It is over 100 years since the use of oxygen to relieve angina pectoris was first described by Steele.1 More importantly, it is over 50 years since Russek and colleagues cautioned that the administration of 100% oxygen may actually be contraindicated in patients with myocardial infarction or angina pectoris in whom the arterial oxygen saturation is normal.2 Since this warning, there have been numerous reports of potentially harmful effects of high flow oxygen in the treatment of myocardial infarction, yet it is routine clinical practice to administer oxygen to virtually all patients in this situation. In this essay we have considered, from an historical perspective, the findings from the key studies of the effects of oxygen therapy in patients with myocardial infarction. We propose that randomized controlled trials are urgently required.
In their original study, published in JAMA in 1950, Russek and colleagues observed that 100% oxygen via a face mask led to more pronounced and longer duration of the electrocardiograph (ECG) manifestations of myocardial ischemia and failed to prevent the onset or influence the duration of anginal pain.2 These observations led the authors to suggest that the administration of 100% oxygen may actually be contraindicated in patients in whom arterial oxygen saturation is normal, and to hypothesize that hyperoxygenated blood may interfere with the reactive hyperaemia which accompanies an ischaemic myocardium. They stressed that oxygen should be freely administered if indicated (i.e. for relief of hypoxia with pulmonary oedema and Cheyne-Stokes respiration) but that ‘its indiscriminate employment may result in more harm than good.’ These observations contrasted with the pragmatic but unproven medical view of the period that the administration of high flow oxygen was an important therapeutic measure, regardless of arterial hypoxia, on the basis that it increased the oxygen supply to the myocardium and reduced the size of the infarct.3,4
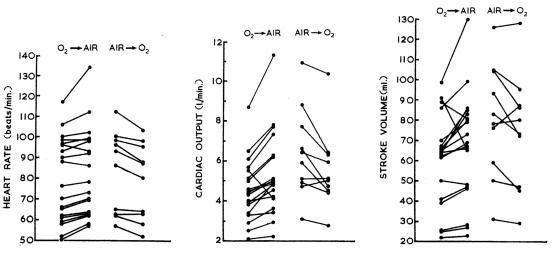
The haemodynamic effects of high flow oxygen in the setting of myocardial infarction were explored by a number of groups in the 1960s. In 1965, Thomas and colleagues reported that in the first few days following myocardial infarction administration of 40% oxygen for 20 minutes resulted in a rise in the arterial blood pressure and fall in cardiac output (Figure 1).5 Similarly, high flow oxygen caused a fall in cardiac output in patients with left ventricular failure and a baseline arterial oxygen saturation of ≥90%.6 The cardiovascular response to high flow oxygen was attributed primarily to arterial vasoconstriction, which had been demonstrated in retinal blood vessels.7 This mechanism was also thought to explain the reduction in cerebral blood flow8 and renal blood flow9 with oxygen therapy.
Figure 1.
Measurements of heart rate, cardiac output and stroke volume made before and after changing the inspired gas from 40% oxygen to air, and from air to 40% oxygen in patients who had recently experienced a myocardial infarction. Reproduced with permission from Thomas et al.5
In 1968 Kenmure and colleagues confirmed that, in subjects with myocardial infarction, high flow oxygen reduced cardiac output and stroke volume and increased the mean arterial pressure and systemic vascular resistance.10 In a contemporaneous clinical trial, Foster and colleagues did not demonstrate a fall in cardiac output when increasing concentrations of oxygen were given to patients with myocardial infarction, although arterial pressure and systemic vascular resistance increased progressively as arterial oxygen tension increased.11
The importance of the degree of underlying arterial hypoxia in determining the effect of oxygen therapy following myocardial infarction was demonstrated by Sukumalchantra and colleagues in 1969.12 They demonstrated that oxygen did not increase oxygen transport in patients with arterial oxygen saturations >90% because of reductions in cardiac output in excess of increases in oxygen content. In contrast, in patients with arterial oxygen saturations <90%, oxygen administration increased oxygen transport due to both increased cardiac output and oxygen content.
