Abstract
Background
Severe acute respiratory syndrome (SARS) was introduced into Canada by a visitor to Hong Kong who returned to Toronto on Feb. 23, 2003. Transmission to a family member who was later admitted to a community hospital in Toronto led to a large nosocomial outbreak. In this report we summarize the preliminary results of the epidemiological investigation into the transmission of SARS between 128 cases associated with this hospital outbreak.
Methods
We collected epidemiologic data on 128 probable and suspect cases of SARS associated with the hospital outbreak, including those who became infected in hospital and the next generation of illness arising among their contacts. Incubation periods were calculated based on cases with a single known exposure. Transmission chains from the index family to hospital contacts and within the hospital were mapped. Attack rates were calculated for nurses in 3 hospital wards where transmission occurred.
Results
The cases ranged in age from 21 months to 86 years; 60.2% were female. Seventeen deaths were reported (case-fatality rate 13.3%). Of the identified cases, 36.7% were hospital staff. Other cases were household or social contacts of SARS cases (29.6%), hospital patients (14.1%), visitors (14.1%) or other health care workers (5.5%). Of the 128 cases, 120 (93.8%) had documented contact with a SARS case or with a ward where there was a known SARS case. The remaining 8 cases without documented exposure are believed to have had exposure to an unidentified case and remain under investigation. The attack rates among nurses who worked in the emergency department, intensive care unit and coronary care unit ranged from 10.3% to 60.0%. Based on 42 of the 128 cases with a single known contact with a SARS case, the mean incubation period was 5 days (range 2 to 10 days).
Interpretation
Evidence to date suggests that SARS is a severe respiratory illness spread mainly by respiratory droplets. There has been no evidence of further transmission within the hospital after the elapse of 2 full incubation periods (20 days).
Through the swiftness of air travel, severe acute respiratory syndrome (SARS) rapidly migrated from its origins in Guangdong Province, China, in November 2002 to many corners of the world, including Canada in February 2003.1 This syndrome, characterized by fever, headache, myalgia, cough and shortness of breath, leads to pneumonia and occasionally to acute respiratory distress syndrome and death. There is strong evidence that SARS is caused by a novel coronavirus2,3,4,5 spread mainly through respiratory droplets.
As of July 10, 2003, a total of 438 cases of SARS (250 probable and 188 suspect) were reported in Canada, 375 (85.6%) of which occurred in Ontario.
The index case of SARS in Canada was an elderly woman who returned to Toronto on Feb. 23, 2003, after a visit to Hong Kong. She had been exposed to SARS during her stay at a hotel in Kowloon, where a cluster of 13 cases of SARS was subsequently reported.6 She became ill upon her return to Toronto, and the infection spread to family members, one of whom was later admitted to the emergency department of a local hospital, where a large nosocomial outbreak occurred. In this paper we describe the preliminary results of the epidemiological investigation of the initial 128 cases of SARS associated with this outbreak, including those who became infected in the hospital and the next generation of illness among their contacts.
Methods
Cases were classified as either probable or suspect SARS based on the case definition issued by Health Canada.7 Suspect cases were defined as people presenting with fever (temperature greater than 38°C) and 1 or more respiratory symptoms, including cough, shortness of breath or difficulty breathing. Suspect cases also had to have travelled, within 10 days before symptom onset, to a World Health Organization (WHO) reported affected area in Asia, to have visited a defined setting that was associated with a cluster of SARS cases or to have had close contact with a suspect or probable case. Probable cases were defined as people meeting the suspect case definition and having severe progressive respiratory illness suggestive of atypical pneumonia or acute respiratory distress syndrome with no known cause. Close contacts of cases were defined as people who cared for, lived with or had face-to-face (within 1 m) contact with a person with SARS or had direct contact with respiratory secretions or body fluids, or both, of a person with SARS.7
The hospital where the nosocomial outbreak occurred (index hospital) is a 249-bed secondary care community hospital in Toronto. It conducted active surveillance for febrile illness among staff and patients from Mar. 14 to Apr. 15, 2003. Cases of SARS were reported to local public health authorities by clinicians and infection control practitioners. A standard questionnaire was administered to all reported cases or their proxies by health care professionals. Data collected included demographic information, signs and symptoms, onset date of symptoms, and history of recent travel and other potential exposures. Specific exposure dates were obtained through follow-up interviews with cases, review of staff rotations and patient assignments, and review of hospital records.
