SYNOPSIS
In collaboration with the Centers for Disease Control and Prevention, participating state and local health departments, universities, and community-based organizations applied venue-based, time-space sampling methods for the first wave of National HIV Behavioral Surveillance of men who have sex with men (NHBS-MSM). Conducted in 17 metropolitan areas in the United States and Puerto Rico from November 2003 through April 2005, NHBS-MSM methods included: (1) formative research to learn the venues, times, and methods to recruit MSM; (2) monthly sampling frames of eligible venues and day-time periods that met attendance, logistical, and safety criteria; and (3) recruitment of participants in accordance with randomly generated venue calendars. Participants were interviewed on HIV risk and prevention behaviors, referred to care when needed, and compensated for their time. By identifying the prevalence and trends of HIV risk and prevention behaviors, NHBS-MSM data may be used at local, state, and federal levels to help obtain, direct, and evaluate HIV prevention resources for MSM.
Well into the third decade of the HIV/AIDS epidemic in the United States, more cases of AIDS are reported among men who have sex with men (MSM) than among any other group.1 Outbreaks of syphilis and gonorrhea among MSM in several cities, coupled with high prevalence and incidence of HIV infection, suggest that HIV transmission may be increasing among MSM.2–10 With the exception of two longitudinal studies conducted in one U.S. city, however, routinely collected data on HIV risk and prevention behaviors among MSM do not exist.4,11,12 As a consequence, insufficient behavioral data have prevented optimal use of HIV prevention resources in several U.S. communities.13 HIV behavioral surveillance, an ongoing systematic collection, analysis, and interpretation of HIV risk and prevention behaviors, is needed to help obtain, direct, and evaluate the use of HIV prevention resources for MSM.14–16
The systematic collection of data on representative samples of MSM, however, presents many challenges, since population lists of MSM do not exist and use of general population surveys yield insufficient samples of MSM.17,18 Moreover, to be relevant, HIV behavioral surveillance must adequately represent MSM subgroups at greatest risk of infection, such as those who are young and black or Hispanic.5,7,9,19–22 These important groups, however, can present even greater challenges for sampling. For example, although several
population-based telephone surveys have purported to obtain representative samples of MSM, these surveys enrolled few young minority MSM, even when conducted in metropolitan areas that have considerable racial and ethnic diversity.6,23,24 While convenient, clinic-based surveys are subject to considerable biases, including underrepresenting those MSM who do not regularly obtain health care.
Pioneered by the CDC in 1994, venue-based, time-space sampling has been used in several research studies to obtain large and diverse samples of young and minority MSM.25–27 Methods used in these studies adapted strategies of traditional time-space surveys to sample flows of human populations.18,28 Given the success of these studies in multiple cities in the 1990s, venue-based, time-space sampling was used for the first wave of National HIV Behavioral Surveillance for MSM (NHBS-MSM).5,21,29–31 This article describes the national application of this sampling approach.
LOCATIONS, PARTNERS, AND SAMPLE REQUIREMENTS
Surveillance period, locations, and partners
The first wave of NHBS-MSM was implemented from November 2003 through April 2005 by staff from state and local health departments, universities, and community-based organizations in the following 17 metropolitan statistical areas (MSAs): Atlanta, GA; Baltimore, MD; Boston, MA; Chicago, IL; Dallas, TX; Denver, CO; Ft. Lauderdale, FL; Houston, TX; Los Angeles, CA; Miami, FL; Newark, NJ; New York City, NY; Philadelphia, PA; San Diego, CA; San Francisco, CA; San Juan, PR; and Washington, DC. The second wave of NHBS-MSM is projected for 2008 after the completion of the first wave of behavioral surveillance for injecting drug users and heterosexuals at risk.32
Sample size
The minimum sample size for the first wave of NHBS-MSM was 500 MSM recruited at eligible venues located within the MSA. This sample size was selected to yield adequate precision in estimating the prevalence of behavioral outcomes of interest, and because previous surveys demonstrated that recruiting 500 MSM was feasible given available resources and the anticipated need to complete recruitment within a nine-month period.
Eligibility
To be eligible for the first wave of NHBS-MSM, all potential participants must have been: (1) men or transgender people born male who were approached by surveillance staff at sampled venues, (2) 18 years of age or older, (3) residents in a locally defined geographic area of interest, (4) first-time participants, and (5) able to speak English or Spanish. Male-to-male sexual behavior was not an eligibility requirement so that all MSM could participate, including those reluctant to disclose their sexual orientation during a brief eligibility interview.
