SYNOPSIS
This article describes a conceptual framework for HIV behavioral surveillance in the United States. The framework includes types of behaviors to monitor, such as risk behaviors, HIV testing behaviors, adherence to HIV treatment, and care-seeking for HIV/AIDS. The framework also describes the population groups in which specific behaviors should be monitored. Because the framework is multifaceted in terms of behaviors and populations, behavioral data from multiple surveillance systems are integrated to achieve HIV behavioral surveillance program objectives. Defining surveillance activities more broadly to include behavioral surveillance in multiple populations will provide more comprehensive data for prevention planning, and lead to a more effective response to HIV/AIDS in the United States.
Through 2003, more than 900,000 people had been reported as having AIDS in the United States.1 The Centers for Disease Control and Prevention (CDC) estimates that the number of new HIV infections per year is approximately 40,000.2 As part of its strategic plan to control the spread of HIV during the epidemic's third decade, CDC has established the overarching goal of reducing new HIV infections in the United States by 50%. To achieve this objective, four specific goals were identified, one of which is to strengthen the national capacity to monitor the HIV epidemic to better direct and evaluate prevention efforts.3
Public health surveillance has been described as the “cornerstone of a country's HIV response.”4 Surveillance of HIV infection in 33 areas with integrated HIV/AIDS surveillance systems highlights that racial/ethnic minorities are disproportionately affected and that marked increases in HIV have occurred among women, young men who have sex with men (MSM), and people infected through heterosexual contact.1 Monitoring the characteristics of these affected populations for HIV prevention and control purposes requires the collection of behavioral data.
In this article, we describe a conceptual framework for HIV behavioral surveillance in the United States, in which behavioral surveillance is an integral part of HIV/AIDS surveillance. First, we define behavioral surveillance and its relationship to disease surveillance. Then, we identify categories of behaviors that are important to monitor in relation to HIV transmission, acquisition, and disease progression, as well as the populations in which those behaviors should be observed. Next, we describe the individual surveillance systems that, taken together, comprise CDC's HIV behavioral surveillance program based on the conceptual framework. Finally, as surveillance is “information for action,” we describe uses of behavioral surveillance data for epidemiologic, program evaluation, and public health intervention functions.
DEFINITION OF BEHAVIORAL SURVEILLANCE
Behavioral surveillance, for public health purposes, is the systematic and ongoing collection of data about risk and health-related behaviors with the purpose of correlating trends in behaviors with changes in disease over time. Behavioral data provide a way to monitor short-term changes in epidemics without having to wait for changes in disease outcomes.5 Surveillance of behaviors that are risk factors for infection or disease is an important public health activity.6 With conditions such as HIV infection, exposure and manifestation of the infection may be years apart. By measuring risk behaviors that are more proximate to the time of HIV infection, it is possible to identify and respond to trends in behaviors that anticipate trends in acquisition and transmission of HIV infection, which in turn would only be reflected years later in HIV/AIDS case report data. Similarly, surveillance of HIV testing and care-seeking behaviors is important because the timing of testing and treatment is related to the time to development of frank disease (i.e., AIDS-defining conditions), and diagnosis and care-seeking can also occur years apart.
