Abstract
ANAPHYLAXIS IS A SEVERE SYSTEMIC ALLERGIC reaction that is potentially fatal. It requires prompt recognition and immediate management. Anaphylaxis has a rapid onset with multiple organ–system involvement and is mostly caused by specific antigens in sensitized individuals. Reactions typically follow a uniphasic course, however, 20% will be biphasic in nature. The second phase usually occurs after an asymptomatic period of 1–8 hours, but there may be a 24-hour delay. Protracted anaphylaxis may persist beyond 24 hours. Concurrent β-blocker therapy may adversely affect the response to management. Epinephrine is the treatment of choice and should be administered immediately. Secondary measures include circulatory support, H1 and H2 antagonists, corticosteroids and, occasionally, bronchodilators. Post-treatment observation of these patients is necessary, and they should remain within ready access of emergency care for the following 48 hours.
Case
A 19-year-old woman with a past history of seasonal allergic rhinitis presented to her family doctor's office for routine injection of allergen immunotherapy (ragweed). She had never had a problem with her injections. She received her injection and, after waiting in the office for 15 minutes afterward, left without incident. Five minutes after leaving the office, however, she began to notice itching in the palms of her hands, followed by shortness of breath and a sensation of throat swelling. She returned to the office, where she was noted to be flushed, sweating profusely and in moderate distress. What features constitute the diagnosis of anaphylaxis? What is the appropriate initial and ancillary management of anaphylaxis? How should such a patient be followed after symptom resolution?
Anaphylaxis is the clinical syndrome that represents the most severe systemic allergic reaction. It results from the immunologically induced release of mast cell and/or basophil mediators after exposure to a specific antigen in previously sensitized individuals. Anaphylaxis is a medical emergency that requires immediate attention. If medical attention is delayed, death may occur most commonly from cardiovascular collapse or airway obstruction, or both. Although any substance has the potential to cause anaphylaxis, the most common causes of IgE-mediated anaphylaxis are insect stings, medications, latex, peanuts1 and tree nuts (e.g., walnuts, hazelnuts, almonds, cashews, pecans and pistachios), shellfish and fish, milk, eggs and wheat. Exercise-induced anaphylaxis and idiopathic anaphylaxis also occur, being mediated by different mechanisms.2,3 Anaphylactoid reactions are clinically indistinguishable from anaphylaxis, but are not IgE mediated and are seen in response to opiates, NSAIDs and radiocontrast agents.
In this review, we discuss the clinical features and accurate diagnosis of anaphylaxis and consider current recommendations for its management. As anaphylaxis is a potentially life-threatening reaction that may be encountered by any practitioner of medicine, all physicians will benefit from knowledge of its recognition and appropriate treatment. We also provide a patient information sheet (Appendix 1).
Diagnosis
Anaphylaxis represents a severe systemic allergic reaction. No universally accepted definition exists because anaphylaxis comprises a constellation of features. A good working definition, however, is that used by the Canadian Pediatric Surveillance Program,4 which defines anaphylaxis as “a severe allergic reaction to any stimulus, having sudden onset and generally lasting less than 24 hours, involving one or more body systems and producing one or more symptoms such as hives, flushing, itching, angioedema, stridor, wheezing, shortness of breath, vomiting, diarrhea, or shock.”
Clinical features
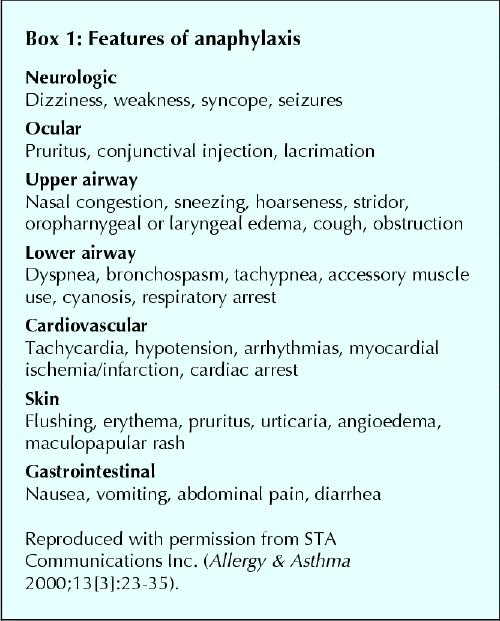
Because anaphylaxis is a generalized reaction, a wide variety of clinical signs and symptoms may be observed5 (Box 1). Often, patients will describe an impending sense of death (angor animi). Infrequently, seizures have been reported during anaphylaxis. Death due to anaphylaxis usually occurs as a result of respiratory obstruction or cardiovascular collapse, or both. It is thought that there is a direct correlation between the immediacy of onset of symptoms after exposure to the triggering agent and the severity of the episode, with the more rapid the onset, the more severe the event.6 Any delay before the administration of epinephrine and a history of asthma are also significant risk factors for anaphylactic death.7
Box 1.