Also at that time, Neill demonstrated—through measurement of the lactate/pyruvate concentration ratio in coronary venous blood—that hypoxia did not affect the availability of oxygen for myocardial metabolism in normal subjects until the oxygen saturation fell to about 50%.13 However, in subjects with coronary artery disease, anaerobic metabolism indicative of myocardial ischemia was observed in some patients with saturations between 70 and 85%. In this study, there was no evidence that hyperoxia augmented myocardial oxygen availability or relieved myocardial ischemia in patients with coronary artery disease. These novel observations provided insight into the complex interactions between the level of arterial oxygen saturation and the presence of local coronary artery obstruction in determining whether myocardial ischaemia occurs.
In similar experiments, Bourassa and colleagues14 extended these observations by reporting that in patients with severe triple vessel disease, abnormal lactate changes were produced or accentuated during the administration of 100% oxygen. These authors concluded that high flow oxygen can reduce coronary blood flow sufficiently to cause myocardial ischemia in patients with severe coronary artery disease.
In the 1970s there were two studies indicating benefit with the use of oxygen in the situation of angina or myocardial infarction. In 1972 Horvat et al. reported that the threshold to pacing-induced angina improved with oxygen therapy,15 although a similar benefit could not be demonstrated with exercise-induced angina.16 In 1976 Madias and colleagues suggested that the administration of oxygen therapy to patients experiencing a myocardial infarction may reduce ischaemic injury, based on precordial ST segment mapping.17 This represents the major clinical evidence for the benefit of oxygen therapy in myocardial infarction, and for this reason the study needs to be considered in detail. Unfortunately, the lack of a randomized controlled design, standardization of duration of oxygen therapy or blinding in the ST measurements limits the significance of their findings. Furthermore, there was no correlation between the ST changes and the age of the infarct, duration of exposure to oxygen inhalation, levels of PaO2, or initial ST measurements. As a result, the Madias et al. study should be considered to provide only moderate evidence at best of a benefit with oxygen therapy and apply only to Q wave myocardial infarction.
It was not until 1976 that Rawles and Kenmure18 undertook the first randomized, double-blind, controlled trial of oxygen therapy in the first 24 hours of uncomplicated myocardial infarction. The group receiving oxygen via an MC mask at a flow rate of 6 litres per minute for the initial 24 hour period had a higher serum aspartate aminotransferase level than the group receiving room air, indicating greater myocardial damage. In the group receiving oxygen, 9/80 (11.3%) died compared to 3/77 (3.9%) in the control group. The relative risk of mortality in the oxygen group was 2.9 (95% CI 0.81-10.3; P=0.08). While this difference did not reach traditional levels of statistical significance, there was clearly the possibility of a substantial type II error rate. Indeed, based on a 95% CI for a difference in proportions, the number needed to cause a death could have been as small as 6.5 for oxygen therapy. Conversely, these findings provided no support for the view that oxygen therapy was either beneficial or safe in terms of either the size of the myocardial infarction or mortality rate, which would have been necessary to justify the use of a therapeutic intervention (i.e. first do no harm). These findings assume greater significance as there have been no further placebo-controlled randomized double-blind trials of oxygen therapy in myocardial infarction.