Initially, behavioral data from case investigations and surveillance (i.e., exposure risk data) elucidated the ways in which HIV is transmitted and the populations most at risk. Historically, behavioral surveillance data have also been used to help understand and explain changes in HIV and AIDS incidence and prevalence, particularly at the local level.7–11 Increasingly, behavioral surveillance data are instrumental in designing and evaluating prevention interventions and in integrating prevention and treatment services for HIV-infected individuals.12 Comparisons can be made of relevant behavioral trends (from behavioral surveillance data) and clinical trends (from case surveillance data). For example, prevalence of and trends in adherence among HIV-infected people may be assessed to determine the extent to which concurrent changes in AIDS incidence are occurring.13 In an example from outside the U.S., ongoing behavioral surveys allowed researchers to attribute declining HIV prevalence in Uganda to deaths rather than to changes in behavior and associated reductions in new infections; in fact, the behavioral data indicated increases in risky behavior among adolescents.14
CONCEPTUAL FRAMEWORK OF THE KEY BEHAVIORS AND POPULATIONS FOR HIV BEHAVIORAL SURVEILLANCE
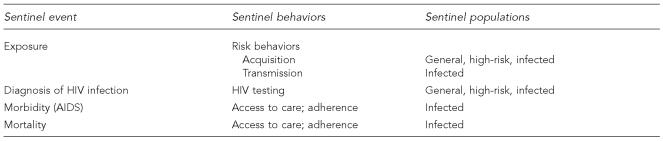
The conceptual framework for HIV behavioral surveillance in the U.S. includes four major “sentinel events” in the life cycle of HIV infection, and four corresponding behavioral components. The sentinel events are exposure to HIV, infection with HIV, development of clinical disease (morbidity), and death (mortality). The four corresponding behaviors are risk behaviors, HIV testing, access to care, and acceptance of and adherence to therapy for HIV infection (Figure 1).
Figure 1.
Sentinel surveillance events, behaviors, and populations that comprise HIV behavioral surveillance in the United States
Since the virtual elimination of transfusion/blood products-associated HIV transmission, and due to substantial progress toward eliminating mother-to-child transmission, virtually all HIV infections in the U.S. are accounted for by transmission from infected individuals to their sex or drug-using partners via male/male sex, injection drug use, and heterosexual sex. Thus, HIV behavioral surveillance can be limited to measurement of sexual and drug-using risks in order to monitor acquisition and transmission of infection.
HIV testing is a key part of HIV prevention activities, as it is required to diagnose an HIV infection. Based on the results of HIV testing, serostatus-specific interventions can be delivered as appropriate to reduce acquisition and transmission of the virus.2 To monitor the epidemic, it is important to know why, when, and where people test or, conversely, why individuals do not seek an HIV test or refuse one if it is offered. Among those tested by conventional methods (i.e., not by rapid tests), it is also important to know whether people return for their results after they are tested. With advances in test technologies, it is also of interest to know how individuals are being tested (e.g., rapid vs. conventional tests).
Certain critical behaviors that relate to treatment of HIV infection include access to and seeking care, accepting recommended therapy, and adhering to prescribed therapy. With the advent of highly active antiretroviral therapy (HAART), it is important that HIV-infected individuals are treated early and adhere to their medication regimens. The benefits of treatment can occur at the individual level through reduced viral load, which slows disease progression, and at the population level, where increasing the proportion of positive individuals with low viral load will reduce mortality and may reduce rates of transmission.15,16 Understanding patterns of acceptance of and adherence to therapy allows a context in which to interpret trends in new AIDS diagnoses and AIDS-related deaths.
The conceptual framework next incorporates populations in which to monitor these behaviors (Figure 1): general, high-risk, and infected populations. Data collected from the general population can be used to determine whether the epidemic is likely to become more generalized (similar to African countries) or remain concentrated in certain high-risk groups (as in the United States). These changes are best monitored through representative sampling of the general U.S. population to measure risk behaviors and HIV-testing behaviors.17,18
Behavioral surveillance also must include the collection of data from infected populations and populations at increased risk for infection. Populations at increased risk for acquiring HIV infection in the United States include MSM, injecting drug users (IDUs), and high-risk heterosexuals who engage in risky behaviors or have HIV-infected partners (HET). Behavioral surveillance data from these high-risk groups provide information from those likely to have the biggest impact on the epidemic's future course.4 In this group, it is necessary to monitor acquisition risk behaviors and HIV testing.
In case-reporting surveillance systems, data are generally collected from people who are infected. It is important to collect behavioral information on how individuals were infected (i.e., acquisition behaviors) and how their ongoing risks may transmit the virus to others. In addition, information about access to and use of HIV-related services and treatment is needed to improve linkage into appropriate care and treatment.
Data on each behavior (risk, testing, care-seeking, adherence) from each relevant population (general, high-risk, and infected) provide part of the overall behavioral surveillance program. Together, these components comprise the HIV behavioral surveillance conceptual framework.
