies in other health care professions, a few examples are described to demonstrate that pharmacy's departure from evidence-based medicine is not unique. Within nursing, an unproven method known as “therapeutic touch” is gaining momentum and being studied by nurses as a valid medical intervention.90 It involves passing the nurse's hands around the body (but not touching the body) in an attempt to manipulate an “energy field” or “aura” until the body returns to health. Of course, the existence of an energy field or aura is completely unknown to legitimate medicine; its widespread acceptance by nursing in the current climate of evidence-based medicine is puzzling at best.
While some health care professionals regard the entire body of chiropractic as unproven and dangerous, a subgroup of chiropractors also resort to several non–evidence-based potentially dangerous treatments.91–94 One is known as “craniosacral therapy,” in which practitioners assert that they can alter the skull's bones with pressures as subtle as the weight of a nickel.95 The fact that the adult's bones are fused does not alter their assertions. Another non—evidence-based chiropractic treatment is “neurocranial restructuring” (also practiced by “naturopaths”), which may be dangerous to patients.91,93,96 Chiropractors often resort to an unproven diagnostic technique known as “applied kinesiology” or “muscle testing.”97–99 Practitioners believe that dysfunctions of the organs, nutrient deficiencies, and allergies are manifested by specific corresponding weaknesses in the muscles, and that in-office muscle testing can uncover the organ disorder. While chiropractors use several unproven methods to carry out applied kinesiology, a common one is to ask the patient to stand with the left arm outstretched at a 90° angle. The healer then pushes the patient's arm down as the patient attempts to resist the pressure. To begin a test for allergies, the patient places a suspected allergen in the mouth or holds it in the right hand. If the healer can now press the left arm down with less force, it is allegedly due to the skin or oral contact with the suspected allergen. One web site suggests that the healer simply read a list of suspected substances, implying that hearing the name of an allergen will make the muscles weak.100 Practitioners also suggest that one can uncover the allergies in a pet through surrogate testing.”101,102 The owner holds the pet to be tested. The weakness of the pet would purportedly be manifested in the person holding it on behalf of the pet. Each of these unproven practices discredit their practitioners within legitimate medicine. They are based on spurious and fallacious physiology and anatomy.
Physicians may also turn to unproven medications and therapies in an attempt to boost lagging incomes or for other reasons, and some have become quite successful at promoting unproven therapies. For instance, a Virginia orthopedic surgeon fraudulently sold an intravenous product containing aloe vera to treat AIDS and cancer, netting as much as $18,000 for each 2-week treatment before he was convicted and began serving a prison term.103
EVIDENCE-BASED EDUCATION
Like other professions, pharmacy is under tremendous external and internal pressure to accept and recommend products lacking proof of safety and efficacy, and not grounded in evidence-based medicine. Pharmacy colleges should include a required course in unproven medications and therapies. It should address the benefits of an evidence-based approach to medicine in general and to pharmaceutical care in particular. It should discuss the ethical dilemma inherent in recommending products lacking proof of safety and efficacy. When unproven systems are taught (eg, homeopathy), they must be clearly labeled as such and their departures from evidence-based medicine clarified for students.104 When specific unproven medications are taught, unproven uses should be identified as lacking supporting data. Dosages should not be required unless there is evidence-based confirmation by the FDA that such doses are safe and effective. Doses found on the Internet or supplied by manufacturers fail this standard. Full coverage of drug interactions and adverse reactions should be provided.
