Abstract
Teachers of pharmacy self-care courses have met annually since 1998 at the Nonprescription Medicines Academy (NMA) held in Cincinnati, Ohio. During these meetings, self-care faculty members discuss methods of enhancing the teaching of self-care in US colleges and schools of pharmacy. Self-care courses are taught using a variety of methods and content is woven into pharmacy curricula in many different ways. This manuscript sets forth the current state of self-care instruction in pharmacy curricula including the recommended core curriculum, instructional methodologies, course mechanics, existing standards, and assessment and curricular placement, and makes recommendations for the future.
Keywords: nonprescription medicines, curriculum, self-care, instruction
INTRODUCTION
In 1998, under the leadership of Dr. Dennis B. Worthen and a grant from Procter and Gamble, Inc, 22 instructors of nonprescription medicines and devices (self-care) met in Cincinnati, Ohio, for the first Nonprescription Medicines Academy (NMA). Through his experience, Dr. Worthen had recognized that there was no forum for teachers of self-care and an absence of self-care as a special interest group within existing pharmacy organizations. There was no body of self-care teachers to view or review self-care research, share new teaching methodologies and products, sharpen self-care andragogy (the art and science of helping adults learn), exchange resources, and establish a professional network for continual growth, development, and scholarship.
Over the succeeding 8 years, with Procter and Gamble's ongoing support, over 200 faculty members, representing many of the nation's colleges and schools of pharmacy, have joined the NMA. Annually, the NMA Conference has been organized to promote excellence in teaching self-care and mentoring and networking among faculty members, discuss issues in self-care, and exhibit and exchange methodologies for teaching pharmacy students about nonprescription medicines and devices. The NMA also maintains a web site (http://www.nmafaculty.org/) that provides ongoing support and tools for self-care faculty members to use throughout the year. Through the conference and its web site, educators in self-care have found a voice and a mechanism to discuss ways to enhance self-care instruction within colleges and schools of pharmacy. Self-care instruction is conveyed in a myriad of methods embedded in curricula through various techniques. There are unique challenges for this instruction as well as significant congruence with prescription therapeutics instruction in pharmacy curricula. The NMA recognizes that the pharmacist's role in self-care and wellness is critical and that the National Association of Boards of Pharmacy (NABP) has increased content in this area on its pharmacist licensure examination. In addition, self-care faculty members found it valuable to obtain guidance from one another with regard to curricular time commitment, credit hours allocated, inclusion in core curricula, and dedicated instructional personnel, among others. The NMA believes it is essential for self-care instructors to serve as advocates of self-care instruction in colleges and schools of pharmacy.
The shared vision within NMA was to support a broad structure of nonprescription medication education; to provide examples of a minimum standard for quality and quantity of educational experiences in nonprescription medication education; and to describe methods for successful teaching of nonprescription therapy. This consensus originates out of a need for increased education as directed by changes in the marketplace, the North American Pharmacist Licensure Examination (NAPLEX), the Center for the Advancement of Pharmaceutical Education (CAPE) outcomes, and the Accreditation Council for Pharmacy Education (ACPE) Accreditation Guidelines.
Currently, self-care medicines and devices are primary or adjunctive therapy for over 500 medical conditions. The market for these drugs and devices (including dietary supplements) was approximately $34 billion in 2000.1 Historically, Congress divided those medications believed to be safe for self-selection from those requiring a prescription and oversight by learned intermediaries in 1951 through the Durham-Humphrey Amendment to the FD&C Act of 1938. Although there were comparatively few classes of prescription drugs in the 1960s, an explosion of new scientific discoveries in ensuing years led pharmacy education to transition away from extensive compounding of products and towards helping the patient/consumer in selection of nonprescription medicines in the era of “Clinical Pharmacy” during the 1970s and 1980s. Historically, clinical pharmacy had its roots in institutional practice where new therapeutic discoveries, pharmacokinetics, clinical clerkships, and emerging roles for pharmacists had immediate application. While the clinical pharmacy era was exciting for students and pharmacists, the majority of patients did not benefit from this initial shift in knowledge because few patients spent lengthy hospital stays annually in comparison to the population as a whole. In addition, the marketplace has observed an explosion of products and devices (including dietary supplements and former prescription medications switched to nonprescription status).
Patients selecting nonprescription products potentially have no intermediary clinician guiding them through the selection and appropriate use of those products. Variables impacting appropriate self-care use involve health literacy and literature interpretation of product labeling. In 2003, the National Council on Patient Information and Education (NCPIE) conducted a survey to determine consumer's use and attitudes regarding self-care products. They determined that 8% of consumers read nothing on the label prior to purchase. Over half (54%) failed to read the label to discover the active ingredient, 80% did not read the label to discover possible side effects, and 77% failed to read the label for dosage information.2 Patients need to be encouraged to ask the pharmacist when they have questions about nonprescription medications and pharmacists need to be more accessible to these patients. These data suggests that an increased risk of harm to the patient may exist because patients do not read the product label or seek the advice of a learned intermediary.
Academic pharmacy is renewing its interest in educating students regarding self-care products. Historically, the discipline of “self-care” has not been supported with special interest groups within pharmacy organizations. In addition, the variety of faculty disciplines assigned for course instruction, limited presence in the curriculum, and the lack of job postings specifically calling for self-care faculty positions indicate that more attention should be paid to self-care in pharmacy education. All too often, the self-care curriculum has been a faculty member's collateral duty. With the number of self-care products purchased annually increasing at a steady rate, the increasing number of drug changes from prescription to nonprescription status, the degree of potential drug or disease interactions, and lack of safety and efficacy data on dietary supplements, pharmacists need increasing knowledge and skills to help guide/advise their patients.