This conceptual model for the U.S. shares many elements of the World Health Organization (WHO)/Joint United Nations Programme on HIV/AIDS (UNAIDS) “second-generation surveillance,”19,20 but furthers that model in several important ways. Second-generation surveillance utilizes national, population-based surveys such as demographic and health surveys; it also recommends some type of surveillance activity for high-risk populations. Similarly, the approach for the U.S. utilizes data from nationwide, repeated, population-based surveys, and calls for repeated cross-sectional surveys among individuals in defined high-risk groups and geographic areas. However, the U.S. model furthers the second-generation surveillance model in that high-quality HIV and AIDS case-surveillance data are available in the U.S. These data allow the U.S. behavioral surveillance model to include all three populations (general, high-risk, and infected) in which understanding acquisition and transmission dynamics is necessary to advance HIV prevention and control.
HIV BEHAVIORAL SURVEILLANCE SYSTEMS
The conceptual framework for HIV behavioral surveillance identifies which behaviors to monitor and in which populations. To move from the conceptual model to an operating model, existing surveillance systems must be augmented and new surveillance systems developed and deployed to collect relevant behavioral information from the three defined populations.
To understand which systems are included in the overall program of HIV behavioral surveillance, it is important to distinguish between one-time behavioral surveys and behavioral surveillance. As previously noted, behavioral surveillance is ongoing and systematic; that is, data must be collected with some sustainable frequency using the same or similar methods and instruments over time to analyze trends. While many behavioral surveys collect important information from one or more of the three population groups that comprise the framework, this survey focuses on systems that meet the surveillance definition.
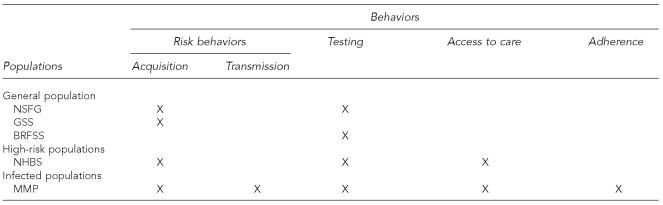
The design and implementation of behavioral surveillance systems in the United States require a variety of approaches to accommodate state and local data needs, different surveillance infrastructures, and limited resources. Rather than try to develop a single behavioral surveillance system to reach all three populations and measure all four behaviors, the Division of HIV/AIDS Prevention at CDC supports multiple surveillance systems that have a behavioral component related to monitoring HIV/AIDS. These systems are shown in Figure 2. More detailed descriptions of some of these systems can be found in other articles within this special issue.21,22
Figure 2.
HIV behavioral surveillance systems: populations and behavioral measures
NSFG = National Survey of Family Growth
GSS = General Social Survey
BRFSS = Behavioral Risk Factor Surveillance System
NHBS = National HIV Behavioral Surveillance System
MMP = Medical Monitoring Project
General population
Within the general population component of HIV behavioral surveillance, data from a number of systems are used to obtain a more complete picture of acquisition risk behaviors and HIV testing patterns in the U.S. population. In addition, multiple systems are needed because of the differences in populations included on the sampling frames, limitations on the overall number of questions per survey, the types of questions (sex, drug use, testing) included in each survey, and the frequency of data collection. Three systems are described here that have provided general population HIV behavioral surveillance data for many years and have a specific collaboration with the Division of HIV/AIDS Prevention at CDC: the National Survey of Family Growth, the Behavioral Risk Factor Surveillance System, and the General Social Survey.
National Survey of Family Growth (NSFG).
NSFG has been conducted periodically since 1973, but plans to move to continuous data collection in 2006.23 It is a nationally representative sample of women aged 15–44; men were added to the NSFG sample in 2002. Primarily a reproductive health survey, NSFG provides detailed sexual behavior questions, including condom and contraceptive use.24 NSFG also collects limited information on injection drug use and HIV testing.25
Behavioral Risk Factor Surveillance System (BRFSS).