METHODS
Overview
Local surveillance staff conducted venue-based, time-space sampling in accordance with a national protocol that organized activities into three components. In the first component, staff conducted formative research to learn the spaces (venues), times, and methods to recruit MSM. In the second component, staff constructed monthly sampling frames of eligible venues and venue-specific, day-time periods (VDTs) (e.g., a dance club on Fridays from 10:00 p.m. to 2:00 a.m.) that met MSM attendance, logistical, and safety eligibility criteria. From these frames, staff randomly selected a set of venues and VDTs in two stages and scheduled these on monthly calendars. In the third component, staff recruited and interviewed men during sampling events conducted in accordance with monthly calendars. Given the alternating cycle of behavioral surveillance for the three targeted populations of MSM, injecting drug users, and heterosexuals at risk, we anticipated having a maximum of 12 months to complete each wave of NHBS-MSM.32 Of these 12 months, three would be devoted to formative research and nine would be devoted to recruiting and interviewing. In the first wave of NHBS-MSM, however, additional resources were provided to allow participating organizations more time to complete both formative research and recruitment.
LEARNING ABOUT VENUES, TIMES, AND METHODS
Venue eligibility
Venues eligible for consideration for NHBS-MSM were defined as public or private locations attended by MSM for purposes other than receiving medical, mental health, social, or HIV/STD diagnostic testing or prevention services. In addition, eligible venues had to be logistically feasible and reasonably safe. Typical NHBS-MSM venues included bars, dance clubs, retail businesses, cafes and restaurants, health clubs, social and religious organizations, adult bookstores and bathhouses, street locations, parks, beaches, and special events (e.g., Gay Pride).
Formative research
Formative research was conducted to learn about the venues, times, and methods to recruit MSM. To meet these objectives, staff reviewed advertisements for MSM in online and print media, interviewed key informants, and conducted observations at venues. Key informant interviews were conducted with MSM, MSM researchers, and knowledgeable staff of state and local health departments, prevention planning groups, community-based organizations, service providers, and commercial and social MSM venues. To help ensure that all potential venues were identified, interviews were conducted with key informants of different age groups, race/ethnicities, and sexual orientations.
For each venue identified in these interviews, staff collected information on MSM attendance during specific days and times; the estimated distribution of patrons by race, age group, and sexual orientation; safety issues; and management contact information (if applicable). Staff also asked key informants about participation motivations and disincentives, optimal referrals for prevention and health-care services, and needs for coordination with other venue-based research and prevention efforts. When applicable, staff met with venue owners or managers to solicit their approval to conduct NHBS-MSM on their property.
Finally, staff observed MSM attendance and patron flow patterns at identified venues to learn how recruitment and interview methods might be optimally applied (logistics). If initial formative research did not yield sufficient information on attendance, staff conducted 30- to 60-minute enumerations of male patrons within identified VDTs. If the proportion of male patrons who were MSM was also unknown or thought to be low (e.g., at street locations, mixed clubs, parks), staff would approach counted men to ascertain their demographic, residence, and sexual-behavior characteristics. These data were then used to estimate the number and proportion of eligible MSM who attended VDTs. VDTs estimated to yield >75% MSM of men approached were considered MSM venues.
Based on reviews of media, interview, observation, and enumeration data, staff constructed an initial “universe” of MSM venues and their attendance, safety, and logistical characteristics. The initial universe was considered complete (robust) when only known MSM venues continued to be identified through formative research. Although the bulk of formative research was conducted initially, some research was continued throughout the surveillance period to ensure that new MSM venues were included in the universe and that monthly sampling frames (below) remained robust.
CONSTRUCTING VDTS, SAMPLING FRAMES, AND CALENDARS
VDT attendance criterion
Once the initial universe of MSM venues and attendance patterns was identified, sampling frames were constructed of the set of eligible venues and VDTs expected to yield at least eight eligible MSM. To provide staff with reasonably consistent work schedules, VDTs were constructed as much as possible in standard four-hour day-time periods (e.g., a dance club with six VDTs: Mondays through Saturdays from 10:00 p.m. to 2:00 a.m.). However, some venues had VDTs that lasted only one or two hours (e.g., a gay-bisexual student group that meets every other Wednesday for one hour). Provided these VDTs were estimated to yield eight eligible MSM and met all other eligibility criteria, they were also included in monthly sampling frames.