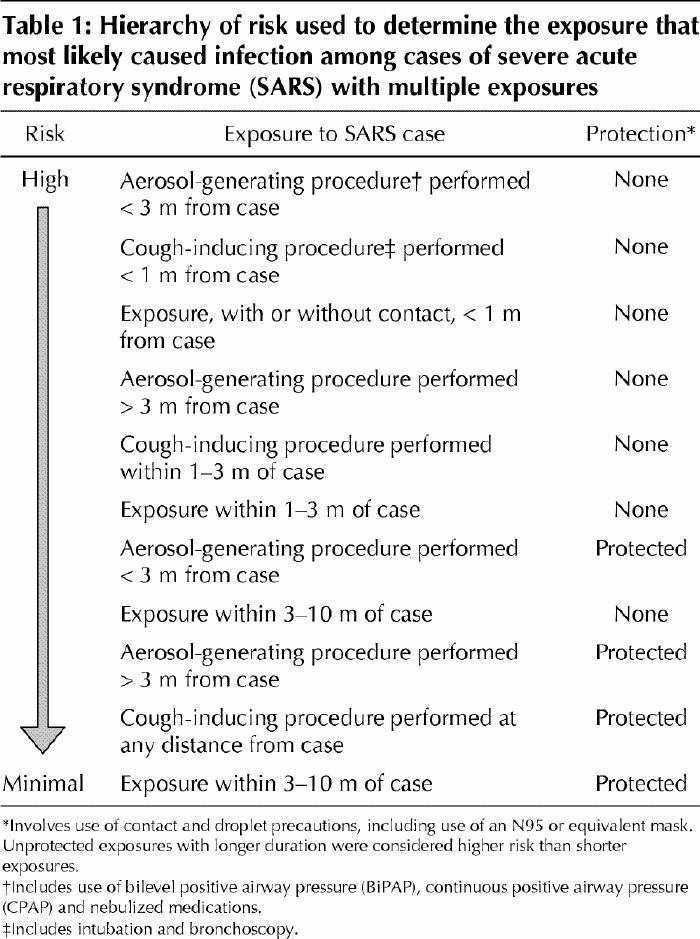
Chains of disease transmission were mapped based on identified exposure history. A hierarchy of risk was developed to determine the most likely exposure that led to infection for people with exposure to more than 1 SARS case (Table 1). The exposure with the highest level of associated risk, based on type, duration and proximity of contact and infection control precautions used, was deemed to be the most likely exposure leading to disease. For cases with multiple exposures, we used the exposure that occurred within 10 days of symptom onset as the most likely exposure based on the incubation periods that had been reported at the time.
Table 1
The incubation period for people with only 1 known exposure was calculated as the number of days between exposure and the date of onset of the first symptom. The case-fatality rate was calculated by dividing the cumulative number of deaths within 60 days after symptom onset by the total number of probable and suspect cases.
Attack rates were calculated for nursing staff on wards in the hospital where at least 1 unrecognized SARS case (i.e., not identified as SARS before transmission from the case) had been admitted. The ward-specific attack rate was calculated by dividing the number of cases among nurses by the total number of nurses who worked during the time a SARS case was on the ward. The number of nurses exposed to a SARS patient was identified through a review of staff rotations. Each nurse was counted only once regardless of the number of shifts worked during the exposure period. Attack rates were also calculated for each ward by the number of nursing hours worked.
All calculations included both probable and suspect cases of SARS associated with the hospital outbreak, including those who acquired infection in the hospital and the next generation of illness arising among their contacts.
Results
Cases
A total of 128 SARS cases (72 probable, 56 suspect) were identified in the outbreak associated with the nosocomial transmission of SARS in the index hospital. Fig. 1 shows the epidemic curve for the outbreak by type of case. The mean age of the cases was 44.8 years (median 42.0 years, range 21 months–86 years); 77 (60.2%) were female. Forty-seven (36.7%) of the cases were hospital staff; patients and visitors accounted for 36 (28.2%) of the cases (Table 2).