In 1984, CDC established BRFSS to monitor state-level prevalence of the major behavioral risks associated with premature morbidity and mortality among adults.26 By 1994, all states, the District of Columbia, and three territories were participating in the BRFSS. Data from BRFSS are available annually. Beginning in 1991, HIV-related questions, mainly focused on HIV testing behaviors, have been included on BRFSS.27
General Social Survey (GSS).
GSS has been conducted about every two years since 1972 and is a nationally representative sample based off the U.S. Census. As the name implies, the purpose of GSS is to monitor trends in the structure and functioning of American society.28 Since 1988, GSS has collected data on sexual behavior and more recently added questions on crack cocaine use.29 HIV testing questions have been proposed for the 2006 survey.
High-risk populations
An internal review of HIV behavioral surveillance activities at CDC, conducted in 2001, recommended that a surveillance system focusing on high-risk populations be developed (“Recommendations for Behavioral and Prevention Services Surveillance in NCHSTP,” CDC unpublished report, 2001 Jul 17). While numerous behavioral surveys of various high-risk populations had been conducted in selected geographic areas over the years,30,31 there was not a system offering ongoing and systematic data that represented a large proportion of the epidemic. In addition, the HIV Prevention Strategic Plan had a significant focus on monitoring the epidemic.3 These factors and others led to the development of a large-scale behavioral surveillance system focusing on individuals at high risk for infection.
The National HIV Behavioral Surveillance System (NHBS) is a comprehensive system for conducting behavioral surveillance among people at highest risk for HIV infection in the U.S.22 The overall strategy for NHBS includes conducting rotating 12-month cycles of surveillance in three populations at high risk for HIV: MSM recruited from venues such as bars, clubs, and public places using time-space sampling;32,34 IDUs recruited through respondent-driven sampling (a peer-referral method);35,36 and HET for which the sampling method has yet to be determined. Data collection began with the first MSM cycle in 2003–200437 and the first IDU cycle in 2005;38 surveillance will be conducted over time with these three groups in 25 participating metropolitan statistical areas that were chosen based on high AIDS rates.
Infected populations
As an adjunct to HIV/AIDS case surveillance, a longitudinal supplemental surveillance study, the Adolescent/Adult Spectrum of Disease (ASD), was launched in 1990 to better determine the natural history and spectrum of disease and, later, the impact of HAART on disease progression, by reviewing medical records over time.39 In addition, an interview study with infected individuals, the Supplement to HIV/AIDS Surveillance, was conducted to collect detailed behavioral data.40 These supplemental surveillance data allowed further description of how the epidemic was changing in terms of who was getting infected and how. They were also useful for the planning and evaluation of prevention and treatment services.9 However, these studies were conducted in a limited number of states and had varied sampling methods. The Medical Monitoring Project (MMP) was designed to improve on the sampling design of previous studies and combine the interview and record review for individuals.41
MMP employs a three-stage, stratified, clustered sampling design resulting in annual cross-sectional probability samples of adults in care for HIV disease. Collection of data from interviews with HIV-infected patients provides information on the prevalence of behaviors that facilitate HIV transmission (sexual behavior, injection drug use); patients' access to, use of, and barriers to HIV-related secondary prevention services; utilization of HIV-related medical services; and adherence to drug regimens. By combining these interview data with data collected from the abstraction of medical records, MMP will provide information on clinical conditions that occur in HIV-infected people as a result of their disease or the medications they take, as well as the type and quality of HIV care and support services these patients receive.
USES OF BEHAVIORAL SURVEILLANCE DATA
The systems that make up the HIV behavioral surveillance program, guided by the conceptual framework, provide data for monitoring the epidemic. In addition, behavioral surveillance data can be used to evaluate case surveillance systems and HIV testing strategies, and to develop and evaluate prevention programs and HIV-related care services.