The attendance criterion of eight was used assuming that staff would approach seven, and of these, six would agree to be screened for eligibility and at least four would agree to participate. These assumptions were based on observed approach, screening, and participation rates of previous venue-based, time-space sample surveys of MSM.5,21,29–31 Conducting a minimum of four interviews per sampling event and 14 events per month during an anticipated nine-month survey would yield a minimum of 500 participants.
Sampling frames, venue selection, and sampling calendars
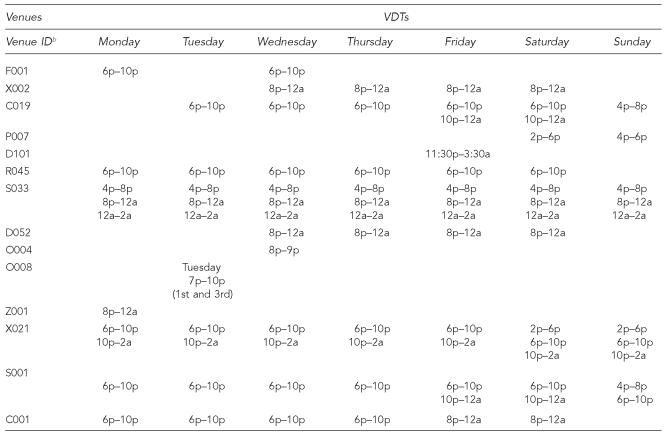
NHBS-MSM sampling frames were composed of two lists. The first list included the set of eligible venues, and the second list was the set of VDTs of each venue that was expected to yield at least eight eligible MSM (Figure 1). Sampling frames were updated on a monthly basis from ongoing formative research.
Figure 1.
Hypothetical sampling frame of MSM-identified venues and associated venue-specific, day-time periods (VDTs)a
a VDTs are venue-specific, day-time periods expected to yield a minimum of eight eligible MSM.
b B = bar; C = café or restaurant; D = dance club; F = fitness club or gymnasium; G = Gay Pride or similar event; H = house party; O = social organization; P = park or beach (not public sex environment); R = retail business; S = street location (e.g., corner); V = rave, circuit party, or similar event; X = sex establishment or environment; Z = other
MSM = men who have sex with men
From updated sampling frames, staff selected venues and corresponding VDTs in two separate stages. In the first stage, a set of venues equal to the number of sampling events planned for the upcoming month was randomly selected without replacement. In the second stage, one VDT was randomly selected from the set of available VDTs of each venue selected. Sampling was conducted in two separate stages to give venues an equal probability of selection to maximize representation of MSM from different venues, and to minimize burden on venue owners and patrons.
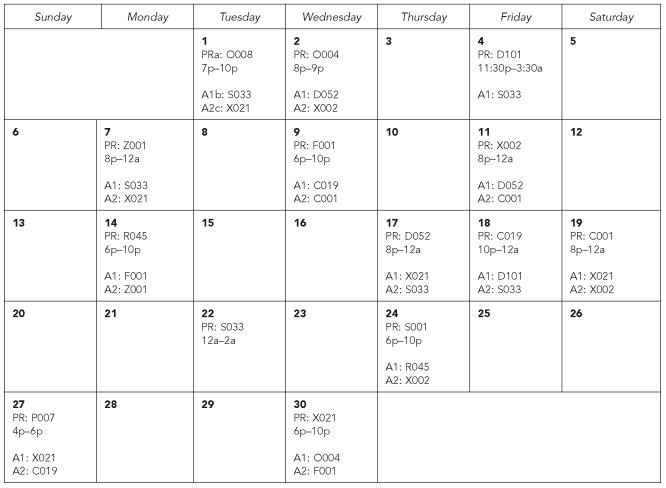
To construct monthly sampling calendars, selected VDTs were scheduled on the calendar as primary sampling events (Figure 2). Although venues and VDTs were randomly selected, actual sampling dates were purposefully chosen. For example, if a bar on Wednesday nights was randomly selected, staff could schedule that bar on any available Wednesday of the upcoming month. Dates were purposefully chosen to accommodate administrative and staff needs.
Figure 2.
Hypothetical sampling calendar for venue-based, time-space sampling of MSM
MSM = men who have sex with men
a PR = primary sampling event
b A1 = first alternate venue
c A2 = second alternate venue
Because venues may be poorly attended at any given time, two alternate venues (if available) were randomly selected from the set of venues in the sampling frame that had VDTs that began on, within, or at the end of the scheduled primary sampling event (Figure 2). These alternate venues could be used only if the primary venue was closed or very poorly attended. Finally, because some important events are known to occur only once a year (e.g., Gay Pride or circuit parties) or a few days in advance (e.g., raves), staff could purposefully select up to a maximum of three different venues each month. Complete with alternate and non-randomly selected venues, the sampling calendar was then ready for use in the upcoming month.