The 1980s and 1990s were dominated by trials of pharmacological agents in myocardial infarction and unstable angina, including thrombolysis, aspirin, heparin, beta blockade, calcium antagonists, angiotensin-converting enzyme inhibitors, nitrates and magnesium. However, during this period, there were a number of studies which raised further concerns about the use of high flow oxygen in other related clinical situations. For example, in critically ill patients, high flow oxygen was shown to reduce whole body oxygen uptake, indicating a mal-distribution of blood flow and functional oxygen shunting to protect tissue from the non-physiological effects of high flow oxygen.19 In congestive heart failure, high flow oxygen was shown to have a detrimental effect on cardiac function, leading the authors to caution against the use of oxygen in the absence of substantial arterial desaturation.20
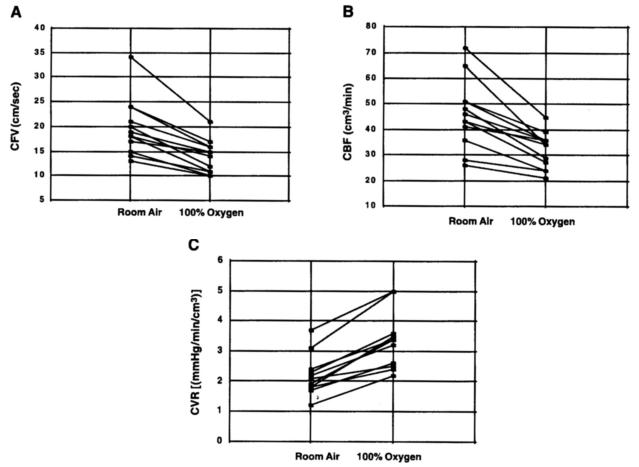
More recently, in 2005 McNulty and colleagues provided direct evidence that the administration of high flow oxygen reduces coronary artery blood flow in stable patients with ischaemic heart disease (Figures 2 and 3).21 As a result, the indirect evidence for such an effect that was provided over 35 years ago14 has now been confirmed utilizing the latest advances in technology: the methods may change, but the effects of oxygen on the heart remain the same.
Figure 2.
The coronary flow velocity (CFV; A), coronary blood flow (CBF; B) and coronary vascular resistance (CVR; C) in subjects during sequential room air and 100% oxygen breathing. Reproduced with permission from McNulty et al.21
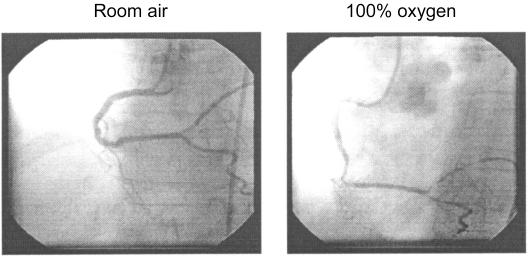
Figure 3.
Right coronary angiogram performed in a subject during intracoronary infusion of acetylcholine while breathing room air (left) and 100% oxygen (right). The diffuse constriction of the distal coronary artery branches while breathing 100% oxygen is evident. Reproduced with permission from McNulty et al.21
We suggest that the current practice of oxygen administration in the setting of myocardial infarction is not based on the key studies which appear to have been buried deep in history. We recommend that randomized controlled trials of the use of oxygen therapy in myocardial infarction are urgently required.
Competing interests None declared.
Funding None sought or received.
Ethical approval Not required.
Guarantor Richard Beasley accepts full responsibility for the essay, the interpretation of the data, and controlled the decision to publish.
Contributorship Richard Beasley developed the concept of the essay, undertook the literature search and reviewed the articles, and took primary responsibility for writing the manuscript. Sarah Aldington and Geoffrey Robinson reviewed the articles identified by the literature search and contributed to the drafting of the manuscript. Mark Weatherall undertook the statistical analysis of the Rawles and Kenmure RCT. David McHaffie provided specialist cardiology review of the essay.