Behavioral data can be used for evaluating the representativeness of case surveillance systems. For example, data collected through behavioral surveillance can be compared to HIV case surveillance systems, which include only people who present for HIV testing. Comparing the characteristics of those at high risk who have not been tested with those included in the HIV case surveillance system who have been tested can indicate who may be missed in surveillance because they were not tested and diagnosed. Such a comparison might be a more timely reflection of current trends in the epidemic than looking at concurrent HIV and AIDS diagnoses—another method of monitoring missed opportunities for testing. Further, interpretation of trends in HIV surveillance data is predicated on the assumption that underlying patterns of HIV testing are stable. An increase in new HIV diagnoses may represent an actual increase in new HIV infections, or may be an artifact of increased HIV testing among high-risk individuals. By monitoring HIV testing behaviors among those at high risk, the assumption of stable HIV testing patterns can be validated—or refuted.42
Similarly, information on care-seeking collected through behavioral surveillance may help determine the extent to which new cases of HIV and AIDS are related to access to and utilization of testing and care.42 Case surveillance and behavioral surveillance data from infected people have demonstrated that the most common reason for getting an HIV test was illness.43,44 That information, in turn, can be used to address barriers to testing, such as broadening the reach of messages about the need for routine testing among those at highest risk, improving access to testing services, or developing new testing technologies.
The development of the rapid HIV test creates new opportunities for expanding HIV testing. The Advancing HIV Prevention (AHP) initiative from CDC promotes testing as a routine part of medical care and will implement new models for HIV testing—including the use of the rapid HIV test—in nontraditional settings, particularly nonmedical ones, such as in correctional facilities.45 HIV testing data from behavioral surveillance systems can be used to evaluate the implementation of the strategies that comprise AHP, such as by collecting information on the type of tests used and whether tests were offered at routine medical visits or during prenatal care. A precedent exists for using behavioral surveillance data to conduct this type of assessment of policies and guidelines: data from BRFSS on HIV testing behaviors were used to evaluate the implementation of the 1995 guidelines on counseling and testing pregnant women.46
Behavioral surveillance data are also extremely useful for developing and delivering prevention programs—identifying demographic characteristics of those at high risk and what behaviors put them at risk to then focus prevention efforts toward specific groups and their behaviors. Although the sex and drug-use behaviors that are associated with risk of HIV infection are well known, that information alone is not enough to efficiently target prevention efforts. To design the most effective interventions, additional behavioral data are needed to differentiate among risky behaviors. For example, early in the epidemic, documenting that male/male sex as a risk was important to understand transmission, but further understanding the risk of receptive anal sex (vs. other types of sex with men) allowed for more specific prevention messages and programs to be developed and delivered. In addition, behavioral surveillance data can be used to design prevention programs for people who are HIV positive, to prevent further transmission of the virus.2
Understanding the reasons for lack of acceptance of therapy or nonadherence may suggest strategies for improved secondary prevention services for those living with HIV infection (i.e., to prevent progression of HIV). For example, data from behavioral surveillance may identify behavioral or structural barriers to treatment that could be addressed by appropriate interventions. Ultimately, behavioral surveillance data from MMP will produce data about met and unmet needs for HIV care and prevention services, which can be used to evaluate these services and to direct future resources for HIV-infected patients.41
Given that behavioral surveillance data can be used to guide the design, delivery, and evaluation of prevention and care services, it is logical that such data can also be used to target distribution of funds for prevention and care services. Making decisions based on this data can help ensure an equitable distribution of funds. CDC and the Health Resources and Services Administration (HRSA) jointly support the use of supplemental behavioral and clinical surveillance data through the integration of program planning, evaluation, and resource allocation in the prevention planning and Ryan White planning processes at the community level.9
CONCLUSION
The conceptual framework for HIV behavioral surveillance provided in this article describes which behaviors should be monitored and in which population groups. The ongoing, systematic, representative, and geographically diverse collection of behavioral data via NHBS, MMP, and general population surveys presents a blueprint for integrating behavioral surveillance with clinical and case surveillance (Figure 1) and makes for a stronger “cornerstone” of the response to HIV/AIDS in the United States.