For example, an emerging pertinent curricular deficiency lies within dietary supplements (herbals and nutritional supplements). These products have become a new category of unproven “drugs” through the passage of the Dietary Supplement Health and Education Act (DSHEA). As a result, these products bypass the physician/pharmacist/patient triad when purchased directly by the consumer. These products are not vetted by the FDA for safety and efficacy, although they are marketed with various health-related claims. This, also, is one of the most rapidly evolving therapy areas. For example, in 1999, St. John's wort ranked second on a list of most frequently purchased dietary supplements. By 2002, it had dropped to sixth due to increased knowledge of drug or disease interactions (eg, 34 drugs or classes of drugs are currently listed). Other dietary supplements have similar paths of perceived efficacy and anecdotal evidence.3 In certain circumstances, dietary supplements can represent a dangerous therapeutic “wild card” where pharmacists are the most proximal learned intermediaries.
Self-care is a direct application of pharmaceutical care or pharmacist-assisted self-care. Academic pharmacy must stay abreast of this area by educating competent pharmacists who can help patients determine the risk/benefit ratio of using these products. Integrating self-care products into therapeutics courses or using cases in a practice laboratory without a standalone self-care course is insufficient to prepare students for the demands of relevant practical knowledge that patients require. For these reasons the teachers of self-care, meeting over the past 8 years, have decided to collectively voice our recommendations that instruction on self-care should assume a paramount importance in the education of pharmacy students.
Writing for the NMA, the authors of this paper model the current state of self-care instruction in colleges and schools of pharmacy across the nation. Self-care instruction should be given status befitting its prevalence and importance in health care and the same principles and intensity of andragogy should be applied to self-care therapeutics as exist in other instructional areas in the nation's pharmacy programs. To that end, this manuscript addresses the following issues in self-care instruction: core curriculum, instructional methodologies, course mechanics, existing standards, assessment, curriculum placement, and quantity of instruction.
CURRENT STANDARDS AND RESOURCES FOR SELF-CARE CURRICULUM DESIGN
This section provides an overview of standards and resources for curriculum design, including outcomes, content, and process related to teaching and learning in self-care pharmacy practice, nonprescription medicines, and health promotion and wellness practices.
In 1992, the American Association of Colleges of Pharmacy (AACP) initiated a series of initiatives under the CAPE. These initiatives were designed to support and facilitate the efforts of US colleges and schools of pharmacy to transform their curricula to enhance the education of future practitioners’ delivery of pharmaceutical care. Significant to the design of new curricula were the CAPE Educational Outcomes, which were intended to be the target toward which the evolving pharmacy curriculum should be aimed. The CAPE Advisory Panel on Educational Outcomes was reconvened for that purpose and a revised document was made available in 1998.
At the urging of the 2001-2002 AACP Academic Affairs and Professional Affairs Committees, the AACP Board of Directors committed to a review and revision of the CAPE Educational Outcomes during 2003-2004. This revision process was timely given the anticipated revision of the Accreditation Council for Pharmacy Education (ACPE) Accreditation Standards and Guidelines for the Professional Degree Program in Pharmacy Leading to the doctor of pharmacy degree. Periodic review and revision of the Educational Outcomes document is necessary to assure the contemporary validity of the educational content and outcomes with emerging sciences and scientific developments and evolving roles of the pharmacist in serving patient and public health needs. Another revised version of the CAPE Educational Outcomes was completed and distributed in 2004. The 2004 version provides a new organizing framework that integrates science, professional attributes, interprofessional practice, and professionalism across new major headings of pharmaceutical care, systems management, and public health.
The 2004 CAPE Educational Outcomes provide guidance for the organization of student outcomes in the areas of self-care, nonprescription medications, and health promotion and wellness. A list of these outcomes can be found on the AACP website (http://www.aacp.org/Docs/MainNavigation/Resources/6075_CAPE2004.pdf).
North American Pharmacist Licensure Examination
The NAPLEX is the examination taken by all United States pharmacy graduates prior to licensure. It is meant to ensure that the candidate possesses minimal competency to practice pharmacy. The creators of NAPLEX consider nonprescription product and device training an essential element of pharmaceutical competency. According to the examination's competency statements, the test requires the candidate to perform the following tasks directly or indirectly related to pharmacist-assisted self-care (among others) 4:
Competency 1.1.0: Obtain, interpret and evaluate patient information to determine the presence of a disease or medical condition, assess the need for treatment and/or referral…
Competency 3.2.0: Educate the public and health-care professionals regarding medical conditions, wellness, dietary supplements, and medical devices.
Competency 3.2.4: Provide information regarding the selection, use and care of medical/surgical appliances and devices, self-care products, and durable medical equipment, as well as products and techniques for self-monitoring of health status and medical conditions.