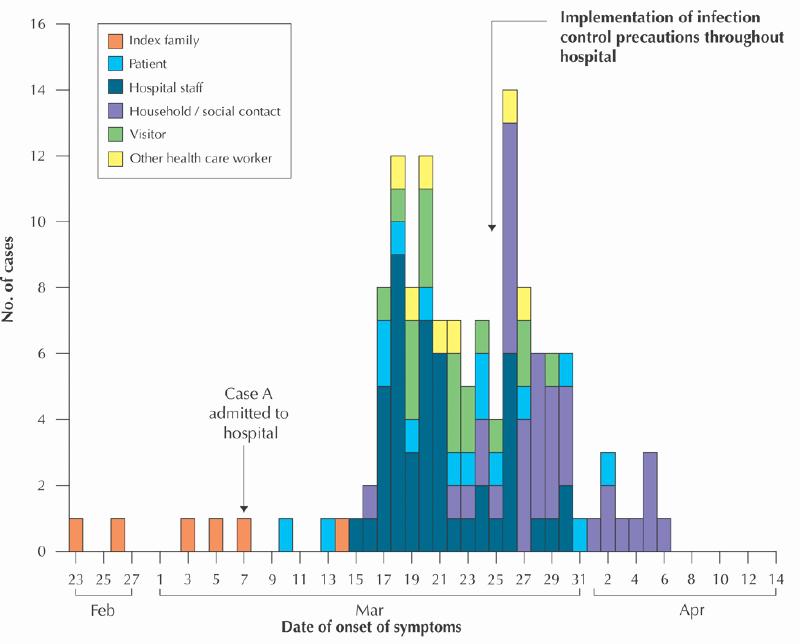
Fig. 1: Reported probable and suspect cases of severe acute respiratory syndrome (SARS) associated with the index case and her family (n = 6) and a nosocomial outbreak at a secondary care community hospital in Toronto (n = 126), by date of onset of symptoms and type of case, from Feb. 23 to Apr. 15, 2003. (Two of the cases in the nosocomial outbreak are not included in this figure because their dates of symptom onset are unknown.)
Table 2

Seven pediatric cases (age less than 18 years) were involved in the outbreak. Four (57.1%) were male. The mean age was 12.8 years (median 17.3 years, range 21 months–17 years). All were household contacts of SARS cases. None required admission to the intensive care unit (ICU), and none died. All 7 cases have been discharged from hospital.
Morbidity and mortality
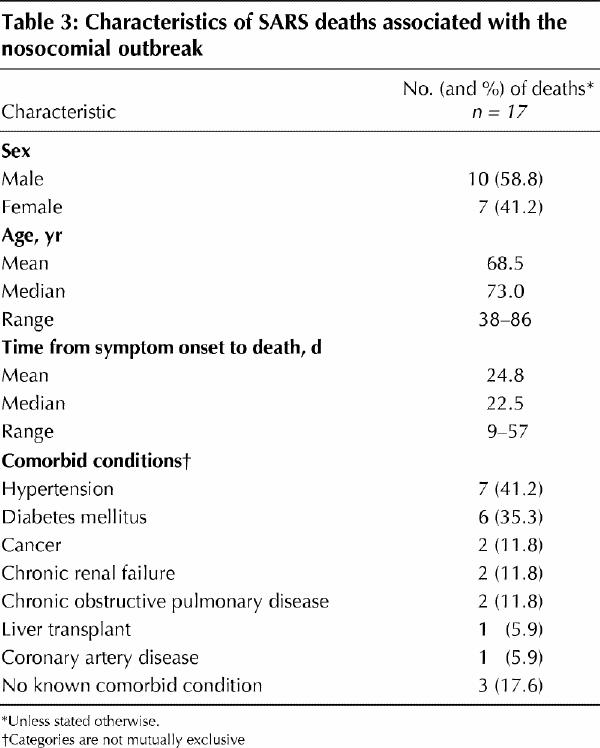
As of July 10, 2003, 17 of the cases had died, for an overall case-fatality rate of 13.3%. Ten (58.8%) of these cases were male, and the mean age was 68 years (median 73 years, range 38–86 years). The case-fatality rate was 2.9% among the 102 cases less than 60 years of age and 53.8% among the 26 cases 60 years or older. For the cases who were already hospital inpatients or were seeking medical attention in the emergency department before their SARS exposure, the case-fatality rate was 0% among the 8 patients less than 60 years and 90.0% among the 10 older patients. For close contacts, hospital staff and visitors, the case-fatality rate was 3.3% among the 94 cases less than 60 years and 31.3% among the 16 older cases. The mean duration between the onset of symptoms and death was 23 days (range 9–57 days). The medical history of the 17 cases who died is reported in Table 3.