REFERENCES
- 1.Centers for Disease Control and Prevention (US) Atlanta: Department of Health and Human Services (US); 2004. HIV/AIDS surveillance report, 2003 (vol. 15) pp. 1–46. [Google Scholar]
- 2.Janssen RS, Holtgrave DR, Valdiserri RO, Shepherd M, Gayle HD, DeCock KM. The serostatus approach to fighting the HIV epidemic: prevention strategies for infected individuals. Am J Public Health. 2001;91:1019–24. doi: 10.2105/ajph.91.7.1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CDC (US) HIV Prevention Strategic Plan through 2005. [cited 2005 Mar 19]; Available from: URL: http://www.cdc.gov/hiv/partners/psp.htm.
- 4.Mills S, Saidel T, Magnani R, Brown T. Surveillance and modelling of HIV, STI, and risk behaviours in concentrated HIV epidemics. Sex Transm Infect. 2004;80:ii57–62. doi: 10.1136/sti.2004.011916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pisani E, Brown T, Saidel T, Rehle T, Carael M. Meeting the behavioural data collection needs of national HIV/AIDS and STD programmes. UNAIDS. 1998 [Google Scholar]
- 6.Morabia A. From disease surveillance to the surveillance of risk factors. Am J Public Health. 1996;86:625–7. doi: 10.2105/ajph.86.5.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wohl AR, Johnson DF, Lu S, Frye D, Bunch G, Simon PA. Recent increase in high-risk sexual behaviors among sexually active men who have sex with men living with AIDS in Los Angeles County. J Acquir Immune Defic Syndr. 2004;35:209–11. doi: 10.1097/00126334-200402010-00019. [DOI] [PubMed] [Google Scholar]
- 8.Lansky A, Nakashima AK, Diaz T, Fann SA, Conti L, Herr M, et al. Human immunodeficiency virus infection in rural areas and small cities of the southeast: contributions of migration and behavior. J Rural Health. 2000;16:20–30. doi: 10.1111/j.1748-0361.2000.tb00433.x. [DOI] [PubMed] [Google Scholar]
- 9.Whitmore SK, Zaidi IF, Dean HD. The integrated epidemiologic profile: using multiple data sources in developing profiles to inform HIV prevention and care planning. AIDS Educ Prev. 2005;17(Suppl B):3–16. doi: 10.1521/aeap.2005.17.Supplement_B.3. [DOI] [PubMed] [Google Scholar]
- 10.CDC (US) Adoption of protective behaviors among persons with recent HIV infection and diagnosis—Alabama, New Jersey,and Tennessee, 1997–1998. MMWR Morb Mortal Wkly Rep. 2000;49(23):512–5. [PubMed] [Google Scholar]
- 11.Sorvillo F, Kerndt P, Odem S, Castillon M, Carruth A, Contreras R. Use of protease inhibitors among persons with AIDS in Los Angeles County. AIDS Care. 1999;11:147–55. doi: 10.1080/09540129948045. [DOI] [PubMed] [Google Scholar]
- 12.Rugg DL, Heitgerd JL, Cotton DA, Broyles S, Freeman A, Lopez-Gomez AM, et al. CDC HIV prevention indicators: monitoring and evaluating HIV prevention in the USA. AIDS. 2000;14:2003–13. doi: 10.1097/00002030-200009080-00017. [DOI] [PubMed] [Google Scholar]
- 13.Sullivan PS, Nakamura GV, Campsmith MS. Surveillance for adherence to antiretroviral therapies and associated factors: results from a multistate interview project in the US. XIV International AIDS Conference; 2002 Feb 22–25; Boston, MA. [Google Scholar]