CONDUCTING SAMPLING EVENTS
Enumeration and eligibility interviews
Depending upon expected attendance at venues, teams of from two to five staff members conducted sampling events at venues in accordance with monthly calendars. During sampling events, all men who appeared ≥18 years of age and who crossed an imaginary line or entered a defined space were counted. Lines or spaces were located at venues based on logistical considerations learned during formative research. When staff members were available, counted men were approached consecutively and asked to stop and complete a brief eligibility interview. Recruiters were trained to approach men from the front in a comfortable style; to appropriately identify themselves, their organization, and their purpose; and to conduct the eligibility interviews as confidentially as possible. Clearly recognizable project clothing (e.g., T-shirts with project logo), identification badges, or a clipboard or handheld computer were used to help assure clients that approaches were legitimate and nonpersonal.
Trained staff used handheld computers or paper questionnaires to ask a standard series of questions to assess eligibility. In addition to age, race, and residence information, all men were asked if they had been approached before about NHBS-MSM (identified by local project name), and if so, whether they had previously participated. Previous participants were informed they were no longer eligible; previous nonparticipants who continued to meet all other eligibility criteria were encouraged to participate. All identified eligible men were invited to participate in a standard interview lasting approximately 25 minutes. Participation in NHBS-MSM was anonymous; participants were not required to provide their names or other personal identifiers as a condition for participation.
Interviews, referrals, and reimbursement
Eligible men who agreed to participate were accompanied to a prearranged location where interviews could be conducted in private. These locations included secluded areas within or outside the venue, in a nearby location (e.g., café), or in an interview van. Trained staff used handheld computers or paper questionnaires to administer standard interviews. The interview included a core set of measures on participant socio-demographic characteristics; sexual, drug-use, and HIV testing behaviors; and site-specific measures on knowledge and use of local HIV prevention programs and services.32 When the interview was completed, staff provided prevention materials and referrals for HIV prevention and health-care services (when needed), and reimbursed participants $25 for their time.
HUMAN SUBJECTS PROTECTIONS
Participation in NHBS-MSM was voluntary and anonymous; names or other personal identifiers were not collected as a condition for participation. Participants could refuse to answer any question or stop the interview at any time. NHBS-MSM eligibility forms, questionnaires, and other surveillance instruments were stored in locked filing cabinets or password protected handheld and desktop computers. Files and computers were maintained in secure office environments with limited and controlled access. Because NHBS-MSM is a public-health surveillance activity used for disease control program or policy purposes, CDC determined that it was not research. At some participating sites, however, Institutional Review Board approval for NHBS-MSM was obtained in accordance with state or local policies on human subjects protections.
QUALITY ASSURANCE
As part of quality assurance, CDC trained surveillance staff on NHBS-MSM formative research, sampling, recruitment, and interview procedures; conducted site visits during the formative research and recruitment periods; and reviewed submitted reports and data. Before conducting the first sampling event, all participating organizations were required to submit and receive CDC approval of a formative research report that included a summary of key informant interviews, the identified universe of MSM venues and VDTs, and the first month's sampling frame and calendar. After the first event, all organizations submitted sampling frames, calendars, and recruitment and interview data on a regular basis for additional quality assurance purposes.
Sampling frames and calendars were used at CDC to monitor the type and number of venues available for sampling, potential venue and VDT sampling violations, and the number of sampling events scheduled and completed. Recruitment data were used to identify (1) the estimated number of eligible men available for recruitment, (2) the proportion of men approached who agreed to an eligibility screen, (3) the proportion screened who were determined to be eligible, and (4) the proportion of eligible men who agreed to participate. These outcomes were used to evaluate potential biases and to assess progress toward meeting NHBS-MSM recruitment goals. These goals included: (1) conducting an average of 14 sampling events per month, (2) completing eligibility screens on ≥90% of enumerated men approached, and (3) enrolling ≥75% of eligible men identified. When needed, CDC consulted with staff to explore alternative methods to identify MSM venues, clarify required sampling and recruitment procedures, and identify potential solutions to meet recruitment goals.