A MODEL CURRICULUM
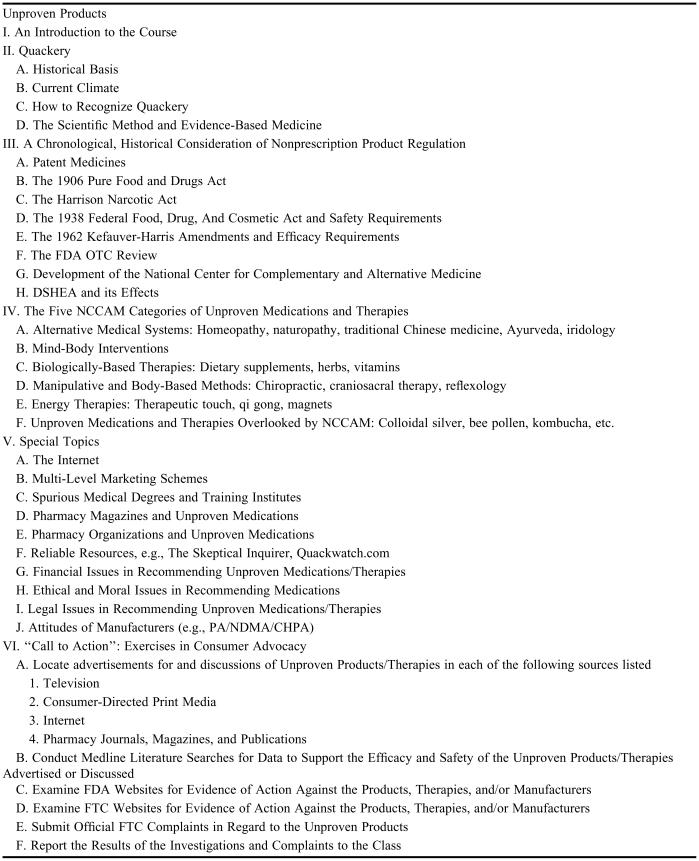
Developing a model curriculum for unproven medications and therapies presents certain fundamental questions. Should practitioners of unproven therapies be invited speakers? The author suggests that any invited speaker's lecture be preceded by a professorial presentation and class discussion of any misconceptions or pseudoscientific beliefs likely to be discussed, so students will be able to understand the nature of the fallacy and to ask specific questions about the core premise on which the therapy is based. Students should also be encouraged to ask penetrating questions designed to force the invited speaker to explain the unproven therapy in the face of evidence-based medicine. The topics included would be subject to time constraints, but could include any or all of those listed in Table 1.
Table 1.
Suggested Topics for Inclusion in a Pharmacy Course on Unproven Medications and Therapies
No single textbook will include all of the topics listed in the suggested curriculum. However, several have useful discussions. A History of Nonprescription Product Regulation includes the chronological history of nonprescription product regulation, serving as a useful background for the current climate. Nonprescription Product Therapeutics includes chapters on herbal supplements, homeopathy, and various other unproven medications and therapies, as well as a discussion of DSHEA. The course coordinator could also consider Natural Products: A Case-Based Approach for Health Care Professionals and Consumer's Guide to Dietary Supplements and Alternative Medicines: Servings of Hope. Undoubtedly, various Internet web sites would be invaluable, including web sites of NCCAM, FDA, FTC, and other regulatory bodies, and also web sites sponsored by those selling unproven products and therapies.
CONCLUSION
The principles of evidence-based medicine have not taken full hold in the realm of nonprescription products and devices. With national organizations and national pharmacy publications failing to fully address the deficiencies inherent in unproven medications and therapies, colleges of pharmacy should offer students a full grounding in the precepts of evidence-based medicine as it relates to unproven medications and therapies. ACPE suggests curricular inclusion of unproven medications and therapies but does not prescribe how it should be taught. It is incumbent upon pharmacy colleges to adhere to the principles of evidence-based medicine, critically examining unproven medications and therapies (eg, homeopathy, herbals, or dietary supplements) in the light of its guiding principles.
DISCLOSURE
Two of the texts referenced in this article12,97 were written by Steven Pray, author of this paper: A History of Nonprescription Product Regulation and Nonprescription Product Therapeutics.
Appendix 1. FTC's Testimony in 2006 Regarding Dietary Supplements105
For Release: March 9, 2006
FTC Testifies on Dietary Supplements
In testimony today before the House Committee on Government Reform, Lee Peeler, Deputy Director of the FTC's Bureau of Consumer Protection, said, “Although many supplements offer the potential for real health benefits to consumers, unproven products and inaccurate information can pose a threat to the health and well-being of consumers and cause economic injury.”
“The Commission has focused its enforcement priorities on national advertising claims for products with unproven benefits; products promoted to treat or cure serious diseases; products that may present significant safety concerns to consumers; and products that are deceptively marketed to or for children and adolescents,” the testimony stated. The FTC has filed fourteen complaints in the past year against companies making allegedly unsubstantiated or false advertising claims for dietary supplements and other natural healthcare products, including oral sprays, creams, and patches. Also, in the past year, the Commission obtained orders against forty companies and forty-four individuals, which prohibited the unlawful practices and required the defendants to pay a total of $35.5 million in consumer redress, disgorgement, and civil penalties.
The testimony noted that, “Products are promoted to adults not just to maintain basic health and nutrition, but also for weight loss, to build muscle, cure sexual dysfunction, treat and prevent colds and flu, and even reverse arthritis, cure cancer, and treat many other serious diseases. Products promoted specifically for children also extend beyond traditional multivitamins to include treatment and cures for a variety of childhood ailments ranging from colds to more serious conditions such as attention deficit/hyperactivity disorder (AD/HD).”