- 14.Wawer M, Gray R, Serwadda D, Namukwaya Z, Makumbi F, Sewankambo N, et al. Declines in HIV prevalence in Uganda: not as simple as ABC. 12th Conference on Retroviruses and Opportunistic Infections; 2005 Feb 22–25; Boston, MA. [Google Scholar]
- 15.Wawer MJ, Gray RH, Sweankambo NK, Serwadda D, Li X, Laeyendecker O, et al. Rates of HIV-1 transmission per coital act, by stage of HIV-1 infection, in Rakai, Uganda. J Infect Dis. 2005;191:1403–9. doi: 10.1086/429411. [DOI] [PubMed] [Google Scholar]
- 16.Gray RH, Wawer MJ, Brookmeyer R, Sewankambo NK, Serwadda D, Wabwire-Mangen F, et al. Probability of HIV-1 transmission per coital act in monogamous, heterosexual, HIV-1 discordant couples in Rakai, Uganda. Lancet. 2001;357:1149–53. doi: 10.1016/S0140-6736(00)04331-2. [DOI] [PubMed] [Google Scholar]
- 17.Holtzman D, Bland S, Lansky A, Mack KA. HIV-related behaviors and perceptions among adults in 25 states: 1997 BRFSS. Am J Public Health. 2001;91:1882–8. doi: 10.2105/ajph.91.11.1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.CDC (US) Number of persons tested for HIV—United States 2002. MMWR Morb Mort Weekly Rep. 2004;53(47):1110–3. [PubMed] [Google Scholar]
- 19.World Health Organization. Guidelines for second-generation HIV surveillance: the next decade. [cited 2006 Sep 6];2000 Available from: URL: http://www.who.int/hiv/pub/epidemiology/pub3/en. [PubMed]
- 20.Rehle T, Lazzari S, Dallabetta G, Asamoah-Odei E. Second- generation HIV surveillance: better data for decision-making. Bull World Health Organ. 2004;82:121–7. [PMC free article] [PubMed] [Google Scholar]
- 21.Lansky A, Drake AJ, DiNenno E, Lee CW. HIV behavioral surveillance among the U.S. general population. Public Health Rep. 2007;122(Suppl 1):24–31. doi: 10.1177/00333549071220S105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gallagher KM, Sullivan PS, Lansky A, Onorato IM. Behavioral surveillance among people at risk for HIV infection in the U.S.: the National HIV Behavioral Surveillance System. Public Health Rep. 2007;122(Suppl 1):32–8. doi: 10.1177/00333549071220S106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Center for Health Statistics (US) National Survey of Family Growth online documents. [cited 2006 Sep 6]; Available from: URL: http://www.cdc.gov/nchs/nsfg.htm.
- 24.Anderson JE, Chandra A, Mosher WD. HIV testing in the United States, 2002. Natl Vital Stat Rep. 2005 Nov 8;363:1–32. [PubMed] [Google Scholar]
- 25.Mosher W, Chandra A, Jones J. Sexual behavior and selected health measures: men and women 15–44 years of age, United States, 2002. Natl Vital Stat Rep. 2005 Sep 15;362:1–55. [PubMed] [Google Scholar]
- 26.CDC (US) Behavioral Risk Factor Surveillance System. [cited 2006 Sep 6]; Available from: URL: http://www.cdc.gov/brfss.
- 27.Ebrahim SH, Anderson JE, Weidle P, Purcell DW. Race/ethnic disparities in HIV testing and knowledge about treatment for HIV/AIDS: United States, 2001. AIDS Patient Care STDS. 2004;18:27–33. doi: 10.1089/108729104322740893. [DOI] [PubMed] [Google Scholar]
- 28.National Opinion Research Center at the University of Chicago (US) General Social Survey: GSS study description. [cited 2006 Sep 6]; Available from: URL: http://www.norc.uchicago.edu/projects/gensoc1.asp.