DISCUSSION
Although several recent surveys suggest ongoing high levels of risk behavior among MSM recruited in several U.S. cities, their utility for monitoring national trends has been limited given their considerable differences in participant eligibility criteria, research designs, and behavioral measures.5–7,11,12,19–22,29–31 For the first time, data on a standard set of HIV risk and prevention behaviors will be collected on large samples of MSM obtained under one standard protocol in 17 communities in the United States and Puerto Rico. Data from upcoming surveillance waves may be used to evaluate behavioral differences over time to help identify emerging epidemiologic trends and opportunities for prevention among MSM. While preliminary findings suggest that our method has again yielded adequate samples of MSM and reaffirmed ongoing high HIV risks, particularly among young black MSM, the successful application of venue-based, time-space sampling presents several methodological and analytic challenges.33
Methodological challenges
Three of the most important methodological challenges include (1) hiring and retaining appropriate staff, (2) obtaining requisite community support, and (3) balancing efforts to meet both ongoing formative research and MSM recruitment needs.
Appropriate staff.
While appropriate staffing is critical to the success of all projects, NHBS-MSM requires staff who are able to meet several unique demands. First, during an approximately nine-month period, NHBS-MSM staff must be able to work schedules that are highly variable and that frequently require working late night and early morning hours, on Fridays and weekends, and in outdoor settings and poor weather. Second, staff must not only be detail oriented to collect valid and reliable data in many different venues, but must also be able to avoid or minimize common adverse events that might occur in these venues (e.g., disruptions from intoxicated or irate patrons). Avoidance of adverse events is particularly important for NHBS-MSM given its long-term reliance on community support to access venues and MSM. Finally, staff must be able to identify, gain access to, and work effectively in all MSM venues including those attended by specific MSM racial/ethnic groups and subcultures. While this was challenging, organizations were able to hire staff that met these demands. NHBS-MSM teams were typically comprised of one full-time supervisor and four to eight full- and part-time men and women who were highly motivated, committed to NHBS-MSM goals, cross-culturally competent, and racially/ethnically diverse.
Community support.
Obtaining community support is fundamental for achieving robust sampling frames, high participation rates, and ultimately large and diverse samples of MSM. However, limited time to develop the support needed to meet these objectives presented a considerable challenge. To expedite this process, several participating organizations utilized consultants or advisory boards composed of influential MSM community members. Many of these members participated in HIV prevention community planning groups (CPGs), local HIV/AIDS research or prevention efforts for MSM, or MSM community-based organizations or advocacy groups. Community advisory boards met on a regular basis to help develop project identities and marketing strategies; obtain community support to construct, purchase, or distribute marketing materials; assess the completeness of venue identification and guide formative research efforts; and gain access to important venues (e.g., some board members met with venue owners to explain the need for NHBS-MSM and resolve participation barriers). To minimize burden on venue patrons and management, many organizations also obtained the support of community prevention groups to prevent the co-occurrence of prevention outreach and NHBS-MSM recruitment activities at sampled venues.
Ongoing formative research.
Several participating organizations without prior experience with venue-based sampling of MSM were challenged with balancing the allocation of staff resources to meet ongoing formative research and MSM recruitment needs. For example, considerable staff resources were needed to clarify MSM attendance patterns at new venues and in cities that had many venues with seasonal MSM attendance (e.g., parks). To address these challenges, some organizations divided ongoing venue-identification responsibilities among key staff and community advisory board members. Also, the sampling period for the first wave of NHBS-MSM was extended to allow organizations without prior experience sufficient time to meet both formative research and sampling needs.
Analytical challenges
One of the most important analytical challenges with venue-based, time-space sampling is developing a valid mechanism that may be needed to adjust for unequal selection probabilities. Like traditional time-space sample surveys, an important feature of our method is that it produces a probability sample of visits to venues included within sampling frames.18,28 The visit, rather than the visitor, is the appropriate unit of analysis because over the course of the survey many MSM will visit and revisit many venues and thus have multiple chances of selection.18,28 In order to draw more meaningful conclusions about MSM, however, NHBS-MSM must treat the unit of analysis as the visitor, and thus potentially must address unequal selection probabilities.
To adjust for unequal selection probabilities in sample surveys, a weighted analysis can be used where the weight is calculated as the inverse of the participant's selection probability.18 Thus, in the case of NHBS-MSM, the more often a person visits VDTs, the higher the selection probability and the lower the weight that person contributes to the parameter estimate (e.g., proportion reporting unprotected intercourse). The true selection probability of an NHBS-MSM participant, however, cannot be known because the probability is based, in part, on the individual's attendance pattern at all available VDTs during the entire surveillance period. Thus, the analytical challenge is to construct and validate a weighting mechanism that uses venue-attendance data measured in the survey to estimate a participant's selection probability.