The testimony highlighted recent examples of FTC cases, consumer education efforts, and partner cooperation that illustrated the Commission's multi-faceted approach. In particular, the testimony discussed the FTC's priority on youth-targeted products, “not only because young consumers represent a particularly vulnerable audience, but also because the safety concerns are heightened when children, who are still growing and developing, use products that may have been studied for safety only in adults, if at all.”
The Commission approved the testimony by a vote of 5-0.
NOTE: The views expressed in the written testimony represent those of the Federal Trade Commission. Oral testimony and responses to questions do not necessarily reflect the views of the Commission or any individual Commissioner.
REFERENCES
- 1. Anon. Orrin G. Hatch (R-UT) Top Contributors. Available at: http://www.opensecrets.org/politicians/contrib.asp?CID=N00009869&cycle=2002. Accessed November 10, 2006.
- 2.Mehlman MJ. Quackery. Am J Law Med. 2005;31:349–63. doi: 10.1177/009885880503100209. [DOI] [PubMed] [Google Scholar]
- 3.Griffenhagen GB. Toadstools and mushrooms (editorial) J Am Pharm Assoc. 1963;NS3:457. [Google Scholar]
- 4.Milstead KL. Enforcement of antiquackery laws. J Am Pharm Assoc. 1963;NS3:458–60. [Google Scholar]
- 5.Quackery…The billion dollar miracle business. Rockville, MD: Food and Drug Administration; 1990. [Google Scholar]
- 6.Young JH. The development of the Office of Alternative Medicine in the National Institutes of Health. Bull Hist Med. 1998;72:279–98. doi: 10.1353/bhm.1998.0110. [DOI] [PubMed] [Google Scholar]
- 7. The NIH Almanac-Organization, National Center for Complementary and Alternative Medicine. Available at: http://www.nih.gov/about/almanac/organization/NCCAM.htm. Accessed July 10, 2006.
- 8. About the National Center for Complementary and Alternative Medicine, The National Center for Complementary and Alternative Medicine. Available at: http://nccam.nih.gov/about/aboutnccam/index.htm. Accessed July 10, 2006.
- 9. Gorski TN. Current issues in protecting the public from health fraud: “Dietary supplements” as a public health problem. Testimony before the U.S. Senate Special Committee on Aging, 2001, Quackwatch. Available at: http://quackwatch.org/01QuackeryRelatedTopics/Hearing/gorski.html. Accessed July 10, 2006.
- 10. Atwood KC IV. The ongoing problem with the National Center for Complementary and Alternative Medicine, Committee for the Scientific Investigation of Claims of the Paranormal. Available at: http://www.csicop.org/si/2003-09/alternative-medicine.html. Accessed July 10, 2006.
- 11. Sampson WI. Why the National Center for Complementary and Alternative Medicine should be defunded, Quackwatch. Available at: http://www.quackwatch.org/01QuackeryRelatedTopics/nccam.html. Accessed July 10, 2006.
- 12.Pray WS. A History of Dietary Supplement Regulation. A History of Nonprescription Product Regulation. In: Pray WS, editor. New York NY: Pharmaceutical Products Press; 2003. pp. 205–38. [Google Scholar]
- 13.Mechanick JI. The rational use of dietary supplements and nutraceuticals in clinical medicine. Mt Sinai J Med. 2005;72:161–5. [PubMed] [Google Scholar]
- 14.Perls TT. Anti-aging quackery: Human growth hormone and tricks of the trade–More dangerous than ever. J Gerontol. 2004;59:682–91. doi: 10.1093/gerona/59.7.b682. [DOI] [PubMed] [Google Scholar]
- 15. Focus ADHD Formula, NativeRemedies.com. Available at: http://www.nativeremedies.com/focus_for_adhd.shtml. Accessed July 10, 2006.
- 16. Autism, NativeRemedies.com. Available at: http://www.nativeremedies.com/autism-aspergers-rett-pdd.shtml. Accessed July 10, 2006.
- 17. Fertile XX and Fertile XY, NativeRemedies.com. Available at: http://www.nativeremedies.com/fertile-xx-xy-male-female-fertility.shtml. Accessed July 10, 2006.
- 18. Detox Drops, NativeRemedies.com. Available at: http://www.nativeremedies.com/detox_drops_cleansing_and_weight_loss.shtml. Accessed July 10, 2006.
