Abstract
Angiogenesis is a key process in the pathogenesis of inflammatory arthritis. Angiogenin is one of the most potent inducers of neovascularization in experimental models in vivo. To look for evidence that angiogenin is involved in inflammatory joint disease, we examined plasma and synovial fluid (SF) samples from rheumatology patients and synovial fibroblast cell culture supernatants. Angiogenin levels were determined by radioimmunoassay and ELISA. Plasma angiogenin concentrations ranged from 96 to 478 ng/ml, with no significant difference between patients and normal controls. In SF, angiogenin concentrations were significantly higher in patients with acute or chronic synovitis (rheumatoid arthritis (RA): median, 104 ng/ml; range 13–748, n = 14; crystal-induced arthritis (CIA): median, 149 ng/ml; range, 37–616, n = 14, and other chronic inflammatory arthritis: median, 42 ng/ml; range, 15–205; n = 9) than in the 18 patients with osteoarthritis (OA) (median, 20 ng/ml; range 8–116) (P < 0·0001, anova). Angiogenin levels in SF from RA patients in remission with secondary OA were similar to those achieved in primary OA, and decreased in parallel with the resolution of acute gout. Angiogenin protein was released by cultured synovial fibroblasts from OA and RA patients, and reached 1·18 ng/106 cells/day. These data suggest that angiogenin may mediate local inflammation in arthritis via effects on angiogenesis and leucocyte regulation.
Keywords: angiogenin, crystal-induced inflammation, osteoarthritis, rheumatoid arthritis, synovial fibroblasts
Introduction
The pathogenesis of joint articular diseases such as rheumatoid arthritis (RA) [1], crystal-induced arthritis (CIA) [2], and even osteoarthritis (OA) [3] involves an increase in synovial capillaries. Whereas angiogenesis decreases after the resolution of acute arthritis, persistent angiogenesis is the hallmark of chronic inflammatory arthritis [4,5]. In RA, increased angiogenesis and activation of the endothelium lead to synovial tissue proliferation, with pannus formation, and to migration of blood leucocytes to the synovial tissue. As pointed out by Folkman and Klagsbrun, RA can be considered an ‘angiogenic disease’ [6].
Angiogenesis develops in sequential steps including migration, proliferation, and differentiation of the endothelial cells to form capillaries, in combination with extracellular matrix remodelling. Capillary overgrowth results from a local imbalance between positive and negative regulators [7]. In synovial fluid (SF) and synovial tissue from patients with joint disease, many cytokines such as IL-1β [8], IL-6 [9], IL-8 [10], and tumour necrosis factor-α (TNFα [11]), as well as growth factors, have been detected. The growth factors detected to date include fibroblast growth factors (FGFs) [12,13], hepatocyte growth factor (HGF) [14,15], platelet-derived growth factor (PDGF) [13,16], transforming growth factor-β (TGFβ) [17], vascular endothelial growth factor (VEGF) [18,19], and angiogenin [20]. In addition, receptors involved in the angiogenesis process have been found, such as the VEGF receptors Flt-1, KDR, and NP-1 [21]; the receptor tyrosine kinases tie-1 and tie-2 [22], and the HGF receptor c-met [15].
Angiogenin (for a review see [23]) is one of the most active angiogenic factors in experimental models in vivo. It was first isolated from culture media conditioned by human colon carcinoma cells and purified based on its ability to induce angiogenesis in the chick chorioallantoic membrane assay [24]. It is a potent angiogenic agent in the rabbit meniscus [25] and rabbit cornea [24]. Angiogenin is a heparin-binding 14·1-kD polypeptide and a ribonucleolytic enzyme [26,27]. In addition to its strong angiogenic effect, the possible involvement of angiogenin in tumour development is suggested by its overexpression in patients with cancer and the ability of angiogenin antagonists to prevent the growth of human tumour xenografts in athymic mice [28–30]. Furthermore, angiogenin is regulated in vivo and in vitro as an acute-phase protein [31,32]. Therefore, we studied the distribution of angiogenin in plasma and synovial fluid specimens from patients with inflammatory and noninflammatory joint diseases, and we sought to determine whether peripheral blood monocytes and synovial fibroblasts produced angiogenin.