In its latest revision of the NAPLEX blueprint, implemented in 2005, the National Association of Boards of Pharmacy (NABP) announced a pioneering amendment in regard to nonprescription products: the organization will ensure that the examination will “treat over-the-counter and prescription products equally.”4 Taken literally, this statement appears to indicate that for every question involving a prescription product, the blueprint will retain balance by presenting the candidate with a question involving a nonprescription product. This appears to be the first time that any accrediting body or standard-setting agency has recognized that knowledge of nonprescription products is as important to the nascent pharmacist's future as prescription products. Another manuscript in this series authored by Matt Lee, PharmD, National Association of Boards of Pharmacy, provides an explanation of the reasons behind increasing the value of nonprescription medicines and self-care onto the licensure examination with equal weight when compared to prescription medicines.
Accreditation Standards and Guidelines
Pharmacy degree programs in the United States are accredited by ACPE using a set of standards and guidelines. In February 2006, ACPE issued new standards and guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. These standards will become effective on July 1, 2007. In that document, Standard 12, Professional Competencies and Outcome Expectations, includes language adapted from the CAPE Educational Outcomes 2004 as described above. Specific guidance related to nonprescription medications and self-care is included in Appendix C, related to advanced pharmacy practice experiences. Delineated activities specific to nonprescription medications and self-care include:
identifying, evaluating, and communicating to the patient and other health care professionals the appropriateness of the patient's specific pharmacotherapeutic agents, dosing regimens, dosage forms, routes of administration, and delivery systems;
consulting with patients regarding self-care products;
recommending prescription and nonprescription medications, dietary supplements, diet, nutrition, traditional non-drug therapies, and complementary and alternative therapies;
providing pharmacist-delivered patient care to a diverse patient population; and
providing patient education to a diverse patient population.5
Clearly, educators, regulators, and accreditors consider knowledge of pharmacist-assisted self-care, nonprescription products, and professional triage to be components of core competency for the prospective pharmacist. Documents and resources promulgated by the organizations representing these constituencies provide guidance for curriculum review and the design of teaching and learning activities and assessment strategies in the areas of nonprescription medications, self-care, and health promotion.
THE IMPORTANCE OF SELF-CARE IN THE CORE CURRICULUM
Besides the aforementioned standards and competencies, there are additional justifications for including nonprescription products in the curriculum. The pharmacy curriculum is intended to prepare students to care for patients in a variety of settings. According to the US Department of Labor, approximately 62% of pharmacists work in community pharmacies.6 Another 22% of salaried pharmacists work in hospitals, with the balance being employed in other venues, eg, clinics, mail-order pharmacies, government. The realities of the workplace, therefore, allow one to conclude that a student is almost 3 times more likely to use skills and knowledge specific to community pharmacy. In the community pharmacy, where patients ask for assistance, the pharmacist is the only health care provider present to perform professional triage. Within this role, the pharmacist can help a patient/consumer determine whether to consult a physician, select a nonprescription product, or use a non-drug means to alleviate the problem. Thus, for the typical community pharmacist, self-care is one of the most direct applications of pharmaceutical care. For this reason, instruction on self-care consultations should be expanded and enhanced in the education of pharmacy students.
Another issue that underscores the importance of pharmacist training in nonprescription products is the prescription-to-nonprescription switch movement. Consumers often seek out a newly available product to determine whether it is a better treatment for their condition. The pharmacist has a critical role in assisting patients with selecting and using these potent medications to assure they are used effectively.
An additional compelling reason for enhanced nonprescription product education and skill development for future pharmacists is the need for well-informed patient educators with regard to nonprescription products and devices. Patients often rely on print, television, and Internet advertisements for advice on their condition and on product selection. However, the manufacturer's advertisement is not typically an educational vehicle, but a device to build awareness and demand for their brands, ie, market share. The pharmacist must assess the patient's current understanding and build on this with unbiased information to help the patient decide which product is preferable. With an appropriate education in self-care, the pharmacist can become the primary health professional with specific university-based training in the areas of nonprescription patient education and product selection.
Nonprescription product and device education and skill development and the concept of self-care is vital in the education of future pharmacists in that many future practitioners will continue to work in community pharmacy, the primary venue for advising patients on nonprescription products and devices. Nonprescription products and devices are only judged to be safe by the FDA when the patient reads all labels; however, as stated earlier, many patients do not read labels, making the intervention of a pharmacist potentially lifesaving. Powerful prescription medications are being switched to nonprescription status. The pharmacist is ideally positioned to counsel patients during the post-switch period. A pharmacist can help patients sort through the information dispersed in advertising to help them determine whether the product is the best one for their condition.
SELF-CARE CORE CURRICULUM
A self-care core curriculum can be viewed as a list of several topic areas that are considered of high importance in the nonprescription medicines arena. These topics are key elements about which patients often inquire and, therefore, about which students within pharmacy curricula should be well informed. This list was compiled using multiple references and is meant to serve as a beginning guide for faculty members who teach in the nonprescription arena. The authors recognize that course structure and dynamics are influential when determining content areas to be included and to what degree. This list of topics is in no particular rank-order, so faculty members are encouraged to consider this list and, accordingly, adjust when designing or modifying their nonprescription medicines courses.