Table 3
Of the surviving 111 cases, 2 are still in the hospital and 109 have been discharged home.
Transmission chain
Transmission from the index case resulted in at least 6 generations of transmission, 4 of which were a result of nosocomial spread. Of the 128 cases, 120 (93.8%) had documented contact with a SARS case or with a ward where there was a known SARS case. The links between 100 cases in our nosocomial cluster were established and, of these, 84 could be mapped back to the 6 cases in the index family (the index case, her son [case A] and 4 members of case A's family) (Fig. 2). The remaining 16 cases formed 6 separate clusters in which the connection to the main hospital cluster has not yet been determined.

Fig. 2: Transmission of 84 probable and suspect cases of SARS in the nosocomial outbreak that could be linked to the 6 members of the index family (the index case, her son [case A] and 4 members of case A's family). Photo: Myra Rudakewich
The remaining 28 cases included 20 cases for whom we could not establish links to our nosocomial cluster but who had documented exposure to multiple SARS cases on the same ward or to a number of different hospital wards where there was a known SARS case. They included 5 patients, 7 hospital staff (including 2 housekeepers, 2 technologists and 3 other hospital staff) and 8 visitors who visited to the hospital on multiple occasions. The remaining 8 cases, including health care workers and patients, were all from one hospital ward and had symptom onset between Mar. 17 and 22, 2003; this ward is not known to have admitted a SARS case.
The index case and her husband had vacationed in Hong Kong and had stayed at a hotel in Kowloon from Feb. 18 to 21, 2003. The index case began to experience symptoms after her return on Feb. 23 and died at home on Mar. 5. During her illness, family members, including her son (case A), provided care at home. Case A became ill on Feb. 27 and presented to the index hospital on Mar. 7.8
Nosocomial transmission in the hospital began when case A presented to the emergency department on Mar. 7 with severe respiratory symptoms. He was placed in a general observation area of the emergency department and received nebulized salbutamol. During this time, SARS was transmitted to 2 other patients in the emergency department (cases B and C). Case B, who had presented with rapid atrial fibrillation, was in the bed adjacent to case A, about 1.5 m away and separated by a curtain, and was discharged home after 9 hours in the emergency department. Case C, who had presented with shortness of breath secondary to a pleural effusion, was 3 beds (about 5 m) away from case A and was transferred to a hospital ward and later discharged home on Mar. 10. The 3 patients were cared for by the same nurse.
Case A was transferred briefly to a medical unit, then to the ICU 18 hours after his presentation to the emergency department. Three hours later, he was placed in airborne isolation because tuberculosis was included in his differential diagnosis. Contact and droplet precautions were implemented on Mar. 10 by ICU staff caring for case A, and the patient remained in isolation until his death, on Mar. 13. Case A's family visited him in the ICU on Mar. 8, 9 and 10. During this time, some family members were febrile, and 2 were experiencing respiratory symptoms. Chest radiographs were taken of the family members on Mar. 9 and again on Mar. 11. Four members had abnormal radiographs and were instructed to wear masks at all times, wash their hands upon entering and leaving the ICU and limit their visits to the ICU.
On Mar. 12, the WHO alerted the global community to a severe respiratory syndrome that was spreading among health care workers in Hanoi, Vietnam, and Hong Kong. The alert was forwarded to infectious disease and emergency department physicians in Toronto. The following day, case A died and it became clear that several other family members had worsening illness. The clinicians involved and the local public health unit suspected the family's illnesses might be linked to cases of atypical pneumonia reported in Hong Kong. Four family members were admitted to 3 different hospitals on Mar. 13, and another family member was admitted to hospital on Mar. 14. All were managed using airborne, droplet and contact precautions. No further transmission from these cases occurred after admission to hospital.