Materials And Methods
Study population
Plasma samples were obtained from 22 patients with OA (n = 5), RA (n = 14), or other inflammatory arthritides (IA) (n = 3). SF was obtained from 55 patients with OA (n = 18), RA (n = 14), crystal-induced arthritis (CIA) (n = 14), or IA (n = 9). All RA patients fulfilled the revised American Rheumatism Association criteria [33]; CIA patients had gout or chondrocalcinosis diagnosed on the basis of inflammatory arthritis with crystals of monosodium urate or calcium pyrophosphate dihydrate, respectively, in their SF by polarized microscope examination. All OA patients had involvement of the knee with typical radiographic changes (osteophytes and joint space narrowing) and fewer than 1000 cells per mm3 of SF at the time of sampling. The other IAs were either psoriatic arthritis or HLA-B27-related oligoarthritis. The controls were healthy blood donors (plasma, n = 15; monocytes, n = 11). The study has been approved by our local ethical committee and informed consent was obtained from all subjects.
Plasma collection
Plasma collected on EDTA from the study participants in the fasting state was centrifuged at 1500 g for 20 min at 20°C, aliquoted, and kept at − 80°C until assay.
Synovial fluids
SF was obtained during routine knee aspiration performed as a diagnostic procedure or as a preliminary to intra-articular injection. For each participant, 3–5 ml of SF was collected on commercial sodium heparinate (5000 IU/ml, 20 µl; Choay, Paris, France) and centrifuged at 3800 g for 10 min at 18°C. Supernatants were collected, aliquoted, and frozen at − 80°C. Routine cell counts were performed on 40 SF specimens.
Monocyte supernatants
Peripheral blood mononuclear cells were isolated on a Ficoll-Hypaque density gradient (density = 1·077) from 45 ml of whole blood drawn on a sterile 3·8% sodium citrate solution and prepared as previously described [34]. Eleven pairs of RA and control monocyte samples were studied. Briefly, monocytes (106) were obtained after 2 h of adhesion on plastic Petri dishes, at 37°C, in RPMI 1640 medium supplemented with 10% foetal bovine serum (FBS), penicillin (100 IU/ml), fungizone (2·5 µg/ml), and 2 mM glutamine. Non-adherent cells were removed by aspiration, and monocytes were subsequently maintained in M199 medium supplemented with penicillin, fungizone, and glutamine without serum, for 24 h in a humidified 5% CO2 atmosphere at 37°C. The supernatants were removed, centrifuged, aliquoted, and kept at − 80°C until use. Monocyte supernatants were obtained from unstimulated cells or after stimulation with 10 µg/ml lipopolysaccharide (LPS) or muramyl dipeptide (MDP, a gift from G. Barr, Institut Pasteur, Paris, France) for 24 h. All culture media and reagents were endotoxin-free (endotoxin levels less than 10 pg/ml as measured by the standard Limulus test, Endotoxin assay, Kabi-Pharmacia, St. Quentin-en-Yvelines, France), and all experiments were done under sterile conditions.
Synovial fibroblast cultures
Synovial tissue specimens were obtained during joint replacement in 8 RA and 8 OA patients and during wrist tenosynovectomy in 3 RA patients. The specimens were collected in sterile phosphate-buffered saline (PBS) supplemented with 100 IU/ml penicillin and 100 µg/ml streptomycin. They were washed in sterile PBS, dissected, cut into 1- to 2-mm3 pieces, and subjected to enzymatic digestion. Four millilitres of collagenase-dispase (1 mg/ml, Boehringer, Meylan, France) and DNAase I grade II (1 mg/ml, Boehringer) were added to RPMI 1640 for 60 min at 37°C with regular stirring; 50% volume of fresh enzymes was added for an additional 60-min period. The reaction was stopped with DMEM-5% FBS, and the cells were collected through nylon mesh, centrifuged twice at 300 g for 5 min at 4°C. Synovial cells were suspended in complete medium (DMEM supplemented with 10% FBS, 2 mm glutamine, penicillin-streptomycin, and fungizone) and plated onto 75-cm2 culture flasks. The medium was changed once or twice a week until confluence, and passages were done at a ratio of 1 : 2 or 1 : 3 after trypsinization. After 2–3 passages, the cells had a typical homogenous fibroblast appearance by phase-contrast microscopy. Culture medium, i.e. supernatant, was collected and kept at − 80°C. In kinetic studies, passage 5–7 synoviocytes were seeded onto 24-well plates at a cell density of 3–4 × 104, in 500 µl DMEM with or without FBS. Supernatants were collected at various times, and cell counts were determined in Trypan blue after detachment of the cells.
Synovial fibroblast characterization
Synovial fibroblasts were identified based on their typical morphology by phase-contrast light microscopy and by indirect immunofluorescence using a monoclonal antibody directed against prolyl hydroxylase which is specifically expressed by fibroblast-like cells in the synovium (5B5, Dako, Trappes, France). Fluorescent staining was observed in 90% of the permeabilized cells.