The compilation of this list was influenced by several key references. First and foremost was the discussion conducted at the 2003 NMA annual faculty meeting, which represented approximately 40 schools or colleges of pharmacy. Participants shared experiences from their various colleges of pharmacy and generated a list of key topic areas that were believed to be of central importance when mastering knowledge and skills related to nonprescription medications. Additional data were extracted from the 2 primary textbooks used by most colleges of pharmacy as key references for nonprescription medicine courses: The Handbook of Nonprescription Drugs 7 and Nonprescription Product Therapeutics. 8 The topic areas covered within these textbooks were compared to the initial list generated from the NMA 2003 discussion. In addition, further information was added to each content area to give faculty a more detailed description of the information contained within each topic. Additional comparisons were performed with the list of commonly utilized nonprescription medications based on sales along with the common nonprescription medications most widely recommended by pharmacists.9,10
Prior to embarking on the list of specific content areas that could be considered a core curriculum, the NMA faculty group identified certain skills and special issues that could be considered more universal in nature and span the entire nonprescription curriculum. The skills and issues included: the process of self-care (including patient assessment and triage), emerging issues in nonprescription medicines, the incorporation of special population groups, and cultural competence.
Self-care is among the most important topics in/of which students must be knowledgeable. Skills to accurately assess a patient's condition and triage patients appropriately are also necessary. The assessment process includes patient interviewing techniques and symptom-based diagnostic schemata, along with observational physical assessment skills which will provide the student with the ability to make an accurate decision regarding whether the patient is a good candidate for self-care.
The concept of incorporating emerging issues in nonprescription medicines stems from the fact that the nonprescription product market is continually evolving. Because of the changes in switching medications from prescription to nonprescription status, and the rigorous process of reviewing nonprescription products since 1972, the following topics are ideas to consider when discussing emerging nonprescription issues: FDA regulations of nonprescription drugs and devices including the drug approval process, drug reclassifications (ie, prescription to nonprescription switches); the possibility of the establishment of a third class of drugs, “pharmacist-only,” or a “pharmacy-only” category of drugs; and nonprescription medication marketing issues.
Nonprescription medication selection can be complex in the average patient population. In addition, pharmacists field questions from subpopulations with specific circumstances that make recommending a nonprescription product even more difficult. Some of these special population groups include pediatric, geriatric, pregnant, and lactating patients. With these groups, considerations must be made for a number of different factors including altered pharmacokinetics, population-specific drug effects, and medication administration needs. When learning about the core curriculum topics, students must be cognizant of the modifications needed when making therapeutic recommendations to these specific patient populations.
Cultural competence must be incorporated when discussing nonprescription medications and recommendations for patients as it is a core requirement within the professional curriculum. Cultural competence involves challenging one's own cultural assumptions and beliefs, developing empathy for people from other cultures, and applying specific communication and interaction skills in clinical encounters.11 For health professionals, sensitivity to cultural, ethnic, linguistic, and social diversity helps to avert problems and misunderstandings, improves satisfaction for all concerned, and leads to better patient outcomes. Programs need to focus on providing opportunities in the classroom and the clinical arena for students to work within interprofessional teams. Efforts to be “culturally competent,” in the absence of a patient-centered approach, may unintentionally encourage stereotyping, thereby negatively affecting the quality and content of clinical care.12 Therefore, students' understandings of cultural difference, the accuracy of those understandings, and their impact on patient care should be carefully explored. Andragogical initiatives also need to incorporate case-based formats and interactive sessions with actual or simulated patients and families. The principles underlying this approach: openness, mutual respect, inclusiveness, responsiveness, and understanding one's professional roles should be fundamental to the delivery of culturally competent health care to all ethnic communities.13
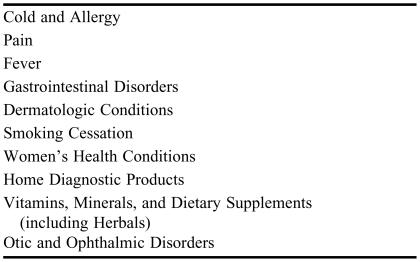
To define a core curriculum, a list of 10 primary topic areas was generated. These topic areas are depicted in Table 2. In addition, they are defined in more detail in the text below. As mentioned previously, these topics can be modified by nonprescription medicines faculty to accommodate the level of students and placement of the course within the curriculum, and to identify overlap with other pharmacy courses. Some examples of other content areas beyond the core 10 listed that may also be included if not covered in other courses include oral care, insomnia, and weight loss.
Table 2.
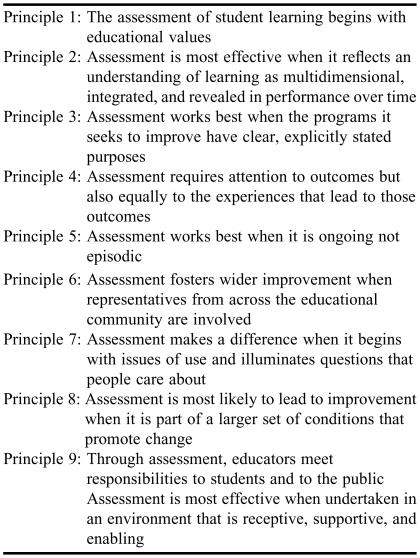
American Association of Higher Education's Nine Principles of Good Practice for Assessing Student Learning
The specific topic categories include both symptom and product-based categories. For symptom-based categories, topics would include prevalence, epidemiology, etiology, transmission, symptom-based diagnostic schemata, specific considerations, and treatment for the specific condition:
Symptoms related to viral and bacterial respiratory infections, respiratory allergies.
Related symptoms include fever, nasal symptoms, sore throat, ear pain or discharge, and cough. Other conditions related to the common cold, such as influenza and bacterial sinusitis, should also be included. Allergic rhinitis and asthma fall under this category because they are common, chronic forms of airway disease that have symptoms similar to the common cold and must be differentiated from infectious processes when making appropriate recommendations or referrals.