- 19.Study shows St. John's wort ineffective for major depression. FDA Consumer. 2002;36(3):8. [PubMed] [Google Scholar]
- 20.Kava and severe liver injury. FDA Consumer. 2002;36(3):4. [PubMed] [Google Scholar]
- 21. About CHPA, Consumer Healthcare Products Association. Available at: http://www.chpa-info.org/ChpaPortal/AboutCHPA/. Accessed July 10, 2006.
- 22.Levy S. NDMA will answer to CHPA and to a growing product list. Drug Topics. 1999;143:39. [Google Scholar]
- 23.Buerki RA, Vottero LD. Madison, WI: American Institute of the History of Pharmacy; Ethical Responsibility in Pharmacy Practice; pp. 146–62. [Google Scholar]
- 24. Code of ethics for pharmacists, American Pharmacists Association. Available at: http://www.aphanet.org/AM/Template.cfm?Section=Home&CONTENTID=2654&TEMPLATE=/CM/HTMLDisplay.cfm. Accessed July 10, 2006.
- 25. Improving medication use. Advancing patient care, American Pharmacists Association. Available at: http://www.aphanet.org/AM/Template.cfm?Section=About_APhA&CONTENTID=2410&TEMPLATE=/CM/HTMLDisplay.cfm. Accessed July 10, 2006.
- 26.Final Program. Washington DC: American Pharmaceutical Association; 1995. American Pharmaceutical Association 142nd Annual Meeting & Exposition; p. 53. [Google Scholar]
- 27.Feldman EG. Harmless, but ineffective, remedies (editorial) J Pharm Sci. 1975;64:1584I. [PubMed] [Google Scholar]
- 28.Foreman D. Lifesaving bacteria. Pharm Today. 2005;11:6. [Google Scholar]
- 29.Product showcase. Pharm Today. 2005;11:6. [Google Scholar]
- 30. Hyland's Complete Flu Care 4 Kids, MyHealthCare21.com. Available at: http://www.myhealthcare21.com/HY152/Complete-Flu-Care.html. Accessed July 10, 2006.
- 31.Guthrie EW. Lessons learned from early Americans. Pharm Today. 2005;11:6. [Google Scholar]
- 32.Foreman D. The ancient beverage that heals. Pharm Today. 2005;11:12;31. [Google Scholar]
- 33.Slezak M. Practicing on pins and needles. Am Druggist. 1996;213:26;28–30. [Google Scholar]
- 34.Slezak M. Rite Aid advertises its vitamin expertise. Am Druggist. 1997;214:13. [Google Scholar]
- 35.Batz F. Integrating herbal therapy into practice. Am Druggist. 1998;215:5858–65. [Google Scholar]
- 36.Tyler VE. Why many ‘health foods’ are not safe and effective. Pharm Times. 1983;49:35–7. [Google Scholar]
- 37.Grauds C, Cox J. Introduction to Aromatherapy. Pharm Times. 1999;65:80. [Google Scholar]
- 38.Grauds C. Selenium reduces incidence of prostate cancer. Pharm Times. 1999;65:83. [Google Scholar]
- 39.Grauds C. Milk thistle: A potential life-saver. Pharm Times. 1996;62:95. [Google Scholar]
- 40.Grauds C. Treating migraine and arthritis with feverfew. Pharm Times. 1995;61:32;34. [Google Scholar]
- 41.Sherman M. Natural medicines: A rare opportunity for pharmacists. Pharm Times. 1997;63:80;82. [Google Scholar]
- 42.McCormick E. Modern and traditional medicines: Can they coexist? Pharm Times. 1998;64:71–2. [Google Scholar]
- 43. RONH10@JUNO.com. Concern over herbals (Letter). Pharm Times. 1997;63(12):8.
- 44.Pacy DJ. “Unleashed herbal explosion” (Letter) Pharm Times. 1999;65:12. [Google Scholar]
- 45.Terrie YC. Antisnoring products. Pharm Times. 2005;71:11;15–6. [Google Scholar]
- 46.OTC product news. Alphactif for Men. Pharm Times. 2005;71:18. [Google Scholar]
- 47.Garrett AD. Complementary medicine and diabetes: What's fact, what's fiction? Pharm Times. 2005;71:34. [Google Scholar]
- 48.Appearex (Advertisement) Pharm Times. 2005;71:35. [Google Scholar]
- 49.Pray WS. Quackery, a deadly threat to health. US Pharm. 1991;16:35–6. 39–40. [Google Scholar]
- 50.Kwong-Robbins C. Traditional Chinese medicine–a natural and holistic approach. US Pharm. 2002;27(12):44;46;48–50. [Google Scholar]
- 51.Kwong-Robbins C. The art and science of Chinese herbal medicine. US Pharm. 2003;28(3):62;65;68;71;75. [Google Scholar]
- 52. Drug Store News, Drug Store News. Available at: http://www.drugstorenews.com/. Accessed January 6, 2006.