Case B became febrile on Mar. 10, 3 days after exposure to case A in the emergency deparment and discharge home. Respiratory symptoms evolved over the next 5 days. He was brought to the index hospital on Mar. 16 by 2 Emergency Medical Services (EMS) paramedics, who did not immediately use contact and droplet precautions. After 9 hours in the emergency department, where airborne, contact and droplet precautions were used, case B was transferred to an isolation room in the ICU. His wife became ill on Mar. 16. She was in the emergency department with case B on Mar. 16 (no precautions used) and visited him in the ICU on Mar. 21 (precautions used); he died later that day. The infection also spread to 3 other members of case B's family. SARS developed in a number of people who were in contact with case B and his wife on Mar. 16, including the 2 paramedics who brought him to the hospital, a firefighter (also present at the EMS call), 5 emergency department staff, 1 other hospital staff, 2 patients in the emergency department, 1 housekeeper who worked in the emergency department while case B was there, and 7 visitors who were also in the emergency department at the same time as case B (symptom onset Mar. 19 to 26). The 16 hospital staff, visitors and patients transmitted the infection to 8 household members and 8 other family contacts. In the ICU, intubation for mechanical ventilation of case B was performed by a physician wearing a surgical mask, gown and gloves. He subsequently acquired SARS and transmitted the infection to a member of his family. Three ICU nurses who were present at the intubation and who used droplet and contact precautions had onset of early symptoms between Mar. 18 and 20. One transmitted the infection to a household member.
Case C became ill on Mar. 13 with symptoms of a myocardial infarction and was brought to the index hospital by EMS personnel. It was unknown that he had been in contact with case A on Mar. 7, and thus it was not recognized that he had SARS. As a result, he was not isolated, and other precautions were not used. He was admitted to the coronary care unit (CCU) for 3 days and then transferred to another hospital for renal dialysis. He remained in the other hospital until his death, on Mar. 29. Subsequent transmission of SARS occurred within that hospital.9 Case C's wife became ill on Mar. 26. At the index hospital, case C transmitted SARS to 1 patient in the emergency department, 3 emergency department staff, 1 housekeeper who worked in the emergency department while case C was there, 1 physician, 2 hospital technologists, 2 CCU patients and 7 CCU staff. One of the EMS paramedics who transported case C to the index hospital also became ill. Further transmission then occurred from ill staff at the index hospital to 6 of their family members, 1 patient, 1 medical clinic staff and 1 other nurse in the emergency department.
Incubation period
Forty-two (32.8%) of the 128 cases had a single known contact with a SARS case. The mean incubation period in these cases was 5 days (median 4 days; range 2–10 days).
Attack rates
Nurses in the index hospital usually worked 12-hour shifts. In the emergency department, there were at least 6 nursing shifts during which there could have been exposure to a SARS case without the use of contact or droplet precautions. The attack rate among nurses who worked in the emergency department while a SARS case was there was 22.2% (8/36). Further analysis by number of hours worked in the emergency department during the exposure period resulted in an attack rate of 13.6 cases per 1000 nursing-hours worked. In the ICU, there was only a 3-hour period when there may have been unprotected exposure. The attack rate among ICU nurses was 10.3% (4/39), or 2.4 cases per 1000 nursing-hours worked. In the CCU, there were at least 6 nursing shifts during which nurses had unprotected exposure. The attack rate among CCU nurses was 60.0% (6/10), or 31.3 cases per 1000 nursing-hours worked.
Interpretation
The importation of 1 case of SARS to Toronto on Feb. 23, 2003, led to 5 cases among the woman's family contacts and at least 128 cases through subsequent spread in a single local hospital between late February and mid-April.
Airborne, contact and droplet precautions were implemented by staff caring for known cases of SARS in the index hospital on Mar. 13, the day after the WHO issued its global alert. At that time, only the index case's son (case A) and 3 other family members were identified as having SARS. However, by Mar. 13, transmission of SARS had already occurred within the hospital. Following the initial investigation, contact and droplet precautions were implemented for all patients in the ICU on Mar. 22, and the ICU and emergency department were closed on Mar. 23. On Mar. 24, following the identification of staff and patient cases not linked to the ICU or emergency department, the hospital was closed to admissions, outpatient clinics were closed, and discharged patients were placed into quarantine at home for 10 days. Along with an increased emphasis on handwashing, additional precautions, including the use of gowns, gloves, N95 or equivalent masks, and eye protection, were implemented for all patient care, and single or negative-pressure rooms were used for all febrile patients. Dedicated equipment was used for all patients, and patients were restricted to their rooms except for medically necessary tests. Staff wore N95 masks at all times in the hospital and were placed into quarantine at home (with the exception of coming to work). Volunteers and medical students were excluded from the hospital, and patient visits were restricted. There has been no further transmission within the hospital since this time.
The epidemiological links described in our investigation of this nosocomial cluster support the theory that the SARS agent is transmitted mainly through respiratory droplets and direct contact.6,8,10 Transmission in most cases occurred in those who had close contact with a SARS case. The additional precautions implemented were effective in halting the transmission in the hospital.