Symptoms involving headache or musculoskeletal pain.
The following subcategories of pain that can be incorporated into the curriculum include headache, muscle and joint pain (strains, sprains, repetitive strain injury), contusions, back pain, sciatica, musculoskeletal injuries and disorders (ankle, knee, and tendon injuries), and arthritis.
Symptoms related to the gastrointestinal tract.
The following subcategories of gastrointestinal disorders that can be incorporated into the curriculum include heartburn, abdominal pain, nausea and vomiting (motion sickness), intestinal gas discomfort (bloating, flatulence, and colic), lactose intolerance, constipation, diarrhea, pinworm infestations, anorectal disorders (hemorrhoids), poisoning emergencies, and ostomy care and supplies.
Symptoms involving skin and soft tissue.
The following subcategories of dermatological conditions and disorders that can be incorporated into the curriculum include atopic dermatitis, hyperproliferative skin disorders (dandruff, seborrheic dermatitis, psoriasis, cradle cap), arthropod stings and bites, pediculosis, scabies, minor wounds, cellulitis, burns, sun-induced skin damage, acne, fungal skin infections, warts, contact dermatitis and poison ivy/oak/sumac, diaper dermatitis, skin hyperpigmentation (solar lentigines, ephelides, melasma), foot problems (corns, calluses, bunions, blisters, high arches, ingrown toenails), hair loss, and unwanted hair.
Symptoms specific to females.
Self-treatable conditions related to women's health can include vaginal and vulvovaginal disorders such as vaginal dryness and vulvovaginal candidiasis, along with disorders related to menstruation such as dysmenorrhea, menorrhagia, menopause, dysuria, and premenstrual symptoms. Information related to contraceptive products should also be included.
Symptoms related to the eye and ears.
Ophthalmic conditions can include dry eye, redness and discomfort of the eye, allergic conjunctivitis, corneal edema, and prevention of contact lens-related disorders. Otic conditions can include cerumen impaction, prevention of infections of the external ear canal, and ear pain.
Smoking/tobacco cessation products.
Nonprescription products for smoking/tobacco cessation should be the primary focus of the material presented, as well as behavioral change models (eg, transtheoretical) that assess a patient's readiness to quit and encourage appropriate counseling for the patient's stage of change.
Home diagnostic products (including self-monitoring of blood glucose).
Topics to be covered include a category-by-category overview of the home diagnostic testing kits/devices available for patients. These could include screening tests for pregnancy, detection of ovulation, screening for colorectal cancer, self-detection of urinary tract infections, screening for illicit drugs, screening for HIV, screening for high cholesterol levels, and monitoring of Hemoglobin A1C. In addition, many devices exist for monitoring chronic conditions, eg, diabetes. Students should be provided with an overview of devices that are used by patients for monitoring blood glucose. In addition, insulin syringes, insulin pens, and other insulin-related accessories can be presented, if not incorporated into other courses within the pharmacy curriculum.
Vitamins, minerals, dietary supplements, and herbal products.
Topics to be covered should include patient assessment to determine the need for vitamin and mineral supplementation, common terminology used to describe vitamin and mineral products, regulation of dietary supplements and herbal products, and general information about the many different products within these broad categories. Instruction should be based on evidence-based medicine.
A number of different methods can be utilized to incorporate these core curriculum topics into classroom learning. A few pharmaceutical manufacturing companies offer sample nonprescription medicine products that can be demonstrated and distributed for inspection during class. In addition, students could be required to complete product-oriented, performance-based activities that could include items such as a virtual family with the need for nonprescription product recommendations or a cost comparison activity that evaluates different products within similar therapeutic categories. These activities would be designed to familiarize the students with the plethora of nonprescription products currently available on the market, so the students become more comfortable and confident in helping patients make product decisions and selections.
The ideal situation would be to provide active-learning instruction in the core curriculum topics within a standalone course. However, given the nature of pharmacy curricula, other methods for incorporating this material are through integration in pathophysiology and therapeutics courses, laboratory and skills-based courses, and experiential education. Even so, many NMA faculty members have found that coverage of nonprescription medication topics decreases when a standalone course is not provided and content must be incorporated into other courses.