- 53.Lavalle JB. Treating women's health the natural way. Drug Store News. 1998;8:CP31. [Google Scholar]
- 54.Eder R. OTC giants join herbal game. Drug Store News. 1997;7:27. [Google Scholar]
- 55.Nature's Essence Blood Tonic Syrup (Advertisement) Drug Store News. 1998;8:CP14. [Google Scholar]
- 56.Snyder K. R.Ph.s can learn more about CAM. Drug Topics. 1996;140:52. [Google Scholar]
- 57.Bennett J. The best pharmacy practices: Innovative or diverse services. Drug Topics. 1997;141:96–105. [Google Scholar]
- 58.Snyder K. Cold-Eeze lozenges are taking the nation by storm. Drug Topics. 1997;141:16;19. [Google Scholar]
- 59.Davis WM. The role of glucosamine and chondroitin sulfate in the management of arthritis. Drug Topics (supplement). 1998;142(8):1S–15S. [Google Scholar]
- 60.Portyansky E. Alternative medicine-how bountiful is the harvest? Drug Topics. 1998;142:44–45;47;49–50. [Google Scholar]
- 61.Tarlach GM. Turning herbs ‘N2’ profits. Drug Topics. 1998;142(2):66. [Google Scholar]
- 62.Levy S. M.D.s issue call for testing alternative medications. Drug Topics. 1998;142:21. [Google Scholar]
- 63.Angell M, Kassirer JP. Alternative medicine-The risks of untested and unregulated remedies (editorial) N Engl J Med. 1998;339:839–41. doi: 10.1056/NEJM199809173391210. [DOI] [PubMed] [Google Scholar]
- 64.Fleming H., Jr A natural progression. Drug Topics. 1998;142:74. [Google Scholar]
- 65.Levy S. Reading, writing…and complementary care. Drug Topics. 1999;143:42;44. [Google Scholar]
- 66.Levy S. Don't miss this boat. Drug Topics. 1999;143:41–2;44;49. [Google Scholar]
- 67.Levy S. R.Ph. finds consumers becoming complementary care friendly. Drug Topics. 1999;143:61. [Google Scholar]
- 68.Fleming H., Jr Two in one. Drug Topics. 1999;143:15. [Google Scholar]
- 69.Williamson JS, Wyandt CM. New perspectives on alternative medicine. Drug Topics. 2001;145:57–66. [Google Scholar]
- 70.Kratz AM. Flawed article (letter) Drug Topics. 2001;145(5):18. [Google Scholar]
- 71. Allen Kratz, Premiere Speakers Bureau. Available at: http://premierespeakers.com/1066/index.cfm. Accessed July 10, 2006.
- 72.Kwong-Robbins C. Setting record straight on herbs (Letter) Drug Topics. 2001;145:12;15. [Google Scholar]
- 73.New product bulletin, Alpha CF (Advertisement) NARD Journal. 1989;111:12. [Google Scholar]
- 74.Herbals' increasing popularity raises regulatory concerns. NABP Newsletter. 1999;28:156–7. [Google Scholar]
- 75.NAPLEX pool to include items on dietary supplements. NABP Newsletter. 2002;31:143. [Google Scholar]
- 76.NAPLEX to test herbal knowledge. AACP News. 2003;34(1):4. [Google Scholar]
- 77. ACPE, Accreditation Council for Pharmacy Education. Available at: http://www.acpe-accr%20edit.org/about/default.asp. Accessed July 10, 2006.
- 78. Accreditation standards and guidelines for the professional program in pharmacy leading to the Doctor of Pharmacy degree, Accreditation Council for Pharmacy Education. Available at: http://www.acpe-accredit.org/deans/standards.asp. Accessed July 10, 2006.