External validity
Provided that the above methodological and analytical challenges are met, NHBS-MSM findings may be generalized (externally valid) to the population of MSM ≥18 years of age who attend venues included in sampling frames and who reside within selected MSAs. Findings from the first wave of NHBS may not be valid for MSM <18 years of age, MSM who do not attend MSM-identified venues, or MSM who do not reside in the 17 selected MSAs.
Although some MSM do not attend MSM-identified venues, several surveys suggest that most attend one or more types of venues included in our sampling frames.17 For example, based on a telephone survey of 2,881 MSM in four U.S. cities from November 1996 through February 1998, the weighted prevalence of attending a gay bar, nightclub, or dance club at least once in the past year was 83.8%. Club attendance shown in this survey, however, varied by age group: 96.1% among 18–29 year olds; 90.8% among 30–39 year olds; 83.2% among 40–49 year olds; 62.7% among 50–59 year olds; and 45.7% among MSM ≥60 years of age (Lance Pollack, PhD, personal communication, 2003 Oct). Thus, the external validity of NHBS-MSM findings to older MSM residents (e.g., ≥50 years of age) within a selected MSA may be less compared with younger MSM.
In addition to older MSM, the external validity of our findings to all MSM within selected MSAs may decrease over time given the apparent increasing use of the Internet by MSM to meet sex partners.34–36 Research is currently underway to assess the proportion of MSM who use the Internet to meet other men and who do not attend the types of venues included within our sampling frames.37 This research, for example, may find that some MSM who are not “out” about their sexual orientation only use the Internet, rather than visit venues, to meet other men. If this limitation is found to be important, supplemental network or other survey methods such as respondent-driven sampling may need to be considered in future NHBS-MSM waves.38,39
CONCLUSION
Since 1994, state and local health departments have been directed to use a community-planning process to allocate federal HIV prevention resources based on emerging epidemiological trends.40 In several external reviews of prevention community planning, insufficient relevant and timely epidemiological data were identified as an important barrier to prevention planning, and as a result, some CPGs avoided developing prevention plans that prioritized population segments in greatest need of HIV prevention.13 A behavioral surveillance system that provides relevant, timely, and high-quality risk and prevention data is needed to help CPGs and state and local health departments construct evidence-based plans to appropriately direct local HIV prevention efforts for MSM. Moreover, behavioral surveillance data are needed at the federal level to measure progress in meeting strategic goals and to obtain the necessary resources to reduce HIV infection among MSM. Despite its challenges, a national application of time-space sampling can provide large and diverse samples of MSM to meet these important needs.
REFERENCES
- 1.Centers for Disease Control and Prevention (US) Volume 15. Atlanta: CDC; 2003. HIV/AIDS Surveillance Report. [Google Scholar]
- 2.Williams LA, Klausner JD, Whittington WL, Handsfield HH, Celum C, Holmes KK. Elimination and reintroduction of primary and secondary syphilis. Am J Public Health. 1999;89:1093–7. doi: 10.2105/ajph.89.7.1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fox KK, del Rio C, Holmes KK, Hook EW, 3rd, Judson FN, Knapp JS, et al. Gonorrhea in the HIV era: a reversal of trends among men who have sex with men. Am J Public Health. 2001;91:959–64. doi: 10.2105/ajph.91.6.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen SY, Gibson S, Katz MH, Klausner JD, Dilley JW, Schwarcz SK, et al. Continuing increases in sexual risk behavior and sexually transmitted diseases among men who have sex with men: San Francisco, Calif., 1999–2001, USA. Am J Public Health. 2002;92:1387–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Valleroy LA, MacKellar DA, Karon JM, Rosen DH, McFarland W, Shehan DA, et al. HIV prevalence and associated risks in young men who have sex with men. JAMA. 2000;284:198–204. doi: 10.1001/jama.284.2.198. [DOI] [PubMed] [Google Scholar]