INSTRUCTIONAL METHODOLOGY
Instruction in nonprescription medications in colleges and schools of pharmacy should include a variety of methods to enhance and support student learning. Students have different learning styles. When faculty members recognize the different capabilities of students and utilize different methods of instruction, this will have a long-lasting effect on the student's ability to retain and apply the knowledge gained.14,15
In a 2003 survey by Covington, most nonprescription medication courses incorporated traditional lecture and case-based instruction. Some courses utilized problem-based learning, computer-assisted instruction, and self-instruction modules. Other pharmacy programs taught nonprescription drugs in the laboratory or experiential learning environment.16
Only recently have pharmacy faculty members ventured outside of pharmacy literature for guidance on how to teach. Lessons learned from schools that specialize in preparing teachers and educational research have begun to appear in pharmacy andragogy. Several pharmacy faculty members have incorporated innovative approaches to teaching nonprescription medications within their curriculum. Chambers, Schmittgen, and Allan incorporated peer teaching within a pharmaceutical care laboratory. They found that the students were successful in learning from their peers and enjoyed the interaction.17 Another approach is using treatment algorithms as a tool for students to learn a decision-making process regarding nonprescription medications for a patient with a specific symptom or condition.18 Tools such as role playing, games, positive incentives, reflection, journaling, and small group interactions are appearing in nonprescription instruction. In a series of published articles in the Journal regarding teaching and learning in a nonprescription medications course, Sibbald reported using a number of active-learning instructional methods to engage students.19-21 Computer-assisted instruction has promoted independent learning, team building, and enhancement of technological skills. Students are actively involved in development of the tools necessary to provide opportunities for learning for themselves and future students. One group of students has produced a consumer web site for nonprescription drugs (ie, CareNet) and a web-based tool incorporating attainment of knowledge, development of cases, and questions to assess a student's understanding of the material (VITAL: a virtual interactive case tool for asynchronous learning).21
Faculty members also have a responsibility to provide the foundation for students to develop as life-long learners, utilizing evidence-based medicine to help guide their self-care recommendations. Several instructional methods have been successful in developing life-long learning skills in professional students. Instruction that includes the use of multiple information resources, goal setting, team-building, cooperation, and reflection can lead to a solid foundation for future learning.22
COURSE MECHANICS
The actual mechanics of self-care courses vary widely among programs. Instruction in nonprescription medications and self-care is integrated into the curriculum in a variety of ways depending upon the curricular philosophy of the school and its faculty members. This includes separate stand-alone courses and integration into courses such as pharmacotherapeutics, community pharmacy practice laboratories, pharmacology, and experiential education. The course(s) may be integrated into the curriculum as a required or elective course. In some programs, the course(s) may be a combination of the aforementioned formats.
Course andragogy varies among programs. In some schools, nonprescription medicine courses are didactic, consisting of lectures only. In other schools, recitations and laboratories may be a course component as well as featuring problem-based learning modules. Some nonprescription medication courses are taught as part of the experiential series and are primarily “hands-on” in nature.
Another issue surrounding nonprescription medicine courses is the academic credentials and standing of the faculty member. In some cases, adjunct or part-time faculty members teach the course. In other cases, full-time pharmacy faculty members with expertise in self-care teach the course. The question has been raised as to whether nonprescription therapeutics is a specialty similar to pediatrics, antithrombosis, or other pharmacy specialty areas. In some programs and in the eyes of some students, self-care courses are not considered in the same light as pharmacotherapeutics courses or other core courses even though many are just as rigorous. There is also discussion about the need for postgraduate education opportunities, eg, specialty residency in self-care.
Course credit hours also vary among schools. According to the 2003 survey, nonprescription medicines courses in US colleges and schools of pharmacy varied in credit hours from 1 hour to 6 semester hours with the majority of courses being assigned 3 credit hours.16
Another issue that needs to be considered is the placement of these courses in the curriculum. There are varying arguments for placing the course in the first-professional year, the last professional year, and in the intermediate curricular years. Teaching the course in the first-professional year enhances professionalization and provides pharmacy content early in the curriculum when many students are enrolled in basic science courses. It also gives the student useful information for early practice experiences where they are able to apply the knowledge. On the other hand, teaching the course later in the curriculum after pathophysiology and pharmacology have been taught allows the professor to spend more time on the pharmacotherapeutics of nonprescription therapy. Further, students are closer to beginning their advanced pharmacy practice experiences where they will be interacting with real patients and most need this information. While neither approach is perfect, placement in the curriculum is an important consideration.
IMPORTANCE OF CURRICULUM MAPPING
The content of a specific pharmacy course and class hours devoted to each topic can be incorporated into a spreadsheet map. The purpose of such a map is to create a document that can be utilized by the pharmacy curriculum committee and by faculty members to assess coverage of course content across the curriculum. It is easy to lose site of the broad curricular structure when constant revisions and modifications are being made. When developing an assessment strategy, one must consider how each characteristic of the assessment relates to course instruction and learning outcomes. Consider: (1) the nature of the task, (2) the level of cognitive processing students should demonstrate, and (3) the appropriate setting for the assessment. The instructor must map the types of knowledge the student is expected to use in accomplishing the course objectives. It is imperative to prospectively connect the objectives, assessment tool, and desired level of cognitive processing to identify repetition and potential disconnects.