In 8 cases, the common exposure appears to have been contact with a hospital ward that is not known to have admitted a SARS case. Although it is not yet known whether individuals are infectious before the onset of symptoms, it is hypothesized that these individuals had exposure to a patient, hospital worker or visitor with SARS who has not yet been identified.
The physician who was exposed to SARS while performing the intubation of case B was wearing a gown, gloves and a surgical mask during the procedure. Although these precautions appear to be effective in preventing the transmission of SARS under most circumstances,11 transmission despite such precautions has occurred in Toronto during at least 2 other intubations when droplet and contact precautions were used.12 During such high-risk procedures, the absence of protective eyewear or other minor breaches in precautions may result in disease transmission.
On Mar. 16, at least 16 people became ill after exposure to case B and his wife in the emergency department. Factors that may have contributed to the transmission include the proximity of the patients, the movement of the nursing staff among the patients and the movement of a symptomatic family member within the emergency department. Although there may have been fomites and airborne spread, the fact that all of the people who became ill were exposed when known symptomatic people were in the room makes this less likely. The investigation of transmission on Mar. 16 is underway.
Our finding that the incubation period varied from 2 to 10 days supports the data that have been reported to date.10,13,14
The majority of the 17 people who died were older (aged 60 years or more) or had comorbid conditions. The case-fatality rates among cases less than 60 years of age (2.9%) and among those 60 years or older (53.8%) were comparable to those reported in Hong Kong (6.8% and 55.0% respectively).13 Despite the higher case-fatality rate among the older cases, we found that the rate was much higher among cases who were already hospital inpatients before SARS exposure than among staff, visitors and close contacts. The overall case-fatality rate was higher than that reported by others (13.3% v. 2.0%–6.5%);10,15,16 however, our follow-up period was longer (up to 60 days in some cases). The use of slightly different case definitions and different methods for calculating the case-fatality rate also makes comparisons difficult. Given the substantial effect of age, the overall case-fatality rates may be misleading if different age groups are affected.
The highest attack rate among the nursing staff occurred in the CCU (60.0%). This rate is likely due to the intense, close-contact care given to the SARS cases in the CCU compared with the shorter contact with patients in the emergency department. In addition, the CCU nurses worked more unprotected shifts than the 3 hours of unprotected exposure to a SARS case in the ICU. Although ICU staff provide more close-contact care than emergency department staff, it is likely that the shorter period of unprotected exposure in the ICU resulted in a lower attack rate among the ICU nurses than among the emergency department staff.
Contact and droplet precautions were implemented throughout the hospital on Mar. 25. After the elapse of 2 full incubation periods (20 days), there was no evidence of further transmission within the hospital. However, cases from the hospital caused further spread of the infection to family members and social contacts. In addition, patients in the hospital who were not recognized as having SARS were transferred to other hospitals, which resulted in transmission in those settings.9 This led to a further 119 cases in the Greater Toronto Area. Intensive infection control efforts led to the control of the spread. After 27 days with no new SARS cases identified in Toronto, contact and droplet precautions were lifted in non-SARS hospital wards on May 16. However, on May 22, a second wave of cases was reported to public health officials,17,18 which resulted in a further 118 cases in the Greater Toronto Area as of July 10, 2003.
Many questions remain with respect to the cause, mode of transmission, period of infectivity, predisposing factors, effectiveness of and compliance with infection control practices, and the natural history and long-term sequelae of SARS. Continuing epidemiological and laboratory investigations in Toronto and around the world will be required to provide answers to these questions.
The findings from our investigation provide insight into the mode of transmission, period of infectivity, and the morbidity and mortality associated with SARS. We have demonstrated that transmission can easily go undetected and lead to a significant number of cases in a short period. Even a limited number of undetected cases has important implications for the health care system, as demonstrated by the large nosocomial cluster arising from the 1 index case in our investigation. It is imperative that we remain vigilant in our surveillance activities and maintain strict infection control precautions to contain this new disease.
Acknowledgments
We thank Carol Tinga, Shira Korman, Anne-Luise Winter, Linda Panaro, Ian Johnson, Bill Mindell, Maureen Perrin and Michelyn Wood for their technical and academic support. We also thank the Ontario SARS Scientific Advisory Committee and the Ontario Ministry of Health and Long-Term Care. We would especially like to thank the staff of the hospital investigated in our study and the local health units in Toronto, York Region, Durham, Peel and Simcoe County for their tireless efforts to control this outbreak.