- 79.Rowell DM, Kroll DJ. Complementary and alternative medicine education in United States pharmacy schools. Am J Pharm Educ. 1998;62:412–9. [Google Scholar]
- 80.Bailey R. Eric Alvarez believes in customer service. Community Pharm. 1999;91:20–2. [Google Scholar]
- 81.Levy S. Independent luminaries of 2002. Drug Topics. 2002;146:25–6;29. [Google Scholar]
- 82.Final Program. Washington DC: American Pharmaceutical Association; 2005. APhA2005 Annual Meeting & Exposition; pp. 44–61. [Google Scholar]
- 83. Aidan Products. Available at: http://www.aidanproducts.com/cart.php?m=product_list&c=1&product=3. Accessed July 10, 2006.
- 84. Flite Tabs, Aidan Products. Available at: http://www.aidanproducts.com/cart.php?m=product_detail&p=11. Accessed July 10, 2006.
- 85. Culturelle Information, ConAgra Functional Foods, Inc. Available at: http://www.culturelle.com/culturelle_info.jsp. Accessed July 10, 2006.
- 86. MoodPlus Sam-e. Available at: http://www.naturemade.com/productdatabase/prd_prod.asp?productid=71. Accessed July 10, 2006.
- 87. Herbal supplements, Naturemade. Available at: http://www.naturemade.com/ProductDatabase/prd_srch_rslt.asp?categoryid=269. Accessed July 10, 2006.
- 88. Exhibitor prospectus, National Community Pharmacists Association. Available at: http://www.ncpanet.org/pdf/2005exhibitorprospectus_web.pdf. Accessed July 10, 2006.
- 89. Guide to the Federal Trade Commission. Available at: http://www.ftc.gov/bcp/conline/pubs/general/guidetoftc.htm. Accessed July 10, 2006.
- 90. Barrett S. Therapeutic touch, Quackwatch. Available at: http://www.quackwatch.org/01QuackeryRelatedTopics/tt.html. Accessed July 10, 2006.
- 91.Atwood KC. “Neurocranial restructuring” and homeopathy, neither complementary nor alternative. Arch Otolaryngol Head Neck Surg. 2003;129:1356–7. doi: 10.1001/archotol.129.12.1356. [DOI] [PubMed] [Google Scholar]
- 92.Schakowsky LA. Experiences in challenging chiropractic. Conn Med. 2003;67:249–50. [PubMed] [Google Scholar]
- 93. Boyer B, Cole ND. NCR-A powerful therapy. Available at: http://www.drboyercole.com/ncr.html. Accessed July 10, 2006.
- 94. Barrett S. Chiropractic's dirty secret: Neck manipulation and strokes. Available at: http://www.quackwatch.org/01QuackeryRelatedTopics/chirostroke.html. Accessed July 10, 2006.
- 95. Barrett S. Craniosacral therapy, Quackwatch. Available at: http://www.quackwatch.org/01QuackeryRelatedTopics/cranial.html. Accessed January 9, 2006.
- 96. Barrett S. Be wary of NeuroCranial restructuring (NCR). Available at http://www.chirobase.org/06DD/ncr.html. Accessed July 10, 2006.
- 97.Pray WS. Precautions in self-care. In: Pray WS, editor. Nonprescription Product Therapeutics, 2nd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2005. pp. 809–10. [Google Scholar]
- 98.Lowes R. A field guide to alternative healers. Your patients see them as well as you, so know who's out there. Med Econ. 2004;81:21–4. [PubMed] [Google Scholar]
- 99. Barrett S. Applied kinesiology: Muscle-testing for “allergies” and “nutrient deficiencies.” Available at: http://www.chirobase.org/06DD/ak.html. Accessed July 10, 2006.
- 100. Muscle testing. Available at http://www.worldtrans.org/TP/TP2/TP2A-67.HTML. Accessed July 10, 2006.
- 101. Touch therapies/Visualization. Available at http://www.alternativepethealth.com/applied-kinesiology.html. Accessed July 10, 2006.
- 102. Veterinary NAET. Available at: http://www.vetnaet.com/article2.html. Accessed July 10, 2006.
- 103.Meadows M. Maryland man, Virginia physician sentenced for illegally marketing aloe vera “treatments.”. FDA Consumer. 2002;36:34–5. [PubMed] [Google Scholar]
- 104.Shang A, Huwiler-Müntener K, Nartey L, et al. Are the clinical effects of homeopathy placebo effects? Comparative study of placebo-controlled trials of homeopathy and allopathy. Lancet. 2005;366:726–32. doi: 10.1016/S0140-6736(05)67177-2. [DOI] [PubMed] [Google Scholar]