ASSESSMENT OF STUDENT COMPETENCIES IN SELF-CARE
Assessment techniques include traditional types of tools such as multiple-choice questions, open-ended questions, and performance-based examinations such as standardized patients and oral examinations. Before providing details about traditional assessment tools and their use in a self-care, nonprescription medications course, educators must recognize that the types of knowledge and the selection of an appropriate assessment tool differs for each. Essentially, there are 3 types of knowledge recognized by cognitive psychologists: declarative, procedural, and conditional knowledge.23 Declarative knowledge is defined as “knowing that.” Examples include facts and verbal information obtained through readings and/or didactic lectures. Multiple-choice questions, open-ended questions, and oral examinations would be appropriate tools for assessing this type of knowledge. Procedural knowledge is defined as “knowing how” to perform a skill or apply concepts. Filling a prescription and entering a medication order into a computer are examples of procedural knowledge. However, if the student was asked to explain how to fill a prescription, it would be considered declarative and not procedural because the student did not actually do anything other than provide a verbal description. Knowing when and why to use declarative or procedural knowledge is considered conditional knowledge.20 An example of conditional knowledge is a pharmacist using her therapeutics knowledge to determine that a patient has hypertension based on his current medications and that using an oral nasal decongestant such as pseudoephredrine would not be recommended if the patient's blood pressure is significantly elevated. Performance-based assessment, as implied by the ACPE, requires that students actually perform, demonstrate, construct, etc, and should be used for procedural and conditional knowledge.5 Another way to categorize cognitive education is via Bloom's taxonomy. Benjamin Bloom and a group of educational psychologist identified 6 levels within the cognitive domain, which involves knowledge and the development of intellectual attitudes and skills. The hierarchy of levels from lowest to more complex is knowledge, comprehension, application, analysis, synthesis, and evaluation. The lowest levels of Bloom's taxonomy relate to declarative knowledge (simple facts or recall) and the more complex levels are associated with procedural and conditional knowledge. When developing an assessment tool, it is useful to assess a student's understanding using the various levels of Bloom's taxonomy.24
Traditional Testing Techniques
There is tremendous value to using multiple-choice questions in a self-care nonprescription medications course. Multiple-choice questions allow the educator to assess students’ basic knowledge of the self-care condition and drugs used in the treatment of that condition (Bloom's taxonomy of objectives: lower levels - knowledge and comprehension). In addition, multiple-choice questions that are well-planned and crafted by the educator allow the student to identify, evaluate, and solve a drug-related problem or treat a self-care problem (Bloom's taxonomy of objectives: higher levels – application and analysis). Therefore, multiple-choice questions in a self-care course have a significant role, but using them as the only form of assessment fails to evaluate performance-based knowledge (skills – communication/counseling, and attitude), which must be tested using higher-order thinking (ie, synthesis and evaluation) on an essay-type examination.
Open-ended questions are valuable in a self-care nonprescription medication course as they can test complex learning outcomes and the student's thought process without providing the answer as in multiple-choice questions. Using this type of assessment format allows for several correct answers with justification based on the clinical case. Open-ended questions can be created so that the educator can evaluate the student's thought process in gathering the key data and selecting the best option based on patient-specific information. Further, it can provide feedback to the student on what he/she knows or does not know related to that condition or drug, or to patient counseling tips.
Performance-based Assessment Techniques
Four primary performance-based assessments have been used in the health sciences: patient management problems, problem-based learning (PBL), oral examinations, and standardized patients/OSCEs. Five primary types of evaluation methods are used with performance-based assessments: scoring rubrics, task-specific scoring guides, rating scales, checklists, and written, and oral comments. Evaluative data in self-care nonprescription medicine curriculum can be obtained from a variety of methods which may include: rubrics, self-evaluation/peer evaluation, oral and written examinations, assignments, papers, questionnaires, patient interviewing, role-playing, simulations, objective structured clinical examination, portfolios, and direct observation in clinical practice. These tools assess the higher levels of Bloom's Taxonomy of Objectives (ie, application, analysis, synthesis, evaluation). The nonprescription medicine curriculum correlates with a performance-based curriculum.
Case Simulations/Problem-based Learning
Case simulations are instructional techniques designed to promote learning and problem-solving skills. Value added to a self-care curriculum by incorporating case simulations and problem-based learning includes: improvement in problem-solving skills, increased utilization and understanding of resources, improvement in communication skills, facilitation of intradisciplinary and interdisciplinary learning, preparation for clinical rotations and residency training, and integration and application of evidenced-based medicine. Potential problems of using this type of assessment include: the additional resources required, inconsistency and inter-rater reliability issues among course facilitators, less student exposure to a broad range of content areas, student anxiety, and the increased workload for students and faculty members.
Standardized Patients/Objective Structured Clinical Examinations
An objective structured clinical examination is a series of interactive and non-interactive stations whereby all candidates rotate through patient-care stations on a timed basis. Interactive stations utilize standardized patients trained to present a case in a standardized manner and non-interactive stations that require written responses to tasks or problems without direct observation and assessment. Generally, checklists are used to judge student performance. The value of an objective structured clinical examination in self-care instruction and student assessment includes increased development of communication and interpersonal skills; identification of ethical conflicts and improved professional judgment; demonstration of integration and application of evidenced-based medicine.
Oral Examinations
Oral examinations can be used to assess clinical decision making, synthesis, analysis, and dissemination of information to the public. Oral examinations can be considered a performance-based assessment that most resembles the way counseling patients about self-care occurs.
RECOMMENDATIONS
Self-care is a growing and important part of pharmacy curricula. This manuscript has outlined the need for self-care in pharmacy education including in current standards and resources for curriculum design, the desired core curriculum, possible instructional methodology, different scenarios for course mechanics, and information about assessment. NMA faculty members strongly recommend addressing the following points when developing or modifying a self-care curriculum:
The doctor of pharmacy curriculum should have no less than 60 contact hours of self-care instruction. The majority of this instruction should occur within a standalone course, supplemented with reinforcement in other courses including the experiential component of the curriculum.
Placement of a standalone course should be done concurrently or integrated with or follow pharmacology, pathophysiology, and patient assessment. Instructors should exchange information about these courses so that each complements the others and strengthens the instructional strategy.
Self-care instruction should use active-learning strategies within a performance-based curriculum.
Self-care courses should be taught by practitioner-educator faculty members who have practiced in a self-care environment.
Student assessment in a self-care course should be based on more than just multiple-choice examinations. Assessment methods such as case simulations should also be employed.