Footnotes
Fast-tracked article. Published at www.cmaj.ca on July 29, 2003.
This article has been peer reviewed.
Contributors: All authors contributed to the conception and design, or analysis and interpretation of the data, and the drafting or critical revision of the article. All authors approved the final version to be published.
Competing interests: None declared.
Correspondence to: Dr. Bonnie Henry, Toronto Public Health, 277 Victoria St., Toronto ON M5B 1W2
References
- 1.Tsang K, Ho P, Ooi G, Yee W, Wang T, Chan-Yeung M, et al. A cluster of cases of severe acute respiratory syndrome in Hong Kong. N Engl J Med 2003; 348(20):1977-85. [DOI] [PubMed]
- 2.Ksiazek T, Erdman D, Goldsmith C, Zaki S, Peret T, Emery S, et al. A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med 2003; 348(20):1953-66. [DOI] [PubMed]
- 3.Drosten C, Gunther S, Preiser W, van der Werf S, Brodt H, Becker S, et al. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med 2003;348(20):1967-76. [DOI] [PubMed]
- 4.World Health Organization. A multicentre collaboration to investigate the cause of severe acute respiratory syndrome. Lancet 2003;361:1730-3. [DOI] [PMC free article] [PubMed]
- 5.Fouchier R, Kuiken T, Schutten M, van Amerongen G, van Doornum J, van den Hoogen B, et al. Koch's postulates fulfilled for SARS virus. Nature 2003;423: 240. [DOI] [PMC free article] [PubMed]
- 6.Update: outbreak of severe acute respiratory syndrome — worldwide, 2003. MMWR Morbid Mortal Wkly Rep 2003;52:241-8. [PubMed]
- 7.Epidemiology, clinical presentation and laboratory investigation of severe acute respiratory syndrome (SARS) in Canada, March 2003. Can Commun Dis Rep 2003;29(8):71-5. [PubMed]
- 8.Poutanen S, Low D, Henry B, Finkelstein S, Rose D, Green K, et al. Identification of severe acute respiratory syndrome in Canada. N Engl J Med 2003; 348 (20):1995-2005. [DOI] [PubMed]
- 9.Dwosh H, Hong H, Austgarden D, Herman S, Schabas R. Identification and containment of an outbreak of SARS in a community hospital. CMAJ 2003; 168 (11):1415-20. [PMC free article] [PubMed]
- 10.Booth C, Matukas L, Tomlinson G, Rachlis A, Rose D, Dwosh H, et al. Clinical features and short-term outcomes of 144 patients with SARS in the Greater Toronto Area. JAMA 2003;289(21):2801-9. [DOI] [PubMed]
- 11.Seto W, Tsang D, Yung R, Ching T, Ng T, Ho M, et al. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS). Lancet 2003;361:1519-20. [DOI] [PMC free article] [PubMed]
- 12.Cluster of severe acute respiratory syndrome cases among protected health care workers — Toronto, Canada, April 2003. MMWR Morbid Mortal Wkly Rep 2003;52(19):433-6. [PubMed]
- 13.Donnelly C, Ghani A, Leung G, Hedley A, Fraser C, Riley S, et al. Epidemiological determinants of spread of causal agent of severe acute respiratory syndrome in Hong Kong. Lancet 2003;361:1761-6. [DOI] [PMC free article] [PubMed]
- 14.Avendano M, Derkach P, Swan S. Clinical course and management of SARS in health care workers in Toronto: a case series. CMAJ 2003;168(13):1649-60. [PMC free article] [PubMed]
- 15.Lee N, Hui D, Wu A, Chan P, Cameron P, Gavin MJ, et al. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med 2003; 348 (20):1986-94. [DOI] [PubMed]
- 16.Peiris J, Lai S, Poon L, Guan Y, Yam L, Lim W, et al. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet 2003;361:1319-25. [DOI] [PMC free article] [PubMed]
- 17.Kondro W. SARS back in Canada. Lancet 2003;361:1876. [DOI] [PMC free article] [PubMed]
- 18.Spurgeon D. Toronto succumbs to SARS a second time. BMJ 2003;326:1162. [DOI] [PMC free article] [PubMed]