Angiogenin measurement
Angiogenin levels in plasma, SF, and cell-conditioned media were determined by the specific radioimmunoassay (RIA) described previously [35]. Human recombinant Met-(−1) angiogenin was provided by Rhône-Poulenc Rorer (Vitry, France) and wild-type human recombinant <Glu-1 angiogenin was a gift from R. Shapiro (Harvard Medical School, Boston, MA, USA). Angiogenin was labelled with 125I using the chloramine T method, as previously described [36]. The assay using a protein A-purified rabbit polyclonal antibody against human Met-(−1) angiogenin, produced by Rhône-Poulenc Rorer (Vitry, France), was species specific. The detection limit for both recombinant Met-(−1) angiogenin and <Glu-1 angiogenin was 10–20 pg/ml with an ED50 at 100–200 pg/ml. Triplicate determinations were repeated at least twice for most plasma and cell supernatants to four times for SF. They were performed and analysed without knowledge of the patient's diagnosis. Results were expressed as mean ± standard deviation in pg/ml or ng/ml.
Angiogenin was also measured in plasma, SF, and cell-conditioned media using a commercially available ELISA (R & D Systems, Abingdon, UK). Similar results were obtained with the two methods (data not shown).
Detection of IL-1β and TNF-α in monocyte supernatants
To check cell viability, IL-1β and TNF-α were measured in the monocyte supernatants using an ELISA (R & D Systems, Abingdon, UK). Cytokine production was stimulated by LPS and MDP, as described above.
Statistical analysis
Data are expressed as the median and range for SF and mean ± SD for plasma. Comparisons of median SF angiogenin concentrations between patient groups were made by Kruskal–Wallis nonparametric anova followed by the Mann–Whitney rank sum test for comparisons between groups. Mean plasma angiogenin concentrations were compared using the Student t-test. Values of p under 0·05 were considered significant.
Results
Angiogenin in plasma
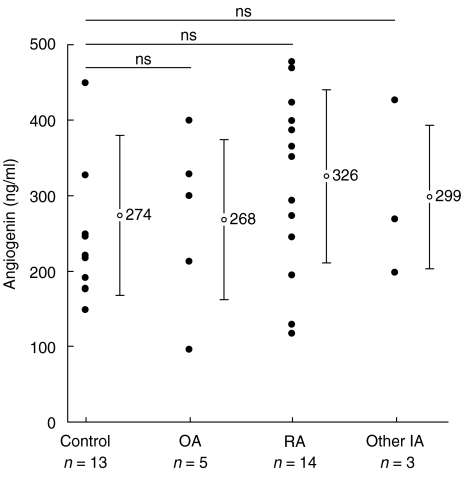
Plasma angiogenin concentrations did not differ significantly between healthy volunteers and patients with OA, RA, or IA. They ranged from 96 to 478 ng/ml (Fig. 1). No statistically significant difference was found when mean concentrations were compared in controls, patients with inflammatory disease, and patients with noninflammatory disease.
Fig. 1.
Plasma angiogenin concentrations from patients with joint disease. Plasma angiogenin levels were assessed by RIA. OA, osteoarthritis; RA, rheumatoid arthritis; other IA, other inflammatory arthritides (psoriatic arthritis and HLA-B27-related oligoarthritis). • represents an individual value; ○ the mean value (ng/ml) in each disease category. The vertical bar represents the standard deviation.