Topics in the core curriculum should at a minimum include symptoms involving viral and bacterial respiratory infections, respiratory allergies, gastrointestinal tract, eye and ear, women's health, headache and musculoskeletal pain, and skin and soft tissue, plus products for smoking cessation, home diagnostics, and wellness maintenance (vitamins, dietary supplements and herbal products). Attention should be paid to special populations within these topic areas.
We hope that this article will help faculty members examine current self-care offerings in colleges and schools of pharmacy to ensure that their professional students are prepared to meet the challenge of pharmacist-assisted self-care.
Table 1.
Suggested Core Self-Care Topics for a Doctor of Pharmacy Curriculum*
*Each topic should include the process of self-care (including patient assessment and triage), emerging issues in nonprescription medicines, the incorporation of special population groups, and cultural competence.
ACKNOWLEDGMENTS
The authors would like to thank Procter and Gamble for their generous and continued support of the Nonprescription Medicines Academy since 1998. Further, the authors acknowledge the recommendations for this manuscript made by Gail D. Newton, PhD, Associate Professor of Pharmacy Practice, Purdue University School of Pharmacy and Pharmaceutical Sciences, and Richard N. Herrier, PharmD, Clinical Associate Professor of Pharmacy Practice, University of Arizona, College of Pharmacy.
REFERENCES
- 1.Covington TR. OTC drugs: an undervalued opportunity? Drug Top. 2000;144:16. [Google Scholar]
- 2. The National Council on Patient Information and Education. Uses and attitudes about taking over-the-counter medicines. Available at: http://www.bemedwise.org/survey/summary_survey_findings.pdf. Accessed November 03, 2005.
- 3.Barnes PM, Powell-Griner E, McFann K, et al. Top Selling Herbs. Adv Data. 2004:1–19. [PubMed] [Google Scholar]
- 4. Updated NAPLEX(R) Blueprint for distribution.doc. Available at www.nabp.net/ftpfiles/NABP01/updatednaplexblueprint.pdf. Accessed November 8, 2005.
- 5. Revised Pharm.D. Standards American Council on Pharmaceutical Education, Chicago. 2006. Available at http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed November 28, 2006.
- 6. Pharmacists. U.S. Department of Labor. http://www.bls.gov/oco/ocos079.htm. Accessed November 21 2005.
- 7.Berardi RR, editor. Handbook of Nonprescription Drugs. 14th ed. Washington, DC: American Pharmacists Association; 2004. [Google Scholar]
- 8.Pray WS. Nonprescription Product Therapeutics. 2nd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 9.Hamacher Resource Group. Best of the bunch: which were the winningest OTCs/HBCs launched in 2004? Drug Top. 2005;149:38,44–6. [Google Scholar]
- 10.American Pharmacists Association. Pharmacists’ picks of top OTCs. Pharm Today. 2004;10:22–6. [Google Scholar]
- 11.Bennett DL, Chown P, Kang MS. Cultural diversity in adolescent health care. Med J Aust. 2005;183:436–8. doi: 10.5694/j.1326-5377.2005.tb07113.x. [DOI] [PubMed] [Google Scholar]
- 12.Hunt LM, de Voogd KB. Clinical myths of the cultural “other”: implications for Latino patient care. Acad Med. 2005;80:918–24. doi: 10.1097/00001888-200510000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Purden M. Cultural considerations in interprofessional education and practice. J Interprof Care. 2005;19:224–34. doi: 10.1080/13561820500083238. [DOI] [PubMed] [Google Scholar]
- 14.Austin Z. Development and Validation of the Pharmacists' Inventory of Learning Styles (PILS) Am J Pharm Educ. 2004;68 Article 37. [Google Scholar]
- 15.Shuck AA, Phillips CR. Assessing Pharmacy students' learning styles and personality types: a ten-year analysis. Am J Pharm Educ. 1999;63:27–33. [Google Scholar]
- 16. Covington TR. National Curriculum Survey: Status of Instruction in Nonprescription Drug Therapy AACP Annual Meeting Salt Lake City, UT July 10–13, 2004.
- 17.Chambers SL, Schmittgen J, Allan CR. Evaluation of peer teaching in a pharmaceutical care laboratory. Am J Pharm Educ. 2000;64:283–8. [Google Scholar]
- 18.Nykamp D. Teaching clinical problem solving in a nonprescription medication course with treatment algorithms. Am J Pharm Educ. 1999;63:338–41. [Google Scholar]
- 19.Sibbald DJ. Innovative, problem-based, pharmaceutical care courses for self-medication. Am J Pharm Educ. 1998;62:109–19. [Google Scholar]
- 20.Sibbald DJ. Bridging the gap to practice pharmacy PBL students establish consumer website for nonprescription drugs. Am J Pharm Educ. 2000;64:339–48. [Google Scholar]
- 21.Sibbald DJ. Virtual interactive case tool for asynchronous learning: PBL students develop online resource for nonprescription drugs. Am J Pharm Educ. 2003:67. Article 19. [Google Scholar]
- 22. Dunlap, JC. Preparing Students for Lifelong Learning: A Review of Instructional Methodologies 1997 Proceedings of Selected Research and Development Presentations at the 1997 National Convention of the Association for Educational Communications and Technology Albuquerque NM February 1997.
- 23.Garavalia LS, Marken PA, Sommi RW. Selecting appropriate assessment methods: asking the right questions. Am J Pharm Educ. 2003;66:108–12. [Google Scholar]
- 24. Bloom's Taxonomy http://www.officeport.com/edu/blooms.htm Accessed February 16, 2006.