- 29.Anderson JE. Condom use and HIV risk among US adults. Am J Public Health. 2003;93:912–4. doi: 10.2105/ajph.93.6.912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Valleroy LA, MacKellar DA, Karon JM, Rosen DH, McFarland W, Shehan DA, et al. HIV prevalence and associated risks in young men who have sex with men. JAMA. 2000;284:198–204. doi: 10.1001/jama.284.2.198. [DOI] [PubMed] [Google Scholar]
- 31.Kellerman SE, Lehman SJ, Lansky A, Stevens MR, Hecht FM, Bindman AB, et al. HIV testing within at-risk populations in the United States and the reasons for seeking or avoiding HIV testing. J Acquir Immune Defic Syndr. 2002;31:202–10. doi: 10.1097/00126334-200210010-00011. [DOI] [PubMed] [Google Scholar]
- 32.MacKellar D, Valleroy L, Karon J, Lemp G, Janssen R. The young men's survey: methods for estimating HIV seroprevalence and risk factors among young men who have sex with men. Public Health Rep. 1996;111(Suppl 1):138–44. [PMC free article] [PubMed] [Google Scholar]
- 33.Muhib FB, Lin LS, Stueve A, Miller RL, Ford WL, Johnson WD, et al. A venue-based method for sampling hard-to-reach populations. Public Health Rep. 2001;116(Suppl 1):216–22. doi: 10.1093/phr/116.S1.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stueve A, O'Donnell LN, Duran R, Doval A, Blome J. Time-space sampling in minority communities: results with young Latino men who have sex with men. Am J Public Health. 2001;91:922–6. doi: 10.2105/ajph.91.6.922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations. Social Problems. 1997;44:174–99. [Google Scholar]
- 36.Heckathorn DD. Respondent-driven sampling II: deriving valid population estimates from chain-referral samples of hidden populations. Social Problems. 2002;49:11–34. [Google Scholar]
- 37.MacKellar D, Gallagher KM, Finlayson TJ, Sanchez TH, Lansky A, Sullivan PS. Surveillance of HIV risk and prevention behaviors of men who have sex with men—a national application of venue-based, time-space sampling. Public Health Rep. 2007;122(Suppl 1):39–47. doi: 10.1177/00333549071220S107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lansky A, Abdul-Quader AS, Cribbin M, Hall T, Finlayson T, Garfein R, et al. Developing an HIV behavioral surveillance system for injecting drug users: the National HIV Behavioral Surveillance System. Public Health Rep. 2007;122(Suppl 1):48–55. doi: 10.1177/00333549071220S108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Farizo KM, Buehler JW, Chamberland ME, Whyte BM, Froelicher ES, Hopkins SG, et al. Spectrum of disease in persons with human immunodeficiency virus infection in the United States. JAMA. 1992;267:1798–805. [PubMed] [Google Scholar]
- 40.Buehler JW, Diaz T, Hersh BS, Chu SY. The supplement to HIV/AIDS surveillance project: an approach for monitoring HIV risk behaviors. Public Health Rep. 1996;111(Suppl 1):133–7. [PMC free article] [PubMed] [Google Scholar]
- 41.Sullivan PS, Karon JM, Malitz FE, Broyles S, Mokotoff ED, Buskin SE, et al. A two-stage sampling method for clinical surveillance of individuals in care for HIV infection in the United States. Public Health Rep. 2005;120:230–9. doi: 10.1177/003335490512000304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fleming PL, Wortley PM, Karon JM, DeCock KM, Janssen RS. Tracking the HIV epidemic: current issues, future challenges. Am J Public Health. 2000;90:1037–41. doi: 10.2105/ajph.90.7.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wortley PM, Chu SY, Diaz T, Ward JW, Doyle B, Davidson AJ, et al. HIV testing patterns: where, why, and when were persons with AIDS tested for HIV? AIDS. 1995;9:487–92. [PubMed] [Google Scholar]
- 44.CDC (US) Late versus early testing of HIV—16 sites, United States, 2000–2003. MMWR Morb Mortal Wkly Rep. 2003;52(25):581–6. [PubMed] [Google Scholar]
- 45.CDC (US) Advancing HIV prevention: new strategies for a changing epidemic—United States, 2003. MMWR Morb Mortal Wkly Rep. 2003;52(15):329–32. [PubMed] [Google Scholar]
- 46.Lansky A, Jones JL, Frey RL, Lindegren ML. Trends in HIV testing among pregnant women: United States, 1994–1999. Am J Public Health. 2001;91:1291–3. doi: 10.2105/ajph.91.8.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]