- 6.Catania JA, Osmond D, Stall RD, Pollack L, Paul JP, Blower S, et al. The continuing HIV epidemic among men who have sex with men. Am J Public Health. 2001;91:907–14. doi: 10.2105/ajph.91.6.907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.CDC (US) HIV incidence among young men who have sex with men—seven U.S. cities, 1994–2000. MMWR Morb Mortal Wkly Rep. 2001;50(21):440–4. [PubMed] [Google Scholar]
- 8.Weinstock H, Dale M, Gwinn M, Satten GA, Kothe D, Mei J, et al. HIV seroincidence among patients at clinics for sexually transmitted diseases in nine cities in the United States. J Acquir Immune Defic Syndr. 2002;29:478–83. doi: 10.1097/00126334-200204150-00008. [DOI] [PubMed] [Google Scholar]
- 9.Vu MQ, Steketee R, Valleroy L, Weinstock H, Karon J, Janssen R. HIV incidence in the United States, 1978–1999. J Acquir Immune Defic Syndr. 2002;31:188–201. doi: 10.1097/00126334-200210010-00010. [DOI] [PubMed] [Google Scholar]
- 10.CDC (US) Increases in HIV diagnoses—29 states, 1999–2002. MMWR Morb Mortal Wkly Rep. 2003;52(47):1145–8. [PubMed] [Google Scholar]
- 11.Ekstrand ML, Stall RD, Paul JP, Osmond DH, Coates TJ. Gay men report high rates of unprotected anal sex with partners of unknown or discordant HIV status. AIDS. 1999;13:1525–33. doi: 10.1097/00002030-199908200-00013. [DOI] [PubMed] [Google Scholar]
- 12.Katz MH, Schwarcz SK, Kellogg TA, Klausner JD, Dilley JW, Gibson S, et al. Impact of highly active antiretroviral treatment on HIV seroincidence among men who have sex with men: San Francisco. Am J Public Health. 2002;92:388–94. doi: 10.2105/ajph.92.3.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnson-Masotti AP, Pinkerton SD, Holtgrave DR, Valdiserri RO, Willingham M. Decision-making in HIV prevention community planning: an integrative review. J Community Health. 2000;25:95–112. doi: 10.1023/a:1005125506642. [DOI] [PubMed] [Google Scholar]
- 14.Thacker SB, Berkelman RL. Public health surveillance in the United States. Epidemiol Review. 1988;10:164–90. doi: 10.1093/oxfordjournals.epirev.a036021. [DOI] [PubMed] [Google Scholar]
- 15.Mills S, Saidel T, Bennett A, Rehle T, Hogle J, Brown T, et al. HIV risk behavioral surveillance: a methodology for monitoring behavioral trends. AIDS. 1998;12(Suppl 2):S37–S46. [PubMed] [Google Scholar]
- 16.Anderson JE, Stall R. How many people are at risk for HIV in the United States? The need for behavioral surveys of at-risk populations. J Acquir Immune Defic Syndr. 2002;29:104–5. doi: 10.1097/00126334-200201010-00016. [DOI] [PubMed] [Google Scholar]
- 17.Harry J. Sampling gay men. Journal of Sex Research. 1986;22:21–34. [Google Scholar]
- 18.Kalton G. Sampling considerations in research on HIV risk and illness. In: Ostrow DG, Kessler RC, editors. Methodological Issues in AIDS Behavioral Research. New York: Plenum; 1993. pp. 53–74. [Google Scholar]
- 19.Stall RD, Hays RB, Waldo CR, Ekstrand M, McFarland W. The gay '90s: A review of research in the 1990s on sexual behavior and HIV risk among men who have sex with men. AIDS. 2000;14(Suppl 3):S101–14. [PubMed] [Google Scholar]
- 20.Torian LV, Makki HA, Menzies IB, Murrill CS, Weisfuse IB. HIV infection in men who have sex with men, New York City Department of Health sexually transmitted disease clinics, 1990–1999: a decade of surveillance finds that racial disparities and associations between HIV and gonorrhea persist. Sex Transm Dis. 2002;29:73–8. doi: 10.1097/00007435-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 21.MacKellar DA, Valleroy LA, Secura GM, Behel S, Bingham T, Celentano DD, et al. Unrecognized HIV infection, risk behaviors, and perceptions of risk among young men who have sex with men: opportunities for advancing HIV prevention in the third decade of HIV/AIDS. J Acquir Immune Defic Syndr. 2005;38:603–14. doi: 10.1097/01.qai.0000141481.48348.7e. [DOI] [PubMed] [Google Scholar]
- 22.Ruiz JD, Ritieni A, Facer M, Nunez A, Ginsberg M, Molitor F. HIV infection and related risk behaviors among Latino MSM in the Tijuana-San Diego border region [Abstract M1-B1603]. Proceedings of the 2003 National HIV Prevention Conference; 2003 Jul 27–30; Atlanta, GA. [Google Scholar]