References
- 1.Steele C. Severe angina pectoris relieved by oxygen inhalations. BMJ 1900;2: 1568 [Google Scholar]
- 2.Russek HI, Regan FD, Naegele CF. One hundred percent oxygen in the treatment of acute myocardial infarction and severe angina pectoris. JAMA 1950;144: 373-5 [DOI] [PubMed] [Google Scholar]
- 3.Boland EW. Oxygen in high concentrations for relief of pain in coronary thrombosis and severe angina pectoris. JAMA 1940;114: 1512 [Google Scholar]
- 4.Boothby WM, Mayo CW, Lovelace WR Jr. One hundred percent oxygen: indications for its use and methods of its administration. JAMA 1939;113: 477 [Google Scholar]
- 5.Thomas M, Malmcrona R, Shillingford J. Haemodynamic effects of oxygen in patients with acute myocardial infarction. Brit Heart J 1965;27: 401-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daly WJ, Behnke RH. Hemodynamic consequences of oxygen breathing in left ventricular failure. Circulation 1963;27: 252-6 [DOI] [PubMed] [Google Scholar]
- 7.Dollery CT, Hill DW, Mailer CM, Ramalho PS. High oxygen pressure and the retinal blood vessels. Lancet 1964;2: 291-2 [DOI] [PubMed] [Google Scholar]
- 8.Kety SS, Schmidt CF. The effects of altered arterial tensions of carbon dioxide and oxygen on cerebral blood flow and cerebral oxygen consumption in normal young men. J Clin Invest 1948;27: 484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aber GM, Harris AM, Bishop JM. The effect of acute changes in inspired oxygen concentration on cardiac, respiratory and renal function in patients with chronic obstructive airways disease. Clin Sci 1964;26: 133-43 [PubMed] [Google Scholar]
- 10.Kenmure ACF, Murdoch WR, Beattie AD, Marshall JCB, Cameron AJV. Circulatory and metabolic effects of oxygen in myocardial infarction. Brit Med J 1968;4: 360-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Foster GL, Casten GG, Reeves TJ. The effects of oxygen breathing in patients with acute myocardial infarction. Cardiovasc Res 1969;3: 179-89 [DOI] [PubMed] [Google Scholar]
- 12.Sukumalchantra Y, Levy S, Danzig R, Rubins S, Alpern H, Swan HJC. Correcting arterial hypoxemia by oxygen therapy in patients with acute myocardial infarction. Am J Cardiol 1969;24: 838-52 [DOI] [PubMed] [Google Scholar]
- 13.Neill WA. Effects of arterial hypoxemia and hyperoxia on oxygen availability for myocardial metabolism: patients with and without coronary heart disease. Am J Cardiol 1969;24: 166-71 [DOI] [PubMed] [Google Scholar]
- 14.Bourassa MG, Campeau L, Bois MA, Rico O. The effects of inhalation of 100 per cent oxygen on myocardial lactate metabolism in coronary heart disease. Am J Cardiol 1969;24: 172-7 [DOI] [PubMed] [Google Scholar]
- 15.Horvat M, Yoshida S, Prakash R, Marcus HS, Swan HJC, Ganz W. Effect of oxygen breathing on pacing-induced angina pectoris and other manifestations of coronary insufficiency. Circulation 1972;45: 837-44 [DOI] [PubMed] [Google Scholar]
- 16.Lecerof H. Central haemodynamics during oxygen breathing in angina pectoris. Thorax 1974;29: 673-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Madias JE, Madias NE, Hood WB. Precordial ST-segment mapping: 2. Effects of oxygen inhalation on ischemic injury in patients with acute myocardial infarction. Circulation 1976;53: 411-7 [DOI] [PubMed] [Google Scholar]
- 18.Rawles JM, Kenmure ACF. Controlled trial of oxygen in uncomplicated myocardial infarction. BMJ 1976;1: 1121-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reinhart K, Bloos F, Konig F, Bredle D, Hannemann L. Reversible decrease of oxygen consumption by hyperoxia. Chest 1991;99: 690-4 [DOI] [PubMed] [Google Scholar]
- 20.Haque WA, Boehmer J, Clemson BS, Leuenberger UA, Silber DH, Sinoway LI. Hemodynamic effects of supplemental oxygen administration in congestive heart failure. J Am Coll Cardiol 1996;27: 353-7 [DOI] [PubMed] [Google Scholar]
- 21.McNulty PH, King N, Scott S et al. Effects of supplemental oxygen administration on coronary blood flow in patients undergoing cardiac catheterization. Am J Physiol Heart Circ Physiol 2005;288: H1057-H1062 [DOI] [PubMed] [Google Scholar]