Angiogenin in synovial fluid
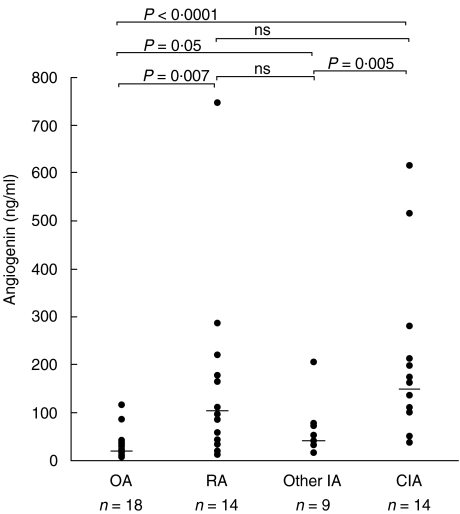
Angiogenin was detected in all SF samples tested. By anova, differences in SF angiogenin concentrations between disease groups were highly significant (P < 0·0001). Angiogenin levels in SF were higher (P < 0·0001) in the patients with inflammatory disease (median, 103 ng/ml; range, 13–748; n = 37) than in those with OA (median, 20 ng/ml; range, 8–116; n = 18) (Fig. 2). Median angiogenin concentrations in SF were similar in the three subgroups of patients with inflammatory disease: RA (median, 104 ng/ml; range 13–748, n = 14), CIA (median, 149 ng/ml; range, 37–616, n = 14), and other chronic IA (median, 42 ng/ml; range, 15–205; n = 9). SF angiogenin concentrations were significantly higher in patients with inflammatory diseases than in patients with OA (RA versus OA, P = 0·0007; CIA versus OA, p < 0·0001; and other IA versus OA, P = 0·05). Moreover the highest angiogenin levels in SF were achieved in patients with active RA or acute gout. Angiogenin levels were not correlated with the total cell count, lymphocyte count, or polymorphonuclear cell count in SF. Interestingly, serial angiogenin levels in SF from a patient with acute gout decreased from 616 to 164 ng/ml in parallel with resolution of the arthritis within 7 days under oral colchicine therapy. Moreover, in three patients with RA considered to have been in remission for several months, noninflammatory knee effusion developed as a manifestation of secondary OA. In this subset of RA patients, SF cell counts were lower than 1000 cells/mm3, respectively, 30, 560, and 650 cells/mm3 and SF angiogenin levels ranged from 15 to 111 ng/ml, which was similar to the 8–116 ng/ml range in patients with primary OA (P = 0·22, nonparametric test). No paired plasma and SF samples were available.
Fig. 2.
Angiogenin concentrations in synovial fluid (SF) from patients with joint disease.SF angiogenin concentrations were assessed by RIA. OA, osteoarthritis; RA, rheumatoid arthritis; other IA, other inflammatory arthritides (psoriatic arthritis and HLA-B27-related oligoarthritis); and CIA, crystal-induced arthritis (gout and pseudo-gout). • represents an individual value. The horizontal bar indicates the median value. Comparisons were made using a nonparametric test.
Cellular source of angiogenin
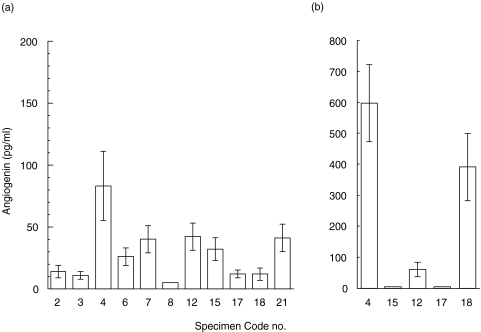
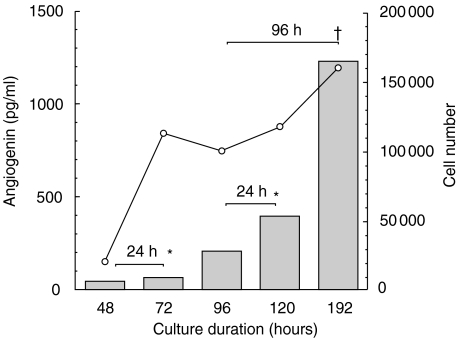
Angiogenin was not detected in supernatants (<200 pg/ml, n = 22) from RA or control monocytes cultured for 24 h with or without stimulation by LPS (n = 5) or MDP (n = 6), both of which are bacterial compounds (data not shown). However, IL-1β and TNF-α were detected and increased significantly after LPS or MDP stimulation for 24 h, confirming the viability of the cultured monocytes and the validity of the assay (data not shown). In contrast, angiogenin immunoreactivity was detected in conditioned media of synovial fibroblasts isolated from both active and chronic RA lesions and from OA joints (Fig. 3). No synovial material from crystal-induced arthritis was available to compare the levels of synthesis. Figure 4 shows a representative time-course of angiogenin release in supernatants (n = 2) by synovial fibroblasts relative to cell density and cell culture duration. When calculated, cumulative angiogenin production reached 1·18 ng/106 cells/day.
Fig. 3.
Release of angiogenin protein by cultured synovial fibroblastsConditioned media were collected from synovial fibroblasts cultured in 75 cm2-flasks in complete medium for 3–5 days, and angiogenin concentrations were determined as described in Methods. Each bar represents production by cultured cells from different synovial tissue specimens grown at (a) passage 0 and (b) passage 1, respectively. The numbers indicate the code for each specimen; nos. 12, 15, and 17 were from OA joints and all other specimens were from RA synovitis.
Fig. 4.