- 23.Stall R, Barrett D, Bye L, Catania J, Frutchey C, Henne J, et al. A comparison of younger and older gay men's HIV risk taking behaviors: the Communication Technologies 1989 Cross-Sectional Survey. J Acquir Immune Defic Syndr. 1992;5:682–7. [PubMed] [Google Scholar]
- 24.Osmond D, Page K, Wiley J, Garrett K, Sheppard HW, Moss AR, et al. HIV infection in homosexual and bisexual men 18 to 29 years of age: the San Francisco Young Men's Health Study. Am J Public Health. 1994;84:1933–7. doi: 10.2105/ajph.84.12.1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.MacKellar D, Valleroy L, Karon G, Lemp G, Janssen R. The Young Men's Survey: methods for estimating HIV seroprevalence and risk factors among men who have sex with men. Public Health Rep. 1996;111(Suppl 1):138–44. [PMC free article] [PubMed] [Google Scholar]
- 26.Muhib F, Lin L, Stueve A, Miller RL, Ford WL, Johnson WD, et al. A venue-based method for sampling hard-to-reach populations. Public Health Rep. 2001;116(Suppl 1):216–22. doi: 10.1093/phr/116.S1.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stueve A, O'Donnell LN, Duran R, San Doval A, Blome J. Time-space sampling in minority communities: results with young Latino men who have sex with men. Am J Public Health. 2001;91:922–6. doi: 10.2105/ajph.91.6.922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kalton G. Sampling flows of mobile human populations. Surv Methodol. 1991;17:183–9. [Google Scholar]
- 29.Stueve A. O'Donnell L, Duran R, San Doval A, Geier J. Being high and taking sexual risks: findings from a multisite survey of urban men who have sex with men. AIDS Educ Prev. 2002;14:482–95. doi: 10.1521/aeap.14.8.482.24108. [DOI] [PubMed] [Google Scholar]
- 30.Peterson JL, Bakeman R, Stokes J Community Intervention Trial for Youth Study Team. Racial/ethnic patterns of HIV sexual risk behaviors among young men who have sex with men. J Gay Lesbian Med Assoc. 2001;5:155–62. [Google Scholar]
- 31.Choi KH, McFarland W, Neilands TB, Nguyen S, Louie B, Secura GM, et al. An opportunity for prevention. Prevalence, incidence, and sexual risk for HIV among young Asian and Pacific Islander men who have sex with men, San Francisco. Sex Transm Dis. 2004;31:475–80. doi: 10.1097/01.olq.0000135988.19969.62. [DOI] [PubMed] [Google Scholar]
- 32.Gallagher KM, Sullivan PS, Lansky A, Onorato IM. Behavioral surveillance among people at risk for HIV infection in the U.S.: the National HIV Behavioral Surveillance System. Public Health Rep. 2007;122(Suppl 1):32–8. doi: 10.1177/00333549071220S106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.CDC (US). HIV prevalence, unrecognized infection, and HIV testing among men who have sex with men—five U.S. cities, June 2004–April 2005. MMWR Morb Mortal Wkly Rep. 2005;54(24):597–601. [PubMed] [Google Scholar]
- 34.McFarlane M, Bull SS, Rietmeijer CA. The Internet as a newly emerging risk environment for sexually transmitted diseases. JAMA. 2000;284:443–6. doi: 10.1001/jama.284.4.443. [DOI] [PubMed] [Google Scholar]
- 35.Kim AA, Kent C, McFarland W, Klausner JD. Cruising on the Internet highway. J Acquir Immune Defic Syndr. 2001;28:89–93. doi: 10.1097/00042560-200109010-00013. [DOI] [PubMed] [Google Scholar]
- 36.Taylor M, Aynalem G, Smith L, Bemis C, Kenney K, Kerndt P. Correlates of Internet use to meet sex partners among men who have sex with men diagnosed with early syphilis in Los Angeles County. Sex Transm Dis. 2004;31:552–6. doi: 10.1097/01.olq.0000137902.71284.b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Department of Health and Human Services (US). Evaluation of web-based HIV risk behavior surveillance among men who have sex with men; notice of availability of funds. Federal Register. 2003;68:34391–4. [Google Scholar]
- 38.Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations. Social Problems. 1997;44:174–99. [Google Scholar]
- 39.Heckathorn DD, Semaan S, Broadhead RS, Hughes JJ. Extensions of respondent-driven sampling: a new approach to the study of injection drug users aged 18-25. AIDS and Behavior. 2002;6:55–67. [Google Scholar]
- 40.Valdiserri RO, Aultman TV, Curran JW. Community planning: a national strategy to improve HIV prevention programs. J Community Health. 1995;20:87–100. doi: 10.1007/BF02260331. [DOI] [PubMed] [Google Scholar]