Symptoms of anaphylaxis generally have their onset within minutes, but occasionally occur as late as 1 hour after exposure to the offending antigen. The signs and symptoms may follow a uniphasic course, with resolution of symptoms within hours of treatment, but about 20% of anaphylactic reactions will follow a biphasic course.8 Because the initial report by Stark and Sullivan described asymptomatic periods of 1–8 hours,8 this is the time frame often quoted in the medical literature, although some authors report a smaller window of 1–3 hours9,10 based on another case series.7 Recently, the mean time to onset of second-phase reactivity has been documented to be 10 hours.11 A number of cases have been documented of biphasic reactivity occurring as late as 24–38 hours after the initial manifestation of the anaphylactic reaction (Fig. 1).11,12,13 We have found that about one-third of the second-phase reactions were more severe than the initial reaction, one-third were similar and one-third were milder.11 Mortality from biphasic reactions is possible but is not adequately documented in the literature.
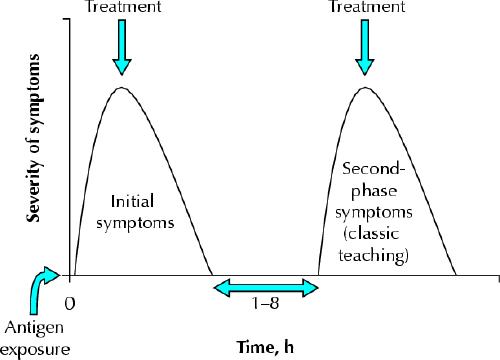
Fig. 1: Schematic representation of a biphasic anaphylactic reaction. The second-phase reaction has been described as occurring between 1 and 8 hours after the initial reaction, but new evidence suggests that this second phase may occur up to 38 hours (mean 10 hours) after the initial reaction. About one-third of the second-phase reactions are more severe, one-third are as severe and one-third are less severe.
Currently, many authors recommend the administration of corticosteroids to prevent or minimize the second phase, as this has been demonstrated to be beneficial.14,15 However, there have also been several documented cases of patients who received corticosteroid therapy and yet went on to experience severe biphasic or protracted reactions.8,12 Thus, physicians must anticipate the occurrence of severe second-phase reactions, even when corticosteroids have been administered. Protracted anaphylaxis, which is frequently associated with profound hypotension and sometimes lasts longer than 24 hours, is minimally responsive to aggressive therapy,8 and has a poor prognosis.
Differential diagnosis
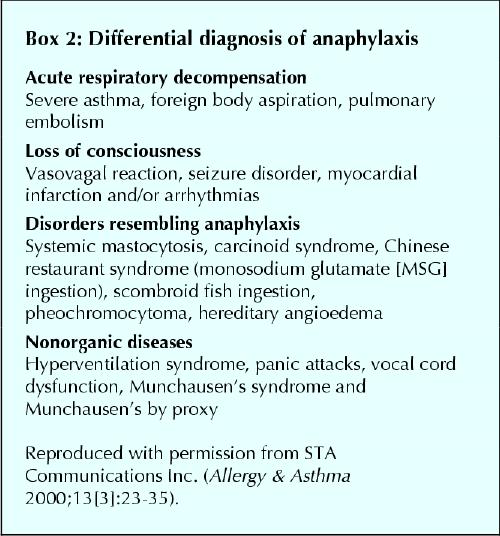
In practical terms, it is not necessary to differentiate between anaphylactic and anaphylactoid reactions at the time of patient presentation, as both respond to the same treatment, however, anaphylactic shock must be differentiated from other causes of circulatory collapse. The most common conditions that mimic anaphylaxis are vasovagal reactions, which are characterized by hypotension, pallor, bradycardia, weakness, nausea, vomiting and diaphoresis. Urticaria, pruritus, angioedema, tachycardia and bronchospasm are not vasovagal responses.
Acute respiratory decompensation from severe asthma attacks, foreign body aspiration and pulmonary embolism can feature respiratory symptoms suggestive of anaphylaxis, but other characteristics (e.g., pruritis, urticaria, angioedema) are lacking. Hereditary angioedema, precipitated by nonspecific environmental, physiological and emotional stressors, usually presents with swelling of the lips, tongue, upper airway and other mucosal surfaces, as well as gastrointestinal symptoms such as cramping and diarrhea, but does not involve pruritus and urticaria. As this is an autosomal dominant condition, a family history of hereditary angioedema is usually present. Other conditions such as seizure disorders, myocardial infarction and/or arrhythmias may infrequently present initially with similarities to anaphylaxis, but are readily distinguished clinically. A full differential diagnosis is presented in Box 2.
Box 2.
Management
Anaphylaxis is a medical emergency that requires immediate treatment. The management of acute anaphylaxis is summarized in Table 1. Parenteral epinephrine is the cornerstone of management.16 The dosage for adults is 0.3–0.5 mL of a 1:1000 dilution, and recent research has established the intramuscular route to be superior to the subcutaneous route.17 The dosage for children is 0.01 mL/kg, up to a maximum 0.3 mL of a 1:1000 dilution. Epinephrine can be reinjected every 5–15 minutes until there is resolution of the anaphylaxis or signs of hyperadrenalism (including palpitations, tremor, uncomfortable apprehension and anxiety) occur. Intravenous epinephrine (1:10 000 dilution) should be administered only in severe hypotensive shock because of its potential for tachyarrhythmias. An adequate airway must be established and maintained, and supplemental oxygen given to all patients with anaphylactic reactions.
Table 1
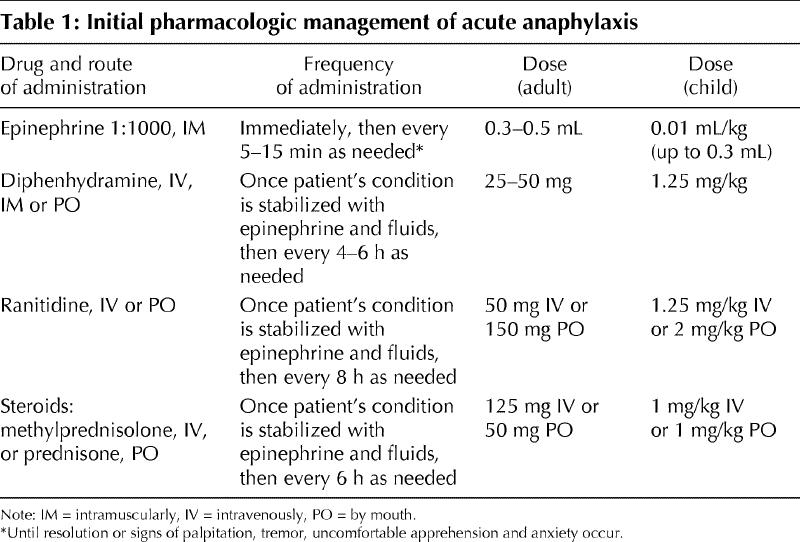
Other supplementary therapy for anaphylaxis includes the use of H1 and H2 antihistamines, for example, diphenhydramine, 25–50 mg intravenously, and ranitidine, 50 mg intravenously or 150 mg orally. Current recommendations are to administer these agents in combination, because H1 and H2 blockade is more effective than H1 blockade alone in preventing symptomatology of anaphylaxis in experimental models.18 Inhaled β2- agonists (e.g., salbutamol) are useful when bronchospasm is present. Corticosteroids (e.g., methylprednisolone, 125 mg intravenously, or prednisone, 50 mg orally; the intravenous route of administration is often used for more severe reactions) may help prevent or minimize second-phase reactions, but biphasic reactions are well documented in patients who received corticosteroids as part of their initial management.8,12 Hypotensive patients should receive intravenous fluid support with crystalloid or colloid, and severe cases may require vasopressor agents such as dopamine or high-dilution epinephrine (1:10 000). Individuals who use β-blockers (and possibly angiotensin-converting-enzyme inhibitors, although the evidence is incomplete) may not respond completely to epinephrine, in which case glucagon should be administered at a dose of 5–15 μg/min intravenously. Glucagon has inotropic, chronotropic and vasoactive effects that are independent of β-receptors, and it also causes endogenous catecholamine release. Considering the reported incomplete prophylactic coverage of corticosteroids and the acknowledged benefit of histamine blockade to prevent anaphylactoid reactions (i.e., to radiocontrast media),19 it is the standard practice in our unit to provide 4 days of regularly dosed prednisone and diphenhydramine upon discharge post anaphylaxis.
Finally, post-treatment observation of these patients is required, owing to the potential for a second phase of reactivity. Although most of these reactions will occur within 1–8 hours, prolonged asymptomatic windows of up to 25 and 38 hours have been reported.11,12 Observation in a monitored setting for 24 hours post anaphylaxis would be ideal, but is often not practical. We recommend that patients be discharged from the emergency department only with adequate supervision, and to environments with easy access to the emergency medical response system should symptoms recur. Following successful treatment of anaphylaxis, the patient should stay where he or she can call 911 with timely delivery to hospital for the next 48 hours.
Prevention
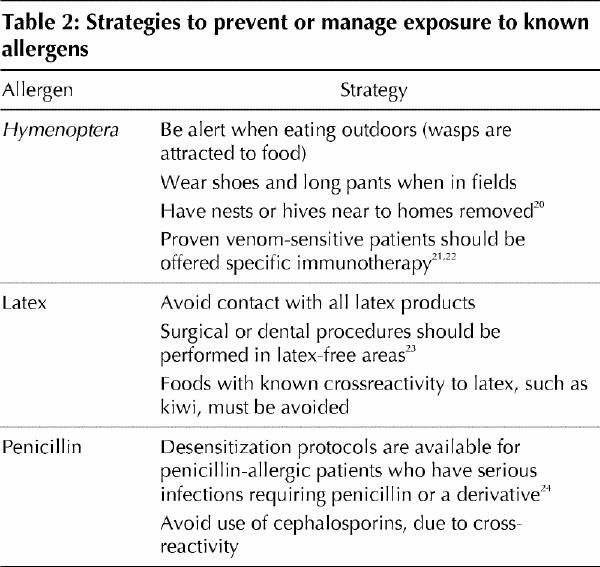
The first essential step in the prevention of anaphylaxis is identification of the causative agent, if possible. Confirmation of the cause requires referral to an allergist for a skin prick test and, when deemed necessary, in-vitro assessment for the presence of specific IgE antibodies. Referral for skin prick testing is particularly important when no causative agent can be clearly identified by history or for bee or wasp stings, because confirmation of IgE-mediated reactivity is necessary to offer potentially curative immunotherapy (see Table 2).20,21,22,23,24 Specific management and preventive strategies by allergen are discussed in Table 2. In the case of drug or food allergy, not only must the offending substance be avoided, but the potential for crossreactivity (e.g., cephalosporins in the case of penicillin allergy25) must also be recognized.
Table 2
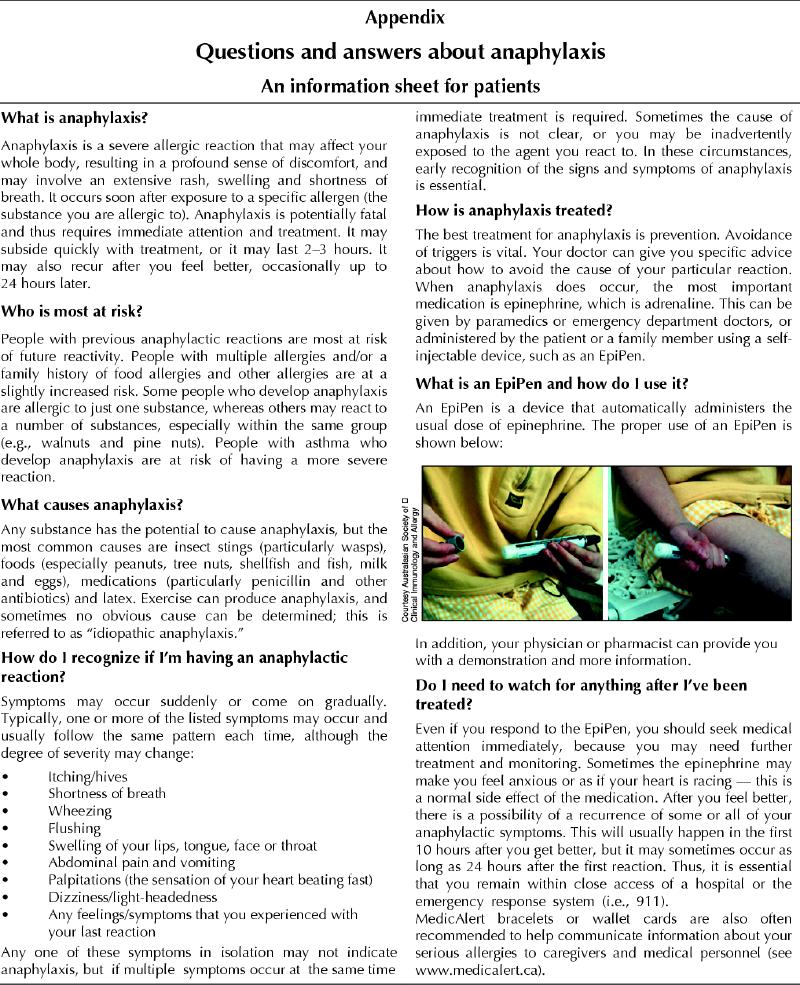
Patients should be prescribed, and be instructed in the use of, self-injectable epinephrine (e.g., EpiPen). They should also obtain a MedicAlert bracelet or necklace. Subsequent reactions typically escalate in severity, but they may remain the same or even be diminished. If sufficient time elapses without contact with the triggering agent, a decrease in or loss of sensitivity occurs in a significant number of patients.6
Case revisited
The family doctor immediately assessed the patient's condition, recognized anaphylactic reactivity and administered an adult self-injectable epinephrine device and an intramuscular injection of diphenhydramine, 50 mg. The patient began to feel better within 5–10 minutes of the epinephrine injection, and at 30 minutes claimed to feel “completely fine.” At her physician's insistence, however, she was transported to the local hospital's emergency department for further monitoring, where about 3 hours after initial resolution of symptoms, she noted whole-body urticaria and shortness of breath and had swelling of her lips and hands. She was given an additional injection of epinephrine at 1:1000 dilution, 0.3 mL intramuscularly, followed by ranitidine, 50 mg intravenously, and methylprednisolone, 125 mg intravenously. Her symptoms abated over the ensuing 30 minutes, and she was monitored for an additional 5 hours in the emergency department without further incident. She was discharged home with her mother with a prescription for self-injectable epinephrine and a referral back to her allergist for reassessment of her immunotherapy schedule, and was advised to remain in an area with ready access to the emergency response system for the next 48 hours.
Conclusion
Many cases of anaphylaxis, and especially the potential for second-phase reaction, are underrecognized and undertreated, with potentially life-threatening consequences. Immediate administration of epinephrine intramuscularly is often life saving, but repeated doses may be necessary in combination with other medications. Once recovered, patients must be monitored in some capacity for up to 48 hours.
Appendix 1.
Footnotes
A patient information sheet appears on page 312
This article has been peer reviewed.
Contributors: Dr. Ellis was responsible for the literature search, review and appraisal. Dr. Day was responsible for critically revising the article for important intellectual content. Both authors were responsible for conceiving the article and gave final approval of the version to be published.
Competing interests: None declared.
Correspondence to: Dr. Anne K. Ellis, c/o Dr. James H. Day, Division of Allergy and Immunology, Kingston General Hospital, Kingston ON K7L 2V7; fax 613 546-3079; ellisa@kgh.kari.net
References
- 1.Al-Muhsen S, Clarke AE, Kagan RS. Peanut allergy: an overview. CMAJ 2003;168(10):1279-85. [PMC free article] [PubMed]
- 2.Sheffer A, Austen K. Exercise-induced anaphylaxis. J Allergy Clin Immunol 1984; 73(5 Pt 2):699-703. [DOI] [PubMed]
- 3.Patterson R, Harris KE. Idiopathic anaphylaxis. Allergy Asthma Proc 1999; 20 (5): 311-5. [DOI] [PubMed]
- 4.Simons FER, Chad Z, Gold M. Real-time reporting of anaphylaxis in infants, children and adolescents by physicians involved in the Canadian Pediatric Surveillance Program. J Allergy Clin Immunol 2002;109:S181.
- 5.James JM. Anaphylaxis: multiple etiologies-focused therapy. J Ark Med Soc 1996;93(6):281-7. [PubMed]
- 6.Terr AI. Anaphylaxis. Clin Rev Allergy 1985;3(1):3-23. [DOI] [PubMed]
- 7.Sampson HA, Mendelson L, Rosen JP. Fatal and near-fatal anaphylactic reactions to food in children and adolescents. N Engl J Med 1992;327:380-4. [DOI] [PubMed]
- 8.Stark BJ, Sullivan TJ. Biphasic and protracted anaphylaxis. J Allergy Clin Immunol 1986;78(1 Pt 1):76-83. [DOI] [PubMed]
- 9.Sampson HA. Food anaphylaxis. Br Med Bull 2000;56(4):925-35. [DOI] [PubMed]
- 10.Burks AW, Sampson HA. Anaphylaxis and food allergy. Clin Rev Allergy Immunol 1999;17(3):339-60. [DOI] [PubMed]
- 11.Ellis AK, Day JH. Biphasic anaphylaxis: a prospective evaluation of incidence, characteristics, and predictors [abstract]. Proceedings of the Fifth Annual Meeting for Basic and Clinical Research Trainees; 2002 May 29; Kingston (ON).
- 12.Ellis AK, Day JH. Biphasic anaphylaxis with unusually late onset second phase: a case report. Can J Allergy ClinImmunol 1997;2(3):106-9.
- 13.Brazil E, MacNamara AF. “Not so immediate” hypersensitivity — the danger of biphasic anaphylactic reactions. J Accid Emerg Med 1998;15:252-3. [DOI] [PMC free article] [PubMed]
- 14.Sheffer AL. Anaphylaxis. J Allergy Clin Immunol 1985;75(2):227-33. [DOI] [PubMed]
- 15.Lockey RF, Bukantz SC. Allergic emergencies. Med Clin North Am 1974;58(1):147-56. [DOI] [PubMed]
- 16.Chamberlain D. Emergency medical treatment of anaphylactic reactions. Project Team of the Resuscitation Council (UK). J Accid Emerg Med 1999;16(4):243-7. [DOI] [PMC free article] [PubMed]
- 17.Simons FER, Gu X, Simons KJ. Epinephrine absorption in adults: intramuscular versus subcutaneous injection. J Allergy Clin Immunol 2001;108(5):871-3. [DOI] [PubMed]
- 18.Lieberman P. The use of antihistamines in the prevention and treatment of anaphylaxis and anaphylactoid reactions. J Allergy Clin Immunol 1990;86(4 Pt 2):684-6. [DOI] [PubMed]
- 19.Greenberger PA. Contrast media reactions. J Allergy Clin Immunol 1984; 74:600-5. [DOI] [PubMed]
- 20.Ellis AK, Day JH. Allergy to insect bites and stings. Allergy 1996;9(3):11-22.
- 21.Reisman RE. Insect stings. N Engl J Med 1994;331(8):523-7. [DOI] [PubMed]
- 22.Reisman RE, Livingston A. Venom immunotherapy: 10 years of experience with administration of single venoms and 50 μg maintenance doses. J Allergy Clin Immunol 1992;89(6):1189-95. [DOI] [PubMed]
- 23.Sussman GL, Beezhold DH. Allergy to latex rubber. Ann Intern Med 1995; 122(1):43-6. [DOI] [PubMed]
- 24.Borish L, Tamir R, Rosenwasser LJ. Intravenous desensitization to beta- lactam antibiotics. J Allergy Clin Immunol 1987;80(3 pt 1):314-9. [DOI] [PubMed]
- 25.Saxon A. Immediate hypersensitivity reactions to beta-lactam antibiotics. Ann Intern Med 1987;107(2):204-15. [DOI] [PubMed]
Supplementary Reading
- ·.Ellis AK, Day JH. Anaphylaxis: diagnosis and treatment. Allergy Asthma 2000;13(3):22-35.
- ·.Project Team of the Resuscitation Council (UK). Consensus guidelines: emergency medical treatment of anaphylactic reactions. Resuscitation 1999;41(2):93-9. [PubMed]
- ·.Wuthrich B, Ballmer-Weber BK. Food-induced anaphylaxis. Allergy 2001;56(Suppl 67):102-4. [DOI] [PubMed]
Related Web Sites
- ·.Anaphylaxis Canada: www.anaphylaxis.org
- ·.Food Allergy & Anaphylaxis Network: www.foodallergy.org/anaphylaxis.html
- ·.Canadian Society of Allergy and Clinical Immunology: http://csaci.medical.org