Release of angiogenin protein by cultured synovial fibroblasts relative to cell growth. As a representative experiment, passage 5 synovial fibroblasts obtained from an RA patient (synovium no. 23) were cultured at 3 × 104 cell density in DMEM medium with 10% FBS, in 24-well plates. Mean cell counts (duplicate wells) were determined (○). Medium was changed on days 2 and 4. Conditioned media were collected as indicated and assayed for angiogenin (░). *Angiogenin levels on days 3 and 5 represent the 24-h cumulative angiogenin productions (days 2–3 and days 4–5, respectively). †The angiogenin level on day 8 represents the 96-h cumulative angiogenin production (days 4–8).
Discussion
In this study, we found that angiogenin was present at similar concentrations in plasma from both healthy subjects and rheumatic patients in the same range as those previously reported [35,37]. In addition, no difference in plasma angiogenin levels was found between patients with inflammatory joint disease and those with OA. In SF, angiogenin was found in a wide range of concentrations. Most importantly, a significant difference in SF angiogenin concentrations was found between inflammatory and noninflammatory joint diseases. SF angiogenin levels were highest in patients with chronic synovitis characterized by prominent angiogenesis, such as RA. Moreover, SF obtained from three patients with quiescent RA and secondary OA contained angiogenin levels similar to those observed in primary OA. Conversely, high SF angiogenin levels were found in patients with acute crystal-induced inflammation, namely, gout attacks. In addition, in one patient with gouty arthritis, SF angiogenin levels decreased with the resolution of acute inflammation, suggesting that this molecule may either reflect or play a role in monosodium urate crystal-induced inflammation. Taken together, these findings suggest a local role for angiogenin in joints exhibiting inflammation.
We addressed the cellular origin of angiogenin in SF. Macrophages are key angiogenesis effector cells in inflammatory and tumoral angiogenesis [38], and their presence is associated with local secretion of many pro-angiogenic factors [39]. In human colorectal cancer, the intensity of angiogenin detection has been shown to correlate with microvessel density and focal macrophage infiltration [40]. We therefore looked for angiogenin in serum-free media conditioned for 24h by adherent peripheral blood monocytes. No angiogenin was released by unstimulated monocytes or by LPS- or MDP- stimulated monocytes (< 200 pg/ml), whereas the cytokines IL-1β and TNF-α were readily expressed by these cells. These results are consistent with reports that blood leucocytes express the angiogenin protein and its mRNA at low levels [35, 41, 42]. Hosaka et al. have shown that synovial lining cells, vascular smooth muscle cells, endothelial cells and macrophages in synovial tissue were immunopositive for angiogenin, raising the possibility that cells from the monocyte/macrophage lineage may modulate angiogenin expression [20]. However, a possible contribution of macrophages to significant angiogenin synthesis in specific articular diseases remains to be demonstrated.
Local production of angiogenin is strongly suggested by our finding that angiogenin is released in large amounts by synovial fibroblasts from joints with active or chronic synovitis (Figs 3, 4). All primary cell cultures expressed significant amounts of angiogenin. In agreement with data from Hosaka et al. [20], angiogenin was not detected in supernatants from 24h fibroblast cultures. Angiogenin protein became detectable in cell culture media only after at least 48 h of culturing. As previously described for endothelial cells [35], angiogenin release by synovial fibroblasts increased with cell density, suggesting that excessive proliferation of synovial cells in inflammatory joint disease may result in accumulation of the angiogenic protein.
A potential role for angiogenin in inflammatory conditions is supported by its angiogenic activity. Whether angiogenin induces and/or modulates angiogenesis remains to be determined. Given that angiogenin has been shown to inhibit polymorphonuclear leucocyte degranulation in vitro [43] and to display immunosuppressive activity in vitro [44], it may also act as a regulatory agent. Regulatory cytokines such as IL-6, a major inducer of acute-phase proteins, stimulate the synthesis and secretion of angiogenin protein and also increase the amount of angiogenin mRNA in human HepG2 cells within 24 h [32]. In addition, hypoxia, a component of chronic synovial inflammation, has been shown to stimulate angiogenin mRNA expression and protein release [45,46]. Therefore, angiogenin could be involved in the host response to inflammatory processes.
Acknowledgments
We thank Dr Thé N’Guyen for copioneering the RIA experiments; Dr Robert Shapiro and Prof Bert L. Vallee (Boston, MA) for providing the human recombinant <Glu-1 angiogenin; and Prof Daniel Goutallier, Prof Claude Kénési, and Dr Christophe Piat (Orthopaedics Departments, Henri-Mondor Teaching Hospital (AP-HP), Créteil) for providing the synovial tissue samples. Human recombinant Met-(−1) angiogenin and antibodies against it were produced at the Biotechnology Institute, Vitry, France (Rhône-Poulenc Rorer).
This work was supported in part by the ‘Association pour la Recherche sur la Polyarthrite’ (ARP), the ‘Direction de la Recherche Clinique’ (Assistance Publique-Hôpitaux de Paris, AP-HP), the ‘Association pour la Recherche en Pathologie Synoviale’ (ARPS), the ‘Société Française de Rhumatologie’ (SFR), and the ‘Association de la Recherche sur le Cancer’ (ARC).
References
- 1.Harris ED., Jr Rheumatoid arthritis. Pathophysiology and implications for therapy. N Engl J Med. 1990;322:1277–89. doi: 10.1056/NEJM199005033221805. [DOI] [PubMed] [Google Scholar]
- 2.Goldenberg DL, Cohen AS. Synovial membrane histopathology in the differential diagnosis of rheumatoid arthritis, gout, pseudogout, systemic lupus erythematosus, infectious arthritis and degenerative joint disease. Medicine (Baltimore) 1978;57:239–52. doi: 10.1097/00005792-197805000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Brown RA, Weiss JB. Neovascularisation and its role in the osteoarthritic process. Ann Rheum Dis. 1988;47:881–5. doi: 10.1136/ard.47.11.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walsh DA. Angiogenesis and arthritis. Rheumatology. 1999;38:103–12. doi: 10.1093/rheumatology/38.2.103. [DOI] [PubMed] [Google Scholar]
- 5.Koch AE. The role of angiogenesis in rheumatoid arthritis: recent developments. Ann Rheum Dis. 2000;59:i65–i71. doi: 10.1136/ard.59.suppl_1.i65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Folkman J, Klagsbrun M. Angiogenic factors. Science. 1987;235:442–77. doi: 10.1126/science.2432664. [DOI] [PubMed] [Google Scholar]
- 7.Folkman J. Angiogenesis in cancer, vascular, rheumatoid and other disease. Nature Med. 1995;1:27–31. doi: 10.1038/nm0195-27. [DOI] [PubMed] [Google Scholar]
- 8.Fontana A, Hengartner H, Weber E, Fehr K, Grob PJ, Cohen G. Interleukin 1 activity in the synovial fluid of patients with rheumatoid arthritis. Rheumatol Int. 1982;2:49–53. doi: 10.1007/BF00541245. [DOI] [PubMed] [Google Scholar]
- 9.Al-Balaghi S, Strom H, Moller E. B cell differentiation factor in synovial fluid of patients with rheumatoid arthritis. Immunol Rev. 1984;78:7–23. doi: 10.1111/j.1600-065x.1984.tb00474.x. [DOI] [PubMed] [Google Scholar]
- 10.Seitz M, Dewald B, Ceska M, Gerber N, Baggiolini M. Interleukin-8 in inflammatory rheumatic diseases. Synovial fluid levels, relation to rheumatoid factors, production by mononuclear cells, and effects of gold sodium thiomalate and methotrexate. Rheumatol Int. 1992;12:159–64. doi: 10.1007/BF00274936. [DOI] [PubMed] [Google Scholar]
- 11.Husby G, Williams RC., Jr Synovial localization of tumor necrosis factor in patients with rheumatoid arthritis. J Autoimmun. 1988;1:363–71. doi: 10.1016/0896-8411(88)90006-6. [DOI] [PubMed] [Google Scholar]
- 12.Sano H, Forough R, Maier JA, Case JP, Jackson A, Engleka K, Maciag T, Wilder RL. Detection of high levels of heparin binding growth factor-1 (acidic fibroblast growth factor) in inflammatory arthritic joints. J Cell Biol. 1990;110:1417–26. doi: 10.1083/jcb.110.4.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Remmers EF, Sano H, Wilder RL. Platelet-derived growth factors and heparin-binding (fibroblast) growth factors in the synovial tissue pathology of rheumatoid arthritis. Semin Arthritis Rheum. 1991;21:191–9. doi: 10.1016/0049-0172(91)90009-o. [DOI] [PubMed] [Google Scholar]
- 14.Koch AE, Halloran MM, Hosaka S, et al. Hepatocyte growth factor. A cytokine mediating endothelial migration in inflammatory arthritis. Arthritis Rheum. 1996;39:1566–75. doi: 10.1002/art.1780390917. [DOI] [PubMed] [Google Scholar]
- 15.Nagashima M, Hasegawa J, Kato K, Yamazaki J, Nishigai K, Ishiwata T, Asano G, Yoshino S. Hepatocyte growth factor (HGF), HGF activator, and c-Met in synovial tissues in rheumatoid arthritis and osteoarthritis. J Rheumatol. 2001;28:1772–8. [PubMed] [Google Scholar]
- 16.Thornton SC, Por SB, Penny R, Richter M, Shelley L, Breit SN. Identification of the major fibroblast growth factors released spontaneously in inflammatory arthritis as platelet derived growth factor and tumour necrosis factor-alpha. Clin Exp Immunol. 1991;86:79–86. doi: 10.1111/j.1365-2249.1991.tb05777.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fava R, Olsen N, Keski-Oja J, Moses H, Pincus T. Active and latent forms of transforming growth factor beta activity in synovial effusions. J Exp Med. 1989;169:291–6. doi: 10.1084/jem.169.1.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Koch AE, Harlow LA, Haines GK, Amento EP, Unemori EN, Wong WL, Pope RM, Ferrara N. Vascular endothelial growth factor. A cytokine modulating endothelial function in rheumatoid arthritis. J Immunol. 1994;152:4149–56. [PubMed] [Google Scholar]
- 19.Nagashima M, Yoshino S, Ishiwata T, Asano G. Role of vascular endothelial growth factor in angiogenesis of rheumatoid arthritis. J Rheumatol. 1995;22:1624–30. [PubMed] [Google Scholar]
- 20.Hosaka S, Shah MR, Barquin N, Haines GK, Koch AE. Expression of basic fibroblast growth factor and angiogenin in arthritis. Pathobiology. 1995;63:249–56. doi: 10.1159/000163957. [DOI] [PubMed] [Google Scholar]
- 21.Ikeda M, Hosoda Y, Hirose S, Okada Y, Ikeda E. Expression of vascular endothelial growth factor isoforms and their receptors Flt-1, KDR, and neuropilin-1 in synovial tissues of rheumatoid arthritis. J Pathol. 2000;191:426–33. doi: 10.1002/1096-9896(2000)9999:9999<::AID-PATH649>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 22.Uchida T, Nakashima M, Hirota Y, Miyazaki Y, Tsukazaki T, Shindo H. Immunohistochemical localisation of protein tyrosine kinase receptors Tie-1 and Tie-2 in synovial tissue of rheumatoid arthritis: correlation with angiogenesis and synovial proliferation. Ann Rheum Dis. 2000;59:607–14. doi: 10.1136/ard.59.8.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Badet J. Angiogenin, a potent mediator of angiogenesis: Biological, biochemical and structural properties. Pathologie Biologie. 1999;47:345–51. [PubMed] [Google Scholar]
- 24.Fett JW, Strydom DJ, Lobb RR, Alderman EM, Bethune JL, Riordan JF, Vallee BL. Isolation and characterization of angiogenin, an angiogenic protein from human carcinoma cells. Biochemistry. 1985;24:5480–6. doi: 10.1021/bi00341a030. [DOI] [PubMed] [Google Scholar]
- 25.King TV, Vallee BL. Neovascularisation of the meniscus with angiogenin. An experimental study in rabbits. J Bone Joint Surg (Br) 1991;73-B:587–90. doi: 10.1302/0301-620X.73B4.1712788. [DOI] [PubMed] [Google Scholar]
- 26.Soncin F, Strydom DJ, Shapiro R. Interaction of heparin with human angiogenin. J Biol Chem. 1997;272:9818–24. doi: 10.1074/jbc.272.15.9818. [DOI] [PubMed] [Google Scholar]
- 27.Shapiro R, Riordan JF, Vallee BL. Characteristic ribonucleolytic activity of human angiogenin. Biochemistry. 1986;25:3527–32. doi: 10.1021/bi00360a008. [DOI] [PubMed] [Google Scholar]
- 28.Olson KA, Fett JW, French TC, Key ME, Vallee BL. Angiogenin antagonists prevent tumor growth in vivo. Proc Natl Acad Sci USA. 1995;92:442–6. doi: 10.1073/pnas.92.2.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Olson KA, Byers HR, Key ME, Fett JW. Prevention of human prostate tumor metastasis in athymic mice by antisense targeting of human angiogenin. Clin Cancer Res. 2001;7:3598–605. [PubMed] [Google Scholar]
- 30.Olson KA, Byers HR, Key ME, Fett JW. Inhibition of prostate carcinoma establishment and metastatic growth in mice by an antiangiogenin monoclonal antibody. Int J Cancer. 2002;98:923–9. doi: 10.1002/ijc.10282. [DOI] [PubMed] [Google Scholar]
- 31.Olson KA, Verselis SJ, Fett JW. Angiogenin is regulated in vivo as an acute phase protein. Biochem Biophys Res Commun. 1998;242:480–3. doi: 10.1006/bbrc.1997.7990. [DOI] [PubMed] [Google Scholar]
- 32.Verselis SJ, Olson KA, Fett JW. Regulation of angiogenin expression in human HepG2 hepatoma cells by mediators of the acute-phase response. Biochem Biophys Res Commun. 1999;259:178–84. doi: 10.1006/bbrc.1999.0744. [DOI] [PubMed] [Google Scholar]
- 33.Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–24. doi: 10.1002/art.1780310302. [DOI] [PubMed] [Google Scholar]
- 34.Lioté F, Boval-Boizard B, Weill D, Kuntz D, Wautier JL. Blood monocyte activation in rheumatoid arthritis. increased monocyte adhesiveness, integrin expression, and cytokine release. Clin Exp Immunol. 1996;106:13–19. doi: 10.1046/j.1365-2249.1996.d01-820.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moenner M, Gusse M, Hatzi E, Badet J. The widespread expression of angiogenin in different human cells suggests a biological function not only related to angiogenesis. Eur J Biochem. 1994;226:483–90. doi: 10.1111/j.1432-1033.1994.tb20073.x. [DOI] [PubMed] [Google Scholar]
- 36.Hatzi E, Badet J. Expression of receptors for human angiogenin in vascular smooth muscle cells. Eur J Biochem. 1999;260:825–32. doi: 10.1046/j.1432-1327.1999.00222.x. [DOI] [PubMed] [Google Scholar]
- 37.Bläser J, Triebel S, Kopp C, Tschesche H. A highly sensitive immunoenzymometric assay for the determination of angiogenin. Eur J Clin Chem Clin Biochem. 1993;31:513–16. doi: 10.1515/cclm.1993.31.8.513. [DOI] [PubMed] [Google Scholar]
- 38.Polverini PJ. How the extracellular matrix and macrophages contribute to angiogenesis-dependent diseases. Eur J Cancer. 1996;32A:2430–7. doi: 10.1016/s0959-8049(96)00386-3. [DOI] [PubMed] [Google Scholar]
- 39.Sunderkötter C, Steinbrink K, Goebeler M, Bhardwaj R, Sorg C. Macrophages and angiogenesis. J Leukocyte Biol. 1994;55:410–22. doi: 10.1002/jlb.55.3.410. [DOI] [PubMed] [Google Scholar]
- 40.Etoh T, Shibuta K, Barnard GF, Kitano S, Mori M. Angiogenin expression in human colorectal cancer. The role of focal macrophage infiltration. Clin Cancer Res. 2000;6:3545–51. [PubMed] [Google Scholar]
- 41.Rybak SM, Fett JW, Yao Q-Z, Vallee BL. Angiogenin mRNA in human tumor and normal cells. Biochem Biophys Res Commun. 1987;146:1240–8. doi: 10.1016/0006-291x(87)90781-9. [DOI] [PubMed] [Google Scholar]
- 42.Egesten A, Dyer KD, Batten D, Domachowske JB, Rosenberg HF. Ribonucleases and host defense: identification, localization and gene expression in adherent monocytes in vitro. Biochem Biophys Acta. 1997;1358:255–60. doi: 10.1016/s0167-4889(97)00081-5. [DOI] [PubMed] [Google Scholar]
- 43.Tschesche H, Kopp C, Hörl WH, Hempelmann U. Inhibition of degranulation of polymorphonuclear leukocytes by angiogenin and its tryptic fragment. J Biol Chem. 1994;269:30274–80. [PubMed] [Google Scholar]
- 44.Matousek J, Soucek J, Riha J, Zankel TR, Benner SA. Immunosuppressive activity of angiogenin in comparison with bovine seminal ribonuclease and pancreatic ribonuclease. Comp Biochem Physiol. 1995;112B:235–41. doi: 10.1016/0305-0491(95)00075-5. [DOI] [PubMed] [Google Scholar]
- 45.Hartmann A, Kunz M, Köstlin S, Gillitzer R, Toksoy A, Bröcker E-B, Klein CE. Hypoxia-induced up-regulation of angiogenin in human malignant melanoma. Cancer Res. 1999;59:1578–83. [PubMed] [Google Scholar]
- 46.Koga K, Osuga Y, Tsutsumi O, et al. Evidence for the presence of angiogenin in human follicular fluid and the up-regulation of its production by human chorionic gonadotropin and hypoxia. J Clin Endocrinol Metab. 2000;85:3352–5. doi: 10.1210/jcem.85.9.6837. [DOI] [PubMed] [Google Scholar]