Abstract
High levels of antibodies against the C-terminus of the Trypanosoma cruzi TcP2β ribosomal protein, defined by the peptide EEEDDDMGFGLFD, named R13, have been measured in sera from patients with chronic Chagas’ Heart Disease (cChHD). These antibodies also recognize an epitope on the second extracellular loop of the β1-adrenergic receptor, inducing a functional response on cardiomyocytes. The aim of this study was to gain novel insights into the structural basis of this cross-reactivity as well as to evaluate the origin of anti-M2- cholinergic receptor antibodies, which are also commonly found in cChHD patients. To address these questions we immunopurified anti-R13 antibodies and studied the structural requirements of epitope recognition. Results showed that the immunopurified antibodies recognized a conformation of R13 in which the third Glu residue was essential for binding, explaining their low affinity for the mammalian homologue (peptide H13: EESDDDMGFGLFD). Alanine mutation scanning showed individual variations in epitope recognition in each of the studied patients. The importance of a negatively charged residue at position 3 for the recognition of anti-R13 antibodies was further confirmed by competition experiments using a Ser3-phosphorylated H13 analogue, which had 10 times more affinity for the anti-R13 antibody than the native H13 peptide. Moreover, anti-R13 antibodies stimulated either the β1-adrenergic or the M2-cholinergic receptor, in strict agreement with the functional properties of the IgG fractions from which they derived, demonstrating that the same parasite antigen may generate antibody specificities with different functional properties. This may be a clue to explain the high variability of electrophysiological disturbances found in cChHD.
Keywords: Chronic Chagas’ heart disease, β1-adrenergic receptor, M2-cholinergic receptor, Trypanosoma cruzi, ribosomal P proteins
INTRODUCTION
Chronic Chagas’ Heart Disease (cChHD) is caused by the haemoflagellate Trypanosoma cruzi and is a major health problem in Latin America. It is the most common cause of cardiomyopathy in South and Central America, and in endemic regions it constitutes the leading cause of cardiovascular death among patients between the ages of 30 and 50 years. Amongst other clinical features, cChHD is an arrhythmogenic cardiomyopathy, including a high prevalence of right bundle branch block, left anterior hemiblock, sinus node dysfunction and complex supra-ventricular arrhythmias [1]. Not infrequently, tachy- and bradyarrhythmias coexist in the same patient [2]. Sudden cardiac death due to sustained ventricular tachyarrhythmia is exceedingly common [3].
Although the pathogenesis of cChHD still remains unclear, results from several studies suggest a link between arrhythmias and circulating antibodies with agonist-like properties on cardiac receptors. Antibodies that recognize and stimulate β1- and β2-adrenergic receptors (β1/β2-AR) and M2-cholinergic receptors (M2-ChR) have been extensively reported to exist in cChHD patients [4–6]. They exert functional alterations on the beating rate of cultured rat cardiomyocytes [7,8], on second messenger levels [7,9,10], and are able to induce conduction block on isolated whole rabbit hearts [11]. Different experimental observations elucidated the nature of the antiheart receptor specificities generated in cChHD [8,12]. It has been demonstrated that antibodies directed against the ribosomal P2β protein of T. cruzi (TcP2β) are able to cross-react with and stimulate the β1-AR. This is attributed to the highly antigenic acidic epitope present on the C-terminal end of the parasite ribosomal protein, named R13 (EEEDDDMGFGLFD), which bears similarity to an acidic motif (AESDE) on the second extracellular loop of the receptor.
Mice immunized with the recombinant TcP2β protein that raise a strong response against R13, also develop a lethal supra-ventricular tachycardia, strongly suggesting that the high anti-R13 antibody levels are responsible for the sustained β-adrenergic stimulation of the heart [13]. In addition, the β1-AR stimulatory effect of the anti-R13 antibodies has been further confirmed by the generation of an anti-R13 monoclonal antibody, mAb17·2, with an exclusive stimulatory activity on this receptor subtype [14]. In contradiction with these observations, we have detected cChHD patients with sick sinus syndrome and high anti-R13 antibody levels whose total IgG fraction stimulated the M2-ChR, decreasing the beating rate of cardiomyocytes [6,15].
This study was designed to evaluate the prevalence and fine-specificities of circulating anti-R13 antibodies in cChHD patients with diverse arrhythmogenic anomalies and to study the eventual contribution of these antibodies to the functional effect displayed by the total IgG fraction from patients with cChHD.
MATERIALS AND METHODS
Human sera
Sera were obtained from 123 patients with cChHD who came from the same endemic region located in the north-west of Argentina. The patients underwent a complete clinical and cardiologic examination, an ECG at rest, an exercise stress test, a 24-h ECG Holter monitoring, and a B-mode echocardiogram at the Cardiovascular Division, Ramos Mejia Hospital (Buenos Aires). Ventricular arrhythmias (VA) and sinus node dysfunction (SND) were diagnosed as reported previously [7]. Sera from 103 patients with other non-Chagas cardiomyopathies (idiopathic dilated cardiomyopathy, ischaemic heart disease, severe left ventricular dysfunction, diagnosed according to reported criteria [16]) and 17 healthy individuals were used as negative controls. A subgroup of patients was also classified according to the severity of heart disease in: Chagas Group I (CH I: severe cardiomyopathy, high ventricular dilation, n = 15), Chagas Group III (CHIII: purely electrical arrhythmias, n = 6) and Chagas Group IV (preclinical, with no ECG disturbances, n = 3). No patient could be ascribed to CH group II (moderate heart dilation, with or without arrhythmias). After clinical evaluation, blood samples were drawn, and sera were obtained and coded.
IgG fractionation
The IgG fractions of the sera were prepared by a dilution of 1/5 of the serum in PBS and precipitation at 40% ammonium sulphate saturation. The precipitate was re-dissolved in PBS and dialysed exhaustively against PBS at 4°C.
Synthetic peptides
Peptides were synthesized using the Fmoc technique with solid-phase automatic synthesis. Their purity was assessed by High Performance Liquid Chromatography (HPLC) and identified by mass spectrometry. Peptide R13 (EEEDDDMGFGLFD) and R7 (MGFGLFD) correspond to the C-terminal region (residues 107–119 and 113–119, respectively) of the T. cruzi ribosomal TcP2β protein [17]. Peptide H13 and its phospho-serine analogue pH13 correspond to the C-terminal region (residues 102–115) of the human ribosomal P protein [18].
Affinity purification of anti R13 antibodies
E. coli DH5α strain aliquots were transformed with 1 ng pGex plasmid encoding for the TcP2β protein [19] following a purification method described in Levitus et al. [20]. The transformed cells were plated on LB-agar with Ampicillin (100 µg/ml) and incubated ON at 37°C. On the next day, circular nitrocellulose Hybond C membranes (Amersham Biosciences, London, UK) prewetted in 10 mm IPTG (isopropyl-β-thiogalactoside; Sigma Chemical Co, St.Louis, MO, USA) were laid on the LB-agar dishes with densely grown colonies and incubated for 4 h on fresh LB-agar dishes for expression of the recombinant protein (GST-TcP2β). The cells were lysed on the membrane in a chloroform atmosphere and washed with PBS-Tween 0·1%. The membranes were blocked with PMT 5% (PBS containing 5% w/v of milk, 0·1% Tween-20) for one hour and then incubated overnight at 4°C with a dilution of 1/10 of the serum in PMT 3% to be immunopurified. After two 10 min washings with 150 mm NaCl-Tween 0·1% and three washings with PBS-Tween 0·1%, the specific antibodies were eluted with 3 ml of 0·2 m glycine at pH 2·7 rocking for 15 min at room temperature and immediately neutralized with 0·5 ml 1 m Tris pH 8. Purified antibodies were exhaustively dialysed against PBS at 4°C.
Functional assay on neonatal rat cardiomyocytes
Neonatal rat cardiomyocytes were prepared from hearts of 2–4 days old Sprague Dawley rats by a previously described method [21]. The cells were cultured as monolayers for 4 days at 37°C in DMEM-F12 medium (Life Technologies, Gaithersburg, MD, USA) supplemented with 10% heat-inactivated calf serum. The cardiomyocyte cultures were washed with fresh medium without serum and incubated for 60 min at 37°C. The flasks were transferred to the heatable stage of an inverted microscope, and the basal beating rate was determined inspecting 10 small circular fields and counting the number of contractions for 15 s. Basal beating rate was about 100 beats/min. Measurements were repeated after one hour of incubation with IgG fraction or immunopurified antibodies and subsequent addition of 10 µm atropine (Sigma) and 1 µm bisoprolol (Tocris Cookson Inc., Ellisville, MO, USA). This procedure was repeated for at least three identically treated culture flasks. The functional test was considered positive for the presence of antibodies activating the β1-AR if addition of IgG induced a statistically significant increase in the beating rate that was neutralized by bisoprolol. It was considered positive for the presence of antibodies stimulating the M2-ChR whenever addition of IgG led to a statistically significant reduction in the beating rate that was antagonized by atropine. The significant increase in the beating rate of cardiomyocytes after exposure to atropine that was in turn antagonized by bisoprolol, even in the absence of any initial significant change induced by the IgG alone, was interpreted as an indication of the presence of both types of antiautonomic receptor antibodies.
Western blots
Parasite extracts were obtained from T. cruzi epimastigote CL strain as previously described [22]. SDS-PAGE was performed using 15% polyacrylamide gels. Samples containing 50 µg of total parasites protein were applied to each well. Polypeptides were electrotransferred to a nitrocellulose membrane for 1 h at 80 V and immunodetection was performed with total IgG fractions at a dilution of 10 µg protein/ml, purified anti-R13 antibodies in a dilution of 1/3, or mAb17·2 at a concentration of 60 ng/ml in PMT 3% followed by incubation with peroxidase labelled goat antihuman IgG (Sigma) for 1 h and revealed by the chemiluminiscent ECL technique (Amersham Biosciences).
ELISA
Microwell plates (Nunc Maxi-Sorp F-96, Roskilde, Denmark) were coated overnight at 4°C with 1 µm of R13-BSA coupled synthetic peptide or 20 µg protein/ml of T. cruzi epimastigote lysate in 50 µl of 0·05 m carbonate buffer pH = 9·6. Plates were washed thrice with washing buffer (PBS containing 0·1% Tween-20) and then blocked with PMT 5% for 1 h at 37°C. Plates were rinsed with washing buffer and a 1/200 dilution in PMT 3% of the human sera were added directly to duplicate series of wells and incubated for 1 h at 37°C. Wells were washed thrice with washing buffer and 50 µl of peroxidase-labelled goat antihuman IgG diluted 1 : 3000 in PMT 1·5% was dispensed into each well. Enzyme activity was revealed with 100 µl of TMB substrate (3,3′,5,5′-tetramethylbenzidine dihydrocholoride (Sigma) at a concentration of 3 mg/ml in: 0·1 m citrate buffer pH 7, 2% DMSO, 1·8% glycerol, 0·01% H2O2) per well. The enzymatic reaction was stopped after 10 min by adding 50 µl of HCl 1 m and the optical densities were read at 450 nm with an automated plate reader (Molecular Devices, CA, USA). To determine cut off values, 20% of the wells on the plate were incubated with sera from healthy individuals. A ratio was calculated as ODs/ODHC+ 3SD (ODs = optical density of the unknown sample, ODHC = mean of healthy controls optical density, SD = standard deviation). Sera with ratio values above the cut off line (cut off: ODHC+ 3SD = 1) were considered positive for R13.
For inhibition experiments, affinity purified antibodies in an appropriate dilution (yielding an optical density of 0·7) were preincubated with peptide concentrations ranging between 0 and 20 µm for 1 h at room temperature under agitation and then added to the R13-BSA coated plate as described before. Inhibition constants were estimated as KI: 1/IC50 (m−1) [23]. Peptide R7 was used as a nonbinding control peptide to determine nonspecific competition.
Fine epitope mapping
The fine epitope mapping of the C-terminal region of TcP2β (R13) was performed with the SPOTs® technique (Genosys Biotechnologies Inc, UK). The membrane with a set of 14 peptides representing the R13 sequence and its alanine-replacement analogues was provided by the supplier. The R13 membrane was probed with a 1/10 dilution of the affinity purified anti-R13 antibodies and revealed as described previously [14]. The criterion to determine loss of binding after substitution of any given residue by alanine was the observation of more than 70% decrease in the chemiluminiscent signal at the corresponding spot position as determined by grey scale density measurement using the NIHimage software for Macintosh.
Statistics
For the determination of significant differences in antibody levels between the different groups (CH group I, III and IV), we grouped CH group III and group IV and compared this subgroup with CH group I using the nonparametric Wilcoxon unmatched pairs signed-ranks test.
For functional assays, differences of mean beating rates between treatments were determined using the paired Student's t-test.
RESULTS
Presence of functionally active antibodies in cChHD IgG fractions that stimulate the β1-AR and the M2-ChR
Figure 1a depicts the effect of IgG from patients with cChHD on beating cardiomyocytes compared to IgG from patients with non-Chagas cardiomyopathies. The beating rate was not affected by the addition of IgG from healthy individuals. The analysed cChHD IgG revealed a broad spectrum of chronotropic effects on the cells indicating the presence of antibodies stimulating both the β1-AR and/or the M2-ChR, as determined by subsequent addition of pharmacologically specific antagonists (data not shown). On the other hand, IgG isolated from patients with non-Chagas cardiomyopathies exclusively displayed a positive chronotropic effect, indicating the presence of antibodies that only stimulate the β1-AR.
Fig. 1.
(a) Functional effect on spontaneously beating rat cardiomyocytes of IgG fractions from cChHD (▪), patients with other non-Chagas cardiomyopathies ( ) and healthy individuals (□). Bars represent change in beating rate caused by addition of IgG fraction from each individual. All results represent one from at least three independent experiments. (b) Chronotropic effect of IgG fractions (▪) among the cChHD population. The specificity of the effect was studied by subsequent addition of the M2-ChR antagonist atropine (□) and the β1-AR antagonist bisoprolol (
) and healthy individuals (□). Bars represent change in beating rate caused by addition of IgG fraction from each individual. All results represent one from at least three independent experiments. (b) Chronotropic effect of IgG fractions (▪) among the cChHD population. The specificity of the effect was studied by subsequent addition of the M2-ChR antagonist atropine (□) and the β1-AR antagonist bisoprolol ( ).VA, Ventricular arrhythmias; SND, Sinus node dysfunction; HC, Healthy Controls.
).VA, Ventricular arrhythmias; SND, Sinus node dysfunction; HC, Healthy Controls.
To further investigate the functional variability of IgG among cChHD patients, we evaluated the presence of antiautonomic receptor antibodies in four groups of patients with different types of arrhythmias: (1) ventricular arrhythmia (VA) (2) sinus node dysfunction (SND) (3) both VA and SND, and (4) neither VA nor SND (Fig. 1b). IgG fractions from patients with VA exerted in nine out of 12 cases, 75%, a positive chronotropic effect on cardiomyocytes which was, at least in part, antagonized by the β1-AR specific antagonist bisoprolol, indicating the presence of antiβ1-AR antibody specificities. Forty-two percent of the patients with SND presented functional recognition of the M2-ChR. Only one patient with SND presented antiβ1AR antibodies, whereas two other patients showed IgG fractions that stimulated both type of receptors. Sixty-six percent of the patients, four out of six, with both VA and SND possess both antiβ1-AR and M2-ChR antibodies. Only one out of the five patients with neither VA nor SND exhibited antibodies with a functional effect.
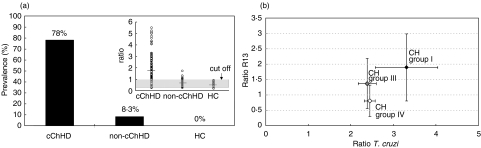
Prevalence of antibodies reacting with the C-terminal region of TcP2β (peptide R13) in cChHD patients and affinity purification of specific anti-R13 antibodies
Molecular expression cloning techniques revealed that patients with cChHD presented a strong humoral response against the C-terminal region of the T. cruzi ribosomal TcP2β protein, defined by the epitope represented by the R13 peptide [24]. Further studies confirmed that (a) the anti-TcP2β reactivity in cChHD was strictly restricted to the recognition of the R13 epitope [12,13,25] indicating that the R13 peptide can be used to monitor the humoral anti-TcP2β response in cChHD, and (b) that polyclonal anti-R13 antibodies from patients, as well as anti-R13 monoclonal antibodies exert a functional effect on cardiomyocytes [12,14]. In consequence, to assess the contribution of anti-R13 antibodies to the functional effect of total IgG fractions from patients with cChHD on cardiac receptors, we first undertook the screening of a large cohort of cChHD patients as to their anti-R13 antibody levels. Serum samples from 123 patients with cChHD were tested by ELISA using the R13 peptide as reactive reagent. Sera from patients with non-Chagas cardiomyopathies and healthy individuals were also included in this study. As shown in Fig. 2a, 78% of the patients with a cChHD displayed high prevalence of anti-R13 antibodies. Notably, high levels of anti-R13 antibodies correlated with the severity of heart disease as shown in Fig. 2b. Patients from CH group I presented significantly higher anti-R13 and anti-T. cruzi antibody levels compared to cChHD patients with mild cardiomyopathy and preclinical cardiomyopathies (CH group III and IV, P < 0·05). To further analyse the functional effects of IgG fractions and anti-R13 antibodies, we immunopurified anti-R13 antibodies from eight cChHD patients with the highest anti-R13 antibody levels (see insert of Fig. 2a).
Fig. 2.
(a) Prevalence of anti-R13 antibodies as determined by ELISA in a cChHD population (n = 123), compared to circulating antibody levels in sera from patients with other non-Chagas cardiomyopathies (n = 103) and healthy individuals (n = 17). Insert: Ratio values distribution of antibody levels among the studied groups (for details see Materials and methods). (b) Correlation between severity of heart disease and circulating antibody levels against R13 and T. cruzi epimastigote lysate. Rhomboids represent mean ratio values for each studied group: CH group I (n = 15): severe chronic Chagas cardiomyopathy (♦), CH group III (n = 6): mild chronic Chagas cardiomyopathy ( ), and CH group IV (n = 3): preclinical chronic Chagas cardiomyopathy with no ECG disturbances (e). Error bars represent standard deviation. Significance of the differences in mean antibody levels between CH group I and CH groups III + IV were determined applying the Wilcoxon test (P < 0·05).
), and CH group IV (n = 3): preclinical chronic Chagas cardiomyopathy with no ECG disturbances (e). Error bars represent standard deviation. Significance of the differences in mean antibody levels between CH group I and CH groups III + IV were determined applying the Wilcoxon test (P < 0·05).
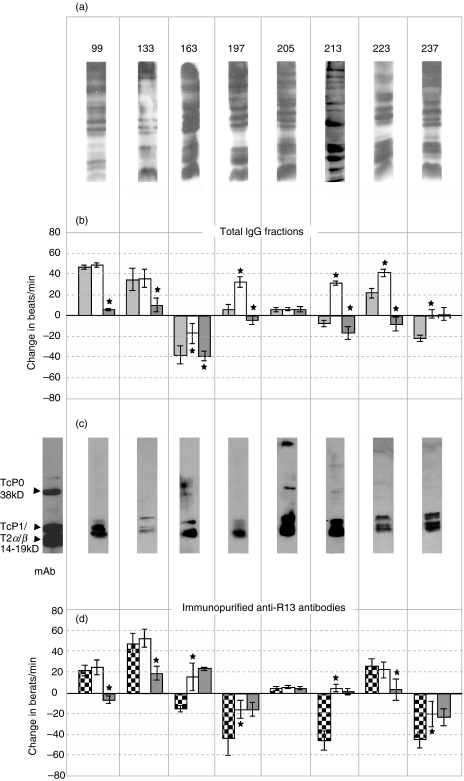
Functional activity of total IgG fractions compared to immunopurified anti-R13 antibodies
The functional effect of different IgG fractions from the eight selected patients was evaluated on neonatal rat cardiomyocytes. Total IgG fractions that reacted with a broad range of T. cruzi proteins as determined by Western blots (Fig. 3a) revealed three patterns of functional reactivity (Fig. 3b) namely IgG with:
an exclusive β1-AR stimulating effect (patients 99, 133);
an exclusive M2-ChR stimulating effect (patients 163, 237);
a combined action on both receptors (patients 197, 213 and 223).
Fig. 3.
(a) Immunoblotting of T. cruzi epimastigotes lysate with the IgG fractions of the eight patients that were selected to purify anti-R13 antibodies. (b) Chronotropic effect of total IgG fractions of eight patients with high anti-R13 antibodies levels. Effect of the IgG fraction ( ), as well as antagonizing effects of 10 µm atropine (□) and 1 µm bisoprolol (
), as well as antagonizing effects of 10 µm atropine (□) and 1 µm bisoprolol ( ) were evaluated. (c) Immunoblotting of T. cruzi epimastigote lysate with the eight purified anti-R13 antibodies. The monoclonal antibody mAb17·2 was used as positive control. Arrows indicate the position of the T. cruzi ribosomal P0 protein and the low molecular weight ribosomal P proteins (TcP1, TcP2α and TcP2β) (d) Chronotropic effect of the corresponding immunopurified purified anti-R13 antibodies (
) were evaluated. (c) Immunoblotting of T. cruzi epimastigote lysate with the eight purified anti-R13 antibodies. The monoclonal antibody mAb17·2 was used as positive control. Arrows indicate the position of the T. cruzi ribosomal P0 protein and the low molecular weight ribosomal P proteins (TcP1, TcP2α and TcP2β) (d) Chronotropic effect of the corresponding immunopurified purified anti-R13 antibodies ( ). Bars represent mean ± SD of the change in beats/min; *significant differences (P < 0·001) with respect to the preceding bar.
). Bars represent mean ± SD of the change in beats/min; *significant differences (P < 0·001) with respect to the preceding bar.
One out of the eight patients exerted no functional effect in our system even though the serum levels of anti-R13 antibodies were high. The reactivities of the immunopurified anti-R13 antibodies are shown in Fig. 3c. They are clearly monospecific, reacting only with the low molecular weight T. cruzi ribosomal P proteins TcP1 and TcP2α and β, which share the same C-terminal region, and display a reactive profile similar to that of the anti-R13 monoclonal antibody, mAb17·2 (first lane in Fig. 3c). The monospecific nature of the anti-R13 antibodies was further confirmed by preincubation with the R13 peptide that completely abolished their reactivity against the parasite ribosomal P proteins (not shown).
The functional activities of the anti-R13 antibodies are shown in Fig. 3d. Anti-R13 antibodies from IgG fractions with an exclusive M2-ChR effect were only functional in recognizing the M2-ChR, whereas those isolated from IgG fractions with pure antiβ1-AR reactivity only reacted with the β1-AR receptor. However, IgG fractions with a combined functional effect, obtained for patients 197, 213 and 223, presented anti-R13 antibodies reacting either with one or with the other receptor, but not with both. For example, purified anti-R13 antibodies from patient 223 displayed a β1-AR effect, whereas antibodies from patients 197 and 213 only stimulated the M2-ChR receptor.
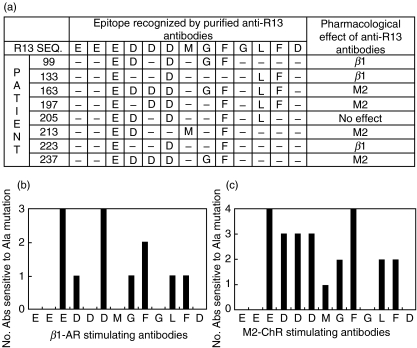
Epitope mapping and fine specificity of human anti-R13 polyclonal antibodies
To evaluate the importance of each amino acid as to the reactive properties of the R13 peptide, we used the alanine mutation scanning technique. As shown in Fig. 4a, the pattern of recognition of the different amino acids turned out to be unique for each patient. The only common element required for recognition of the R13 peptide was the Glu residue at position 3. This result explains the low affinity of the anti-R13 antibodies for the peptide that encompasses the C-teminal region of the human ribosomal protein, EESDDDMGFGLFD, peptide H13.
Fig. 4.
(a) Comparison of the R13 epitope recognized by the different immunopurified anti-R13 antibodies. Each amino acid of R13 was replaced in turn to alanine with the Spots® method (Materials and Methods) and the anti-R13 reactivity was evaluated. In the table, amino acids essential for recognition are represented with the corresponding letters whereas residues nonessential for recognition are symbolized with –. †The pharmacological effect of each purified antibody as evaluated in Fig. 3 is detailed for comparison; β1, β1-AR stimulating effect; M2, M2-ChR stimulating effect. (b,c) Number of antibodies sensitive to alanine mutation evaluated as the number of anti-R13- antibodies with β1-AR (b), or M2-ChR receptor (c) stimulating properties, that fail to recognize R13 when substituted by alanine at the corresponding position. Abs, antibodies.
To test the relevance of the charge of the residue at position 3, we decided to assess the reactivity of a phosphorilated analogue of peptide H13. Accordingly, the ability of the Ser3-phosphorilated peptide (pH13) to compete IgG binding to R13 was determined in ELISA competition assays and compared to the competitive effect of peptide R13 and H13. As it is shown in Table 1, the pH13 peptide was more effective in inhibiting the binding of anti-R13 antibodies to R13 than the H13 peptide, demonstrating the strong influence of a negative charge in the performance of pH13, and stressing the overall importance of the highly charged Glu residue in position 3 of R13.
Table 1.
Equilibrium binding constants estimated as Ki of immunopurified anti-R13 antibodies from the different patients for peptides R13, pH13 and H13. Inhibition constants were calculated as indicated in Materials and Methods
| Patient no. | Ki R13 (m−1) | Ki pH13 (m−1) | Ki H13 (m−1) |
|---|---|---|---|
| 99 | 2·3 × 107 | 5·2 × 106 | 2·5 × 105 |
| 133 | 2·9 × 107 | 3·4 × 106 | 2·3 × 105 |
| 163 | 2·4 × 107 | 1·6 × 106 | 2·2 × 105 |
| 197 | 1·3 × 107 | 8·9 × 105 | 5·9 × 104 |
| 205 | 1·6 × 107 | 6·9 × 105 | 3·1 × 104 |
| 213 | 2·4 × 107 | 2·3 × 106 | 3·1 × 105 |
| 223 | 1·1 × 107 | 4·5 × 105 | 3·3 × 104 |
| 237 | 1·0 × 107 | 7·6 × 105 | 6·4 × 104 |
Analysis of the results depicted in Fig. 4b indicates that anti-R13 antibodies with β1-AR stimulating activity fail to recognize Asp5 and Met7. On the contrary, three out of four anti-R13 antibody preparations that stimulate the M2-ChR do react with Asp5. It is noteworthy that the only anti-R13 preparation that presents cholinergic effect, but does not react with Asp5, does recognize Met7. Although the number of antibody preparations in this study is extremely small to draw conclusive interpretations, these results do point to the fact that very subtle differences in the recognition of R13 determine the functional properties of the anti-R13 antibodies.
DISCUSSION
Anti-autonomic GPCR antibodies might play a role in the pathogenesis of the complex and severe heart disease symptoms commonly found in cChHD patients, not only inducing electrical disorders, but most probably interfering with the electrophysiological properties of cardiac tissues, ultimately causing damage to myocardial cells. The correlation we found between both the presence of β1-AR stimulating antibodies and the incidence of ventricular arrhythmias and the occurrence of M2-ChR stimulating antibodies and sinus node dysfunction strengthens this hypothesis (Fig. 1b). Interestingly, costimulation of both β1-AR and M2-ChR by IgG of patients with cChHD associates with the bradychardic syndrome, result that may be explained by the fact that even in the presence of sympathetic activity, the same level of vagal stimulation exerts a prominent negative inotropic effect on ventricular myocardium [26].
Our present study, together with previous results, sheds light on the origin of anticardiac receptor antibodies in cChHD: they probably originate by a mechanism of molecular mimicry, implying a primary humoral response against the parasite, which has a bystander effect on self structures. This hypothesis is supported by the fact that anti-R13 antibodies bind with very high affinity to the R13 peptide. In our case, antibodies originated against the C-terminus of T. cruzi ribosomal P proteins are also able to recognize the cardiac receptors. In this sense, it is remarkable that patients with the severest form of cChHD possess the highest levels of anti-R13 antibodies (Fig. 2b).
Previous studies had focused on the effect of IgG fractions from cChHD patients with ventricular arrhythmias. In those cases, evidence of cross-reactivity between a β1-AR epitope on its second extracellular loop and peptide R13 were determined [12]. Our results herein demonstrate that human polyclonal anti-R13 antibodies are also able to stimulate the M2-ChR. It is noteworthy that the purified anti-R13 antibodies displayed either a β1-AR or M2-ChR stimulating activity, even in patients with IgG presenting a combined β1-AR/M2-ChR stimulating effect. This observation is the first one describing antibodies against the same epitope, R13, that have different functional specificities, cross-reacting with two different receptors on cardiomyocytes. The probable existence of multiple conformations on the R13 peptide due to its highly charged nature and mobility [27] may explain the generation of different anti-R13 specificities.
Previous studies performed on a monoclonal anti-R13 antibody [14] and on a human polyclonal anti-R13 antibody [12] confirmed the acidic nature of the recognized epitope. The results of alanine-mutation scanning experiments on the R13 epitope using the different immunopurified anti-R13 antibodies illustrates the complexity of the anti-R13 humoral response since each of the eight anti-R13 antibody preparations presented a unique epitope recognition pattern (Fig. 4). Despite this extreme heterogeneity, we were however, able to determine a common reactivity profile where Glu3, and to a lesser extent, Asp6 and Phe9 were predominantly recognized (Fig. 4a). These residues are also included in the epitope recognized by the anti-R13 mAb17·2 [14]. In fact, the substitution of Glu3 into Ser generates the C-terminal end of the human ribosomal P protein, peptide H13, a change that lowers about two orders of magnitude the affinity for the peptide. The importance of the intact poly anionic stretch in the induction of anti-R13 antibodies was confirmed by competition experiments using a Ser3-phosphorylated H13 peptide (pH13), for which binding affinities improved one order of magnitude as compared to H13 (Table 1). These results are in agreement with plasmon resonance studies on the mAb17·2 which demonstrate that its affinity for R13 was 5 times higher than for H13 [14].
Our studies indicate that the anti-R13 response is a component of the humoral response against T. cruzi (Fig. 3a,c). On the other hand, it is of relevance that the functional reactivity of the studied anti-R13 antibodies was always in agreement with the functional properties of the total IgG fraction from which they derive. No anti-R13 antibodies with anti-M2-ChR reactivity were isolated from an IgG fraction with an exclusive β1-AR activity or vice versa, and when the IgG fraction had no functional activity, the corresponding anti-R13 antibodies did not elicit effects on heart cells (patient no. 205, Figs 3b,d).
Since increased anti-R13 antibody levels correlate with the severity of cChHD and R13 is an immunodominant epitope in this disease, it is tempting to hypothesize that an immuno-adsorptive treatment [28] directed to clear functional anti-R13 antibodies from circulating blood, accompanied by antiparasitic chemotherapy [29] may ameliorate the clinical status of anti-R13 positive patients chronically infected by T. cruzi.
Acknowledgments
We would like to thank Dr Gabriela Levitus for helpful assistance. This research has been supported financially by the Argentine National Council for Science and Technology (CONICET), the National Agency of Scientific and Technological Promotion (FONCYT BID1201/OC-AR, PICT 05–06802), the World Health Organization/Special Program for Research and Training in Tropical Diseases and the CNRS-CONICET International Cooperation Program. The work of MJL is partially supported by an International Research Grant of the Howard Hughes Medical Institute (Chevy Chase, MD, USA).
References
- 1.Elizari MV, Chiale PA. Cardiac arrhythmias in Chagas’ heart disease. J Cardiovasc Electrophysiol. 1993;4:596–608. doi: 10.1111/j.1540-8167.1993.tb01247.x. [DOI] [PubMed] [Google Scholar]
- 2.Rassi A, Lorga AM, Rassi SG. Diagnostic and therapeutic approach of the chronic Chagas-related cardiopathy. In: Germiniani H, editor. Diagnosis and Treatment of Cardiac Arrhythmias. 3. Rio de Janeiro: Guanabara Koogan S.A.; 1990. pp. 225–44. [Google Scholar]
- 3.Halperin C, Rassi S. Clinical Relevance of Invasive Electrophysiologic Studies in Patients with Chagas’ Disease. In: Armonk NY, editor. Arrhythmia Management in Chagas’ Disease. Futura Publishing Co Inc.; 2000. pp. 83–93. [Google Scholar]
- 4.Rosenbaum MB, Chiale PA, Schejtman D, Levin M, Elizari MV. Antibodies to beta-adrenergic receptors disclosing agonist-like properties in idiopathic dilated cardiomyopathy and Chagas’ heart disease. J Cardiovasc Electrophysiol. 1994;5:367–75. doi: 10.1111/j.1540-8167.1994.tb01174.x. [DOI] [PubMed] [Google Scholar]
- 5.Goin JC, Borda E, Leiros CP, Storino R, Sterin-Borda L. Identification of antibodies with muscarinic cholinergic activity in human Chagas’ disease: pathological implications. J Auton Nerv Syst. 1994;47:45–52. doi: 10.1016/0165-1838(94)90064-7. [DOI] [PubMed] [Google Scholar]
- 6.Elies R, Ferrari I, Wallukat G, et al. Structural and functional analysis of the B cell epitopes recognized by anti-receptor autoantibodies in patients with Chagas’ disease. J Immunol. 1996;157:4203–11. [PubMed] [Google Scholar]
- 7.Chiale PA, Ferrari I, Mahler E, Vallazza MA, Elizari MV, Rosenbaum MR, Levin MJ. Differential profile and biochemical effects of antiautonomic membrane receptor antibodies in ventricular arrhythmias and sinus node dysfunction. Circulation. 2001;103:1765–71. doi: 10.1161/01.cir.103.13.1765. [DOI] [PubMed] [Google Scholar]
- 8.Ferrari I, Levin MJ, Wallukat G, et al. Molecular mimicry between the immunodominant ribosomal P0 protein of Trypanosoma cruzi and a functional epitope on the human β-adrenergic receptor. J Exp Med. 1995;182:59–65. doi: 10.1084/jem.182.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mijares A, Verdot L, Peineau N, Vray B, Hoebeke J, Argibay J. Antibodies from Trypanosoma cruzi infected mice recognize the second extracellular loop of the β1-adrenergic and M2-muscarinic receptors and regulate calcium channels in isolated cardiomyocytes. Mol Cell Biochem. 1996;163–164:107–12. doi: 10.1007/BF00408646. [DOI] [PubMed] [Google Scholar]
- 10.Sterin-Borda L, Gorelik G, Borda ES. Chagasic IgG binding with cardiac muscarinic cholinergic receptors modifies cholinergic-mediated cellular transmembrane signals. Clin Immunol Immunopathol. 1991;61:387–97. doi: 10.1016/s0090-1229(05)80010-8. [DOI] [PubMed] [Google Scholar]
- 11.De Oliveira SF, Pedrosa RC, Nascimento JH, Campos de Carvalho AC, Masuda MO. Sera from chronic chagasic patients with complex cardiac arrhythmias depress electrogenesis and conduction in isolated rabbit hearts. Circulation. 1997;96:2031–7. doi: 10.1161/01.cir.96.6.2031. [DOI] [PubMed] [Google Scholar]
- 12.Kaplan D, Ferrari I, Lopez-Bergami P, et al. Antibodies to ribosomal P proteins of Trypanosoma cruzi in Chagas’ disease possess functional autoreactivity with heart tissue and differ from anti-P autoantibodies in lupus. Proc Natl Acad Sci USA. 1997;94:10301–6. doi: 10.1073/pnas.94.19.10301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lopez Bergami P, Scaglione J, Levin MJ. Antibodies against the carboxyl-terminal end of the Trypanosoma cruzi ribosomal P proteins are pathogenic. FASEB J. 2001;15:2602–12. doi: 10.1096/fj.01-0132com. [DOI] [PubMed] [Google Scholar]
- 14.Mahler E, Sepulveda P, Jeannequin O, et al. A monoclonal antibody against the immunodominant epitope of the ribosomal P2β protein of Trypanosoma cruzi interacts with the human β1-adrenergic receptor. Eur J Immunol. 2001;31:2210–6. doi: 10.1002/1521-4141(200107)31:7<2210::aid-immu2210>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 15.Ferrari I, Levin MJ, Elizari MV, Rosenbaum MB, Chiale PA. Cholinergic autoantibodies in sinus-node dysfunction. Lancet. 1997;350:262–3. doi: 10.1016/S0140-6736(05)62226-X. [DOI] [PubMed] [Google Scholar]
- 16.WHO/ISFC Task Force. Report on the definition and classification of cardiomyopathies. Br Heart J. 1980;44:672–3. doi: 10.1136/hrt.44.6.672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levin MJ, Vazquez M, Kaplan D, Schijman AG. The Trypanosoma cruzi ribosomal P protein family. Classification Antigenicity Parasitol Today. 1993;9:381–4. doi: 10.1016/0169-4758(93)90088-w. [DOI] [PubMed] [Google Scholar]
- 18.Rich BE, Steitz JA. Human acidic ribosomal proteins P0, P1 and P2: analysis of cDNA clones, in vitro synthesis and assembly. Mol Cell Biol. 1987;7:4065–74. doi: 10.1128/mcb.7.11.4065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lopez Bergami P, Cabeza Meckert P, Kaplan D, et al. Immunization with recombinant Trypanosoma cruzi ribosomal P2β protein induces changes in the electrocardiogram of immunized mice. FEMS Immunol Med Microbiol. 1997;18:75–85. doi: 10.1111/j.1574-695X.1997.tb01030.x. [DOI] [PubMed] [Google Scholar]
- 20.Levitus G, Hontebeyrie-Joskowicz M, Van Regenmortel MH, Levin MJ. Humoral autoimmune response to ribosomal P proteins in chronic Chagas heart disease. Clin Exp Immunol. 1991;85:413–7. doi: 10.1111/j.1365-2249.1991.tb05741.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wallukat G, Wollenberger A. Effects of the serum gamma-globulin fraction of patients with allergic asthma and dilated cardiomyopathy on chronotropic β-adrenoceptor function in cultured neonatal rat heart myocytes. Biomed Biochim Acta. 1987;46:634–9. [PubMed] [Google Scholar]
- 22.Gomez EB, Medina G, Ballesta JP, Levin MJ, Tellez-Inon MT. Acidic ribosomal P proteins are phosphorylated in Trypanosoma cruzi. Int J Parasitol. 2001;31:1032–9. doi: 10.1016/s0020-7519(01)00219-3. [DOI] [PubMed] [Google Scholar]
- 23.Piehler J, Brecht A, Giersch T, Hock B, Gauglitz G. Assessment of affinity constants by rapid solid phase detection of equilibrium binding in a flow system. J Immunol Meth. 1997;201:189–206. doi: 10.1016/s0022-1759(96)00222-0. [DOI] [PubMed] [Google Scholar]
- 24.Levin MJ, Mestri EA, Benarous R, et al. Identification of major Trypanosoma cruzi antigenic determinants in chronic Chagas’ heart disease. Am J Trop Med Hyg. 1989;41:530–8. doi: 10.4269/ajtmh.1989.41.530. [DOI] [PubMed] [Google Scholar]
- 25.Levitus G, Grippo V, Labovsky V, Ghio S, Hontebeyrie M, Levin MJ. DNA immunization with the ribosomal P2β gene of Trypanosoma cruzi fails to induce pathogenic antibodies. Microbes and Infection. 2003;5:1381–8. doi: 10.1016/j.micinf.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 26.Levy MN. Cardiac sympathetic–parasympathetic interactions. Fed Proc. 1984;43:2598–602. [PubMed] [Google Scholar]
- 27.Zurdo J, Sanz JM, Gonzalez C, Rico M, Ballesta JP. The exchangeable yeast ribosomal acidic protein YP2β shows characteristics of a partly folded state under physiological conditions. Biochemistry. 1997;36:9625–35. doi: 10.1021/bi9702400. [DOI] [PubMed] [Google Scholar]
- 28.Wallukat G, Muller J, Hetzer R. Specific removal of β1-adrenergic autoantibodies from patients with idiopathic dilated cardiomyopathy. N Engl J Med. 2002;347:1806. doi: 10.1056/NEJM200211283472220. [DOI] [PubMed] [Google Scholar]
- 29.Apt W, Arribada A, Zulantay I, Sanchez G, Vargas SL, Rodriguez J. Itraconazole or allopurinol in the treatment of chronic American trypanosomiasis: the regression and prevention of electrocardiographic abnormalities during 9 years of follow-up. Ann Trop Med Parasitol. 2003;97:23–9. doi: 10.1179/000349803125002751. [DOI] [PubMed] [Google